Emtricitabine/tenofovir
 | |
|
| |
| Combination of | |
|---|---|
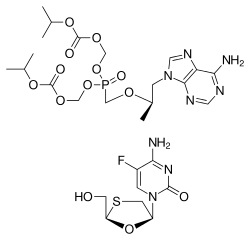
| Tenofovir disoproxil | Nucleotide analogue reverse transcriptase inhibitor |
| Emtricitabine | Nucleoside reverse transcriptase inhibitor |
| Clinical data | |
| Trade names | Truvada, other |
| AHFS/Drugs.com | Professional Drug Facts |
| Pregnancy category | |
| Routes of administration | by mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| PubChem CID | |
| NIAID ChemDB | |
| (verify) | |
Emtricitabine/tenofovir, sold under the brand name Truvada among others, is a medication used to treat and prevent HIV/AIDS.[1][2] It is a fixed-dose combination of two antiretroviral medications: tenofovir disoproxil and emtricitabine.[1] For treatment it is used either alone or together with other antiretroviral medication.[3][4] For prevention before exposure, in those who are at high risk, it is recommended with safe sex practices.[3] It does not cure HIV/AIDS.[1] Emtricitabine/tenofovir is taken by mouth.[5]
Common side effects include headache, feeling tired, trouble sleeping, abdominal pain, weight loss, and rash.[1] Serious side effects may include high blood lactate levels and enlargement of the liver.[3] Use during pregnancy does not appear to harm the baby.[6]
Emtricitabine/tenofovir was approved for medical use in the United States in 2004.[1] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[7] The wholesale cost in the developing world is about US$6.06 to US$7.44 per month.[5] In the United States, as of 2016, the wholesale cost is about US$1,415.00 per month.[8]
Medical uses
Emtricitabine/tenofovir is used to both treat and to prevent HIV/AIDS.[1]
Prevention
In studies, tenofovir reduced the incidence of HIV infection, especially in high-risk individuals (by 42% in MSM), but produced conflicting results in other studies (notably the FEM-PrEP study in heterosexual African women). One study estimated through mathematical modeling that daily intake of tenofovir could potentially achieve a 99% risk reduction of contracting HIV in high-risk individuals.[9] Another study showed overall PrEP effectiveness of 50% rising to 100% when participants took the drug four or more times per week.[10] A Cochrane review found that both tenofovir alone, as well as the tenofovir/emtricitabine combination, decreased the risk of contracting HIV by 51%.[11]
In the US it has been approved for pre-exposure prophylaxis (PrEP) against HIV infection. The Food and Drug Administration approved it for preventative use on July 16, 2012.[12] In the UK a large scale clinical trial has been approved.[13]
The FDA recommends pre-exposure prophylactic (PrEP) considerations for the following high-risk groups:[14]
- Gay or bisexual men who either have had anal sex without a condom or been diagnosed with an STD in the past 6 months
- Heterosexual men or women who do not regularly use condoms during sex with partners of unknown HIV status who are substantial risk
- Injection of drugs in the last month with sharing of equipment
- Sero-discordant heterosexual and homosexual partners where one partner is HIV-positive and the other HIV-negative
The consideration of utilizing Truvada as a reduction strategy involves discussion with a health professional who can help the patient navigate the benefits and risks. Patients who start taking Truvada see HIV reduction benefit up to 72 hours after starting, but the medicine must be taken for thirty days after a high-risk sexual event to ensure HIV transmission levels are optimally reduced.[15]
Available forms
Emtricitabine/tenofovir is a tablet taken by mouth.[5]
Lactation
In pregnancy and lactation, Truvada was shown to be secreted in breast milk.[16]
Side effects
Emtricitabine/tenofovir is generally well-tolerated. Some of its side effects include:[17]
- Rare: lactic acidosis, liver dysfunction, worsening of hepatitis B infection
- Common: headache, abdominal pain, and decreased weight, nausea, diarrhea, decreased bone density
Fat redistribution and accumulation has been observed in people receiving antiretroviral therapy, including fat reductions in the face, limbs, and buttocks and increases in visceral fat of the abdomen and accumulations in the upper back.[17] When used as pre-exposure prophylaxis (PrEP) this effect may not be present.[18] Weight changes have however been linked to the medication.[19]
Drug interactions
The tenofovir component of emtricitabine/tenofovir interacts with the following drugs: didanosine, atazanavir, and lopinavir/ritonavir.
When tenofovir is coadministered with didanosine, the concentration of didanosine increases, and may lead to didanosine toxicity which may result in complications such as pancreatitis and neuropathy. If authorised, the dose of didanosine may be reduced or discontinued completely.
The coadministration of tenofovir and atazanavir results in decreased concentrations of atazanavir and increased concentrations of tenofovir. Atazanavir may be taken with Truvada only with ritonavir and must be monitored for tenofovir toxicity.
The coadministration of tenofovir and lopinavir/ritonavir increases the concentration of tenofovir and must be monitored for tenofovir toxicity.[17]
Other drugs with adverse reactions include adefovir, dabigatran etexilate, lamivudine, and vincristine.
Adefovir: May reduce the therapeutic effect of tenofovir.
Dabigatran Etexilate: Avoid using dabigatran with p-glycoprotein inducers. If dabigatran and p-glycoprotein inducers are used concurrently, monitor for decreased levels/effects of dabigatran.
Lamivudine: May increase the adverse/toxic effect of emtricitabine.
Vincristine (Liposomal): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of vincristine.[20]
High-dose NSAIDs should not be taken by patients who are taking Truvada (tenofovir/emtricitabine) because of possible "new onset or worsening renal impairment."[17]
Society and culture
Cost
As of 2014, the median cost per tablet, in Namibia and South Africa, was US $0.20.[5] In Canada, Truvada costs between $800 - $1,100 per month.[21] Generic emtricitabine/tenofovir was approved by Health Canada in August 2017, with a wholesale cost of $400 per month.[22]
In the United States, as of 2016, the wholesale cost is about US$1415.00 per month.[8] The price of emtricitabine/tenofovir in the United States has been critised by activists, who argued in a 2018 New York Times opinion piece that the high cost keeps the drug out of reach for millions, thus harming efforts to reduce new HIV infections.[23]
Patent status
The patent for the drug combination is owned by Gilead in some regions. The European patent EP0915894B1[24] was due to expire in July 2017, however a case is due before the European Court of Justice seeking to extend the patent.[25] An Irish court rejected an injunction request to prevent the launch of generic versions prior to the resolution of the case.[26]
References
- 1 2 3 4 5 6 7 "Truvada: Uses, Dosage, Side Effects - Drugs.com". www.drugs.com. Archived from the original on 20 December 2016. Retrieved 12 December 2016.
- ↑ "UK label Truvada film-coated tablets". Electronic Medicines Compendium. August 2016. Archived from the original on 2016-12-20.
- 1 2 3 "Truvada - FDA prescribing information, side effects and uses". www.drugs.com. April 2016. Archived from the original on 20 December 2016. Retrieved 12 December 2016.
- ↑ WHO Model Formulary 2008 (PDF). World Health Organization. 2009. p. 160. ISBN 9789241547659. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- 1 2 3 4 "Tenofovir DF+Emtricitabine". International Drug Price Indicator Guide. Management Sciences for Health and World Health Organization. 2014. Retrieved 2015-08-01.
- ↑ "Emtricitabine / tenofovir Use During Pregnancy | Drugs.com". www.drugs.com. Archived from the original on 20 December 2016. Retrieved 12 December 2016.
- ↑ "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- 1 2 "NADAC as of 2016-12-07 | Data.Medicaid.gov". Centers for Medicare and Medicaid Services. Archived from the original on 21 December 2016. Retrieved 12 December 2016.
- ↑ "PK Modeling of Daily TDF/FTC (Truvada) Provides Close to 100% Protection Against HIV Infection". April 2012. Archived from the original on 2015-01-15.
- ↑ "Overall PrEP effectiveness in iPrEx OLE study 50%, but 100% in those taking four or more doses a week". July 2014. Archived from the original on 2016-03-02.
- ↑ Okwundu CI, Uthman OA, Okoromah CAN (2012). Okwundu, Charles I, ed. "Antiretroviral pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals". Cochrane Database Syst Rev. 7 (7): CD007189. doi:10.1002/14651858.CD007189.pub3. PMID 22786505.
- ↑ "FDA approves first pill to help prevent HIV". Seattle Times. 16 July 2012. Archived from the original on 19 July 2012.
- ↑ "NHS England announces major extension of national HIV prevention programme". NHS. 4 December 2016. Archived from the original on 26 February 2017. Retrieved 26 February 2017.
- ↑ "CDC - Pre-Exposure Prophylaxis (PrEP) - Research - Prevention Research - HIV/AIDS". Archived from the original on 5 June 2015. Retrieved 4 June 2015.
- ↑ "Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HIV and Recommendations for Postexposure Prophylaxis". Archived from the original on 8 May 2015. Retrieved 4 June 2015.
- ↑ "Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States" (PDF). nih.gov. National Institutes of Health. Archived (PDF) from the original on 12 April 2014. Retrieved 21 October 2014.
- 1 2 3 4 "US Truvada (emtricitabine/tenofovir disoproxil fumarate) label" (PDF). FDA. March 2016. Archived (PDF) from the original on 2016-12-21.
- ↑ "PrEP does not raise lipids or alter body fat, safety study finds". Retrieved 2018-02-16.
- ↑ "Truvada as HIV PrEP not associated with net fat increase". www.healio.com. Retrieved 2018-02-16.
- ↑ Ramanathan, S; Shen, G; Cheng, A; Kearney, P (2007). "Pharmacokinetics of emtricitabine, tenofovir, and GS-9137 following coadministration of emtricitabine/tenofovir disoproxil fumarate, and ritonavir-boosted GS-9137". J Acquir Immune Defic Syndr. 45 (3): 277. doi:10.1097/QAI.0b013e318050d88c. PMID 17414929.
- ↑ "Pre-Exposure Prophylaxis (PrEP) as a form of HIV prevention". www.actoronto.ca. Archived from the original on 2016-11-04. Retrieved 2016-11-01.
- ↑ "Generic tenofovir + FTC coming to Canada". www.catie.ca. Archived from the original on August 30, 2017. Retrieved August 30, 2017.
- ↑ James Krellenstein, Aaron Lord and Peter Staley (16 July 2018). "Why Don't More Americans Use PrEP?". The New York Times. Retrieved 30 July 2018.
- ↑ "EP0915894B1 - NUCLEOTIDE ANALOGS". Espacenet. Retrieved 13 December 2017.
- ↑ "Gilead in row with generics manufacturers over HIV drug in Ireland". The Irish Times. Retrieved 30 October 2017.
- ↑ "Gilead loss of generic HIV drug battle a boost for gay community". The Irish Times. Retrieved 18 May 2018.