Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm (IPMN) is a type of tumor that can occur within the cells of the pancreatic duct. IPMN tumors produce mucus,[1] and this mucus can form pancreatic cysts.[2] Although intraductal papillary mucinous neoplasms are benign tumors, they can progress to pancreatic cancer.[1] As such IPMN is viewed as a precancerous condition.[3] Once an intraductal papillary mucinous neoplasm has been found, the management options include close monitoring and pre-emptive surgery.
| Intraductal papillary mucinous neoplasm | |
|---|---|
 | |
| Intraductal papillary mucinous neoplasm in magnetic resonance imaging. |
Diagnosis
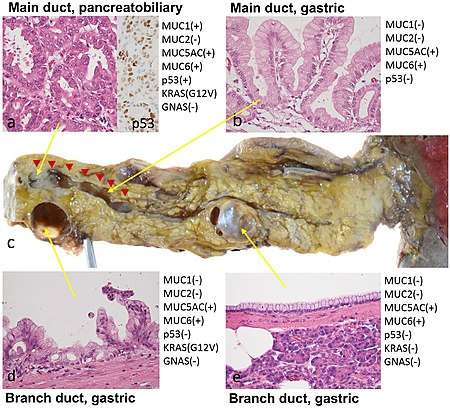
By histopathology, IPMN is characterized on light microscopy by Mucinous epithelial cells,[4] and growth within the pancreatic ducts.[5] Mucin 5AC is a useful immunohistochemistry marker.[6] !! Microscopy findings[6] !! Micrograph !! Immunohistochemistry markers[6] Characteristic genetic alterations are those of KRAS and GNAS.[6]
Further subtyping of IPMN can be done as either:[7]
- Gross pathology: Main duct versus branch duct lesions, which determines surgical management
- By light microscopy and immunohistochemistry:[8] Gastric, intestinal, pancreaticbiliary, and oncocytic.
Treatment
The treatment of choice for main-duct IPMNs is resection due to approximately 50% chance of malignancy. Side-branch IPMNs are occasionally monitored with regular CT or MRIs, but most are eventually resected, with a 30% rate of malignancy in these resected tumors. Survival 5 years after resection of an IPMN without malignancy is approximately 80%, 85% with malignancy but no lymph node spread and 0% with malignancy spreading to lymph nodes.[10] Surgery can include the removal of the head of the pancreas (a pancreaticoduodenectomy), removal of the body and tail of the pancreas (a distal pancreatectomy), or rarely removal of the entire pancreas (a total pancreatectomy).[11] In selected cases the surgery can be performed using minimally invasive techniques such as laparoscopy[12] or robotic surgery. A study using Surveillance, Epidemiology, and End Result Registry (SEER) data suggested that increased lymph node counts harvested during the surgery were associated with better survival in invasive IPMN patients.[13]
History
In 1982, IPMN was reported as a "mucin-producing tumor" by Kazuhiko Ohashi of the Japanese Foundation for Cancer Research.
See also
- Pancreatic serous cystadenoma
- Solid pseudopapillary neoplasm
References
- "Intraductal Papillary Mucinous Neoplasms of the Pancreas". Johns Hopkins University. Retrieved 7 September 2009.
- Campbell, NM; Katz, SS; Escalon, JG; Do, RK (March 2015). "Imaging patterns of intraductal papillary mucinous neoplasms of the pancreas: an illustrated discussion of the International Consensus Guidelines for the Management of IPMN". Abdominal Imaging. 40 (3): 663–77. doi:10.1007/s00261-014-0236-4. PMID 25219664.
- "Precancerous conditions of the pancreas - Canadian Cancer Society". www.cancer.ca. Retrieved 5 November 2017.
- Diana Agostini-Vulaj. "Pancreas - Exocrine tumors / carcinomas - Intraductal papillary mucinous neoplasm (IPMN)". Pathology Outlines. Topic Completed: 1 July 2018. Revised: 9 March 2020
- Adsay, Volkan; Mino-Kenudson, Mari; Furukawa, Toru; Basturk, Olca; Zamboni, Giuseppe; Marchegiani, Giovanni; Bassi, Claudio; Salvia, Roberto; Malleo, Giuseppe; Paiella, Salvatore; Wolfgang, Christopher L.; Matthaei, Hanno; Offerhaus, G. Johan; Adham, Mustapha; Bruno, Marco J.; Reid, Michelle D.; Krasinskas, Alyssa; Klöppel, Günter; Ohike, Nobuyuki; Tajiri, Takuma; Jang, Kee-Taek; Roa, Juan Carlos; Allen, Peter; Castillo, Carlos Fernández-del; Jang, Jin-Young; Klimstra, David S.; Hruban, Ralph H. (2016). "Pathologic Evaluation and Reporting of Intraductal Papillary Mucinous Neoplasms of the Pancreas and Other Tumoral Intraepithelial Neoplasms of Pancreatobiliary Tract". Annals of Surgery. 263 (1): 162–177. doi:10.1097/SLA.0000000000001173. ISSN 0003-4932. PMC 4568174.
- Pishvaian MJ, Brody JR (2017). "Therapeutic Implications of Molecular Subtyping for Pancreatic Cancer". Oncology (Williston Park). 31 (3): 159–66, 168. PMID 28299752.
- Salvia, Roberto (2010). "Differences between main-duct and branch-duct intraductal papillary mucinous neoplasms of the pancreas". World Journal of Gastrointestinal Surgery. 2 (10): 342. doi:10.4240/wjgs.v2.i10.342. ISSN 1948-9366.
- Ishida, Masaharu; Egawa, Shinichi; Aoki, Takeshi; Sakata, Naoaki; Mikami, Yukio; Motoi, Fuyuhiko; Abe, Tadayoshi; Fukuyama, Shoji; Sunamura, Makoto; Unno, Michiaki; Moriya, Takuya; Horii, Akira; Furukawa, Toru (2007). "Characteristic Clinicopathological Features of the Types of Intraductal Papillary-Mucinous Neoplasms of the Pancreas". Pancreas. 35 (4): 348–352. doi:10.1097/mpa.0b013e31806da090. ISSN 0885-3177.
- Shibata, Hideki; Ohike, Nobuyuki; Norose, Tomoko; Isobe, Tomohide; Suzuki, Reika; Imai, Hideyuki; Shiokawa, Akira; Takimoto, Masafumi; Tabuchi, Akihiro; Takano, Yuichi; Yamamura, Eiichi; Nagahama, Masatsugu; Takeyama, Nobuyuki; Yokomizo, Kazuaki; Mizukami, Hiroki; Tanaka, Jun-ichi; Aoki, Takeshi; Murakami, Masahiko (2017). "A resected case of two branch duct-type intraductal papillary mucinous neoplasms showing different clinical courses after a two-year follow-up". Clinical Journal of Gastroenterology. 10 (3): 274–278. doi:10.1007/s12328-017-0728-1. ISSN 1865-7257.-
"This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/)" - Sohn, Taylor (June 2004). "Intraductal Papillary Mucinous Neoplasms of the Pancreas". Annals of Surgery. 239 (6): 788–799. doi:10.1097/01.sla.0000128306.90650.aa. PMC 1356287. PMID 15166958.
- "Pancreatic Surgery". Johns Hopkins University. Retrieved 7 September 2009.
- "Laproscopic Pancreatic Surgery". Johns Hopkins University. Retrieved 7 September 2009.
- Wu, WM (Sep 2014). "An increased total resected lymph node count benefits survival following pancreas invasive intraductal papillary mucinous neoplasms resection: an analysis using the surveillance, epidemiology, and end result registry database". PLOS ONE. 9 (9): e107962. doi:10.1371/journal.pone.0107962. PMC 4179272. PMID 25264746.