Healthcare in Tanzania
Tanzania has a hierarchical health system which is in tandem with the political-administrative hierarchy.[1] At the bottom, there are the dispensaries found in every village where the village leaders have a direct influence on its running. The health centers are found at ward level and the health center in charge is answerable to the ward leaders. At the district, there is a district hospital and at the regional level a regional referral hospital. The tertiary level is usually the zone hospitals and at a national level, there is the national hospital. There are also some specialized hospitals that do not fit directly into this hierarchy and therefore are directly linked to the ministry of health.
The government has several key plans and policies guiding healthcare provision and development. The Health Sector Strategic Plan III (2009–15) is guided by the Vision 2015[2] and guides planning for health facilities.[3] The Big Results Now (BRN) was copied from the Malaysian Model of Development and placed health as a key national result area and mainly was for priority setting, focused planning and efficient resource use.[4] There are many other policies aiming at improving the health system and health care provision in Tanzania.
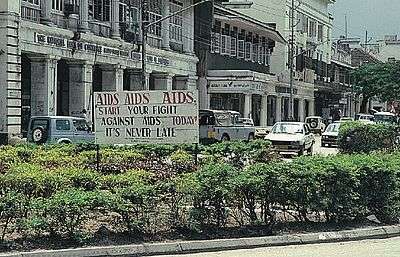
The leading causes of mortality in Tanzania include: HIV 17%, lower respiratory infections 11%, malaria 7%, diarrheal diseases 6%, tuberculosis 5%, cancer 5%, ischemic heart disease 3%, stroke 3%, STDs 3% and sepsis 2%[5] and this shows the double burden of disease the country has to bear.
Health care financing
Health care financing is among the key component of a functional health system.[6] Financing involves three aspects, namely revenue collection, risk pooling, and purchasing.[7] In recent years, there has been a growing demand for access to high-quality and affordable care for all, thus the government is committed to respond with a process of developing health financing strategy[8] is underway since early 2013. An inter-ministerial steering committee has been developed, composed of key ministries and department to ensure that the proposed reforms meet the needs of the population. Improving the prepayment mechanisms are the main agenda in the development of the strategy, which is assumed to be a potential facilitator in the progress towards UHC.
The evolution of health care financing in Tanzania
The Arusha Declaration in 1967 was initiated by the president Julius Nyerere, outlining the principles of Ujamaa (Nyerere vision of social and economic policies) to develop the national economy.[9] It marked the start of a series of health sector reforms with the intention of increasing universal access to social services to the poor and those living in marginalized rural areas. Followed by the Government banning private-for-profit medical practice in 1977[10] and took on the task of providing health services free of charge.
However, by the early 1990s, the strain of providing free health care for all became evident in the face of rising health care costs and a struggling economy. Early 1990s the government adopted health sector reforms that changed the financing system from free services to mixed financing mechanisms including cost sharing policies. Cost sharing in the form of user fees was introduced in four phases: Phase I from July 1993 to June 1994 to referral and some services in regional hospital; Phase II from July 1994 to December 1994 to regional hospital; Phase III from January 1995 onwards to district hospital and Phase IV introduced to health centre and Dispensary after completion of introduction to all district hospital. Exemption and waiver were integral part of the cost sharing policy introduced in 1994.
Health spending
Current data shows in Tanzania there has been an increase in budget allocation for health over the years: Total Health Expendinture (THE) increased from US$734 million in 2002/2003 to US$1.75 billion in 2009/2010 as indicated in the National Health Accounts 2010 report. However donors have been the main financier of health, despite the decrease in their share of health expenditure from 44 percent in 2005/2006 to 40 percent in 2009/2010.[11] (Table 1). Overall, the government allocation for health spending has remained almost constant at about 7 percent since 2002/2003, far away from reaching the Abuja declaration target of 15% of total government expenditure. The increase in donor funding is attributed to the commencement of financing for HIV and AIDS by the Global Fund in 2001 and the commencement of health financing through Sector wide Approach (SWAp)[12] in early 2000.
Table 1: Financing sources as a % of Total Health Expenditure[13]
| 2002/2003 | 2005/2006 | 2009/2010 | |
|---|---|---|---|
| Public | 25.4 | 28.1 | 26 |
| Private | 47.1 | 27.8 | 34.5 |
| Donors | 27.4 | 44.1 | 39.6 |
On the other hand, there has been a commitment to expand the insurance coverage in the country, however the insurance schemes are highly fragmented.[14][15] There are four health insurance schemes which are publicly owned, namely National Health Insurance Fund (NHIF),[16] Social Health Insurance Benefit (SHIB) established as a benefit under the National Social Security Fund (NSSF)[17] and the Community Health Fund (CHF)[18] and Tiba Kwa Kadi (TIKA). Recent statistics shows that there were about 7 private firms as indicated in the Tanzania Insurance Regulatory authority (TIRA)[19] which were providing health insurance per se, while a few of other general insurance firms combine health insurance benefit under life insurance.[20]
National Health Insurance Fund (NHIF)
The NHIF was established by the Act of Parliament No. 8 of 1999 and began its operations in June 2001. The scheme was initially intended to cover public servants but recently there have been provisions which allow private membership.[21] The public formal sector employees pay a mandatory contribution of 3% of their monthly salary and the government as an employer matches the same. This scheme covers the principal member, spouse and up to four below 18 years legal dependants. There has been a steady increase in coverage from 2.0% of the total population in 2001/2002 to 7.1% in 2011.[21]
Social Health Insurance Benefit (SHIB)
Social Health Insurance Benefit (SHIB) is part of the National Social Security Benefits introduced in 2007. All members of NSSF have access to medical care through SHIB after undergoing registration process with only one facility of their choice. The scheme accredits both public and private providers.The benefit is part of their 20% contribution to the NSSF.[22]
Community Health Fund (CHF) and Tiba Kwa Kadi (TIKA)
Community Health Fund is the scheme that targets the largest population in the rural informal sector and membership is voluntary. There is a counterpart called TIKA which mainly targets the informal sector individuals in urban areas. The CHF and TIKA are both regulated under the CHF act 2001 and managed at district level. At the district level, council health service boards (CHSB) and health facilities governing committees (HFGC) are responsible to oversee the operation of CHF and sensitization. In 2009 the National management role of CHF was given to the NHIF.[23]
Private insurance schemes
Strategis[24] was one of the first registered (2002) private health insurance firms in Tanzania. Members of Strategies insurance are corporate employees and become members through their company.
AAR[25] is another private health insurance in Tanzania. The firm started as a health-maintenance organisation (HMO) in 1999 but in 2007 it was re-registered as a private health insurance company.
Jubilee Insurance, Resolution Health and Metropolitan Insurance are other examples of private health insurance firms with more less similar features as strategies and AAR.[26]
Health insurance coverage
Health insurance coverage is still low in Tanzania. As of June 2013 NHIF was estimated to be covering about 6.6% of the population while CHF covers about 7.3% of the population based on 2012 Census. Beneficiaries of NHIF includes the contributing members, spouse and up to four dependants. The CHF beneficiaries include head of household, spouse and all children below 18 years. Other prepayment schemes cover less than 1% of the population. CHF mainly focuses its coverage in rural population while private health insurance schemes target urban population. Low insurance coverage leads to over-reliance on direct payment at the point of use of health care, which is among the fundamental problem that restrain the move towards universal health coverage in many developing countries.[27] Direct payment can lead to high level of inequity, and in most cases denying the poorest access to needed health care.[28]
References
- Manzi, Fatuma; Schellenberg, Joanna Armstrong; Hutton, Guy; Wyss, Kaspar; Mbuya, Conrad; Shirima, Kizito; Mshinda, Hassan; Tanner, Marcel; Schellenberg, David (22 February 2012). "Human resources for health care delivery in Tanzania: a multifaceted problem". Human Resources for Health. 10: 3. doi:10.1186/1478-4491-10-3. PMC 3311084. PMID 22357353.
- http://www.mof.go.tz/mofdocs/overarch/Vision2025.pdf%5B%5D
- , United Republic of Tanzania Ministry of Health and Social Welfare, Health Sector Strategic Plan July 2015- June 2020 Reaching all Households with Quality Healthcare.
- , documents.worldbank.org/curated/en/648601468112497753/Tanzania-Big-Results-Now-for-Health-Project.
- , Global Health- Tanzania Centers for Disease Control and Prevention.
- WHO, World Health Report: Health Syetem Financing: The Path to Universal Coverage. 2010: Geneva
- WHO 2000. Health Systems: Improving performance. Geneva.
- Haazen, Dominic (2012). "Making Health Financing Work for Poor People in Tanzania". World Bank Group Open Knowledge Repository. World Bank Group. Retrieved 5 October 2015.
- Hyden, G. (1980). Beyond Ujamaa in Tanzania: Underdevelopment and an Uncaptured Peasantry. Berkeley and Los Angeles: University of California Press.
- Kolstad, J. R.; Lindkvist, I. (2013). "Pro-social preferences and self-selection into the public health sector: evidence from an economic experiment". Health Policy Plan. 28 (3): 320–327. doi:10.1093/heapol/czs063. PMID 22763126.
- "BTrue - Your Trusted Source of Health Information and News". 9 December 2019.
- "Swiss TPH". swisstph.ch. Archived from the original on 26 September 2015. Retrieved 26 May 2015.
- NHA Tanzania 2010
- McIntyre, D. (2008). "Beyond fragmentation and towards universal coverage: insights from Ghana, South Africa and the United Republic of Tanzania". Bulletin of the World Health Organization. 86 (11): 871–876. doi:10.2471/BLT.08.053413. PMC 2649570. PMID 19030693.
- Mills, A.; Ataguba, J. E.; Akazili, J.; Borghi, J.; Garshong, B.; Makawia, S.; MTEItei, G.; Harris, B.; Macha, J.; Meheus, F.; McIntyre, D. (2012). "Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage" (PDF). Lancet. 380 (9837): 126–133. doi:10.1016/S0140-6736(12)60357-2. PMID 22591542.
- "National Health Insurance Fund". nhif.or.tz. Archived from the original on 8 June 2015. Retrieved 26 May 2015.
- "National Social Security Fund - National Social Security Fund". nssf.or.tz. Archived from the original on 12 July 2015. Retrieved 26 May 2015.
- Super User. "CHF". nhif.or.tz. Archived from the original on 27 May 2015. Retrieved 26 May 2015.
- TIRA 2010. Annual insurance Market Performance Report. For The Year Ended 31st December 2010: Tanzania Insurance Regulatory Authority
- Bultman, J.; Kanywanyi, J. L.; Maarifa, H.; Mtei, G. (2012). Tanzania Health Insurance Regulatory Framework Review. Ministry of Health and Social welfare and Social Security Regulatory Authority.
- NHIF, 2011
- nssf. "Social Health Benefits in Tanzania". nssf. Retrieved 8 September 2015.
- Borghi, J.; Maluka, S.; Kuwawenaruwa, A.; Makwai, S.; Tantau, J.; Mtei, G.; Ally, M.; Macha, J. (2013). "Promoting universal financial protection: a case study of new management of community health insurance in Tanzania". Health Research Policy and Systems. 11: 21. doi:10.1186/1478-4505-11-21. PMC 3686629. PMID 23763711.
- "Strategis Insurance (Tanzania) Ltd". strategistz.com. Archived from the original on 25 September 2015. Retrieved 26 May 2015.
- http://aarhealth.com/aar_tz
- JAMU, N.; NDUHIYE, L.; MACHA, J.; KESSY, F.; BORGHI, J. (2009). A Feasibility Study for the Introduction of TIKA in the Three Municipalities of Dar es Salaam Report prepared for the Ministry of Health and Social (Report).
- Health systems financing: the path to universal coverage. WHO. 2010.
- Mtei, G.; Makawia, S.; Ally, M.; Kuwawenaruwa, A.; Meheus, F.; Borghi, J. (1 March 2012). "Who pays and who benefits from health care? An assessment of equity in health care financing and benefit distribution in Tanzania". Health Policy and Planning. 27 (suppl 1): i23–i34. doi:10.1093/heapol/czs018. PMID 22388497.