Wilms' tumor
| Wilms' tumor | |
|---|---|
| Synonyms | Wilms' tumor |
 | |
| Cut section showing two halves of a nephroblastoma specimen. Note the prominent septa subdividing the sectioned surface and the protrusion of tumor into the renal pelvis, resembling botryoid rhabdomyosarcoma. | |
| Pronunciation |
|
| Specialty | Oncology |
Wilms tumor, also known as nephroblastoma, is a cancer of the kidneys that typically occurs in children, rarely in adults.[1] It is named after Dr. Max Wilms, the German surgeon (1867–1918) who first described it.[2]
Approximately 500 cases are diagnosed in the U.S. annually. The majority (75%) occur in otherwise normal children; a minority (25%) are associated with other developmental abnormalities. It is highly responsive to treatment, with about 90% of patients surviving at least five years.
Signs and symptoms
Typical signs and symptoms of Wilms tumor include the following:
- a painless, palpable abdominal mass
- loss of appetite
- abdominal pain
- fever
- nausea and vomiting
- blood in the urine (in about 20% of cases)
- high blood pressure in some cases (especially if synchronous or metachronous bilateral kidney involvement)
- Rarely as varicocele[3]
Pathogenesis
Most nephroblastomas are on one side of the body only and are found on both sides in less than 5% of cases, although patients with Denys-Drash syndrome mostly have bilateral or multiple tumors.[4] They tend to be encapsulated and vascularized tumors that do not cross the midline of the abdomen. In cases of metastasis it is usually to the lung. A rupture of Wilms tumor puts the patient at risk of bleeding and peritoneal dissemination of the tumor. In such cases, surgical intervention by a surgeon who is experienced in the removal of such a fragile tumor is imperative.
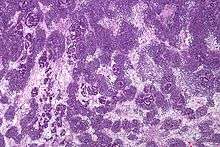
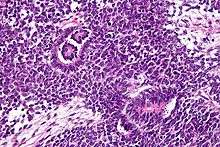
Pathologically, a triphasic nephroblastoma comprises three elements:
- blastema
- mesenchyme (stroma)
- epithelium
Wilms tumor is a malignant tumor containing metanephric blastema, stromal and epithelial derivatives. Characteristic is the presence of abortive tubules and glomeruli surrounded by a spindled cell stroma. The stroma may include striated muscle, cartilage, bone, fat tissue, and fibrous tissue. Dysfunction is caused when the tumor compresses the normal kidney parenchyma.
The mesenchymal component may include cells showing rhabdomyoid differentiation or malignancy (rhabdomyosarcomatous Wilms).
Wilms tumors may be separated into 2 prognostic groups based on pathologic characteristics:
- Favorable - Contains well developed components mentioned above
- Anaplastic - Contains diffuse anaplasia (poorly developed cells)
Molecular biology
Mutations of the WT1 gene on chromosome 11p13 are observed in approximately 20% of Wilms tumors.[5][6] At least half of the Wilms tumors with mutations in WT1 also carry mutations in CTNNB1, the gene encoding the proto-oncogene beta-catenin.[7]
A gene on the X chromosome, WTX, is inactivated in up to 30% of Wilms tumor cases, according to research published in 2007.[8]
Most cases do not have mutations in any of these genes.[9]
Diagnosis
The first sign is normally a painless abdominal tumor that can be easily felt by the doctor. An ultrasound scan, computed tomography scan, or MRI scan is done first. A tumor biopsy is not typically performed due to the risk of creating fragments of cancer tissue and seeding the abdomen with malignant cells.
Staging
Staging is a standard way to describe the extent of spread of Wilms tumors,[10] and to determine prognosis and treatments. Staging is based on anatomical findings and tumor cells pathology.[11][12]
Definitions of stages
Stage I (43% of cases)
Stage I Wilms tumor, all of the following criteria must be met:
- Tumor is limited to the kidney and is completely excised.
- The surface of the renal capsule is intact.
- The tumor is not ruptured or biopsied (open or needle) prior to removal.
- No involvement of extrarenal or renal sinus lymph-vascular spaces
- No residual tumor apparent beyond the margins of excision.
- Metastasis of tumor to lymph nodes not identified.
Stage II (23% of cases)
Stage II Wilms tumor, 1 or more of the following criteria must be met:
- Tumor extends beyond the kidney but is completely excised.
- No residual tumor apparent at or beyond the margins of excision.
- Any of the following conditions may also exist:
- Tumor involvement of the blood vessels of the renal sinus and/or outside the renal parenchyma.
- Extensive tumor involvement of renal sinus soft tissue.
Stage III (20% of cases)
Stage III Wilms tumor, 1 or more of the following criteria must be met:
- Inoperable primary tumor.
- Lymph node metastasis.
- Tumor is present at surgical margins.
- Tumor spillage involving peritoneal surfaces either before or during surgery, or transected tumor thrombus.
- The tumor has been biopsied prior to removal or there is local spillage of tumor during surgery, confined to the flank.
Stage IV (10% of cases)
Stage IV Wilms tumor is defined as the presence of hematogenous metastases (lung, liver, bone, or brain), or lymph node metastases outside the abdomenopelvic region.
Stage V (5% of cases)
Stage V Wilms tumor is defined as bilateral renal involvement at the time of initial diagnosis. Note: For patients with bilateral involvement, an attempt should be made to stage each side according to the above criteria (stage I to III) on the basis of extent of disease prior to biopsy.
Treatment/prognosis
The overall 5-year survival is estimated to be approximately 90%,[13][14] but for individuals the prognosis is highly dependent on individual staging and treatment. Early removal tends to promote positive outcomes.
Tumor-specific loss-of-heterozygosity (LOH) for chromosomes 1p and 16q identifies a subset of Wilms tumor patients who have a significantly increased risk of relapse and death. LOH for these chromosomal regions can now be used as an independent prognostic factor together with disease stage to target intensity of treatment to risk of treatment failure.[15][16] Genome-wide copy number and LOH status can be assessed with virtual karyotyping of tumor cells (fresh or paraffin-embedded).
Statistics may sometimes show more favorable outcomes for more aggressive stages than for less aggressive stages, which may be caused by more aggressive treatment and/or random variability in the study groups. Also, a stage V tumor is not necessarily worse than a stage IV tumor.
| Stage[17] | Histopathology[17] | 4 Year relapse-free survival (RFS) or event-free survival (EFS)[17] | 4 Year overall survival (OS)[17] | Treatment[17] |
|---|---|---|---|---|
| Stage I[17] | Favorable histology in children younger than 24 months or tumor weight less than 550g | 85% | 98% | Surgery only (should be done only within the context of a clinical trial) |
| Favorable histology in children older than 24 months or tumor weight more than 550g | 94% RFS | 98% | Nephrectomy + lymph node sampling followed by regimen EE-4A | |
| Diffuse anaplastic | 68% EFS | 80% | Nephrectomy + lymph node sampling followed by regimen EE-4A and radiotherapy | |
| Stage II[17] | Favorable histology | 86% RFS | 98% | Nephrectomy + lymph node sampling followed by regimen EE-4A |
| Focal anaplastic | 80% EFS | 80% | Nephrectomy + lymph node sampling followed by abdominal radiotherapy and regimen DD-4A | |
| Diffuse anaplastic | 83% EFS | 82% | Nephrectomy + lymph node sampling followed by abdominal radiotherapy and regimen I | |
| Stage III[17] | Favorable histology | 87% RFS | 94% | Nephrectomy + lymph node sampling followed by abdominal radiotherapy and regimen DD-4A |
| Focal anaplastic | 88% RFS | 100% (8 people in study) | Nephrectomy + lymph node sampling followed by abdominal radiotherapy and regimen DD-4A | |
| Focal anaplastic (preoperative treatment) | 71% RFS | 71% | Preoperative treatment with regimen DD-4A followed by nephrectomy + lymph node sampling and abdominal radiotherapy | |
| Diffuse anaplastic | 46% EFS | 53% | Preoperative treatment with regimen I followed by nephrectomy + lymph node sampling and abdominal radiotherapy | |
| Diffuse anaplastic | 65% EFS | 67% | Immediate nephrectomy + lymph node sampling followed by abdominal radiotherapy and regimen I | |
| Stage IV[17] | Favorable histology | 76% RFS | 86% | Nephrectomy + lymph node sampling, followed by abdominal radiotherapy, bilateral pulmonary radiotherapy, and regimen DD-4A |
| Focal anaplastic | 61% EFS | 72% | Nephrectomy + lymph node sampling, followed by abdominal radiotherapy, bilateral pulmonary radiotherapy, and regimen DD-4A | |
| Diffuse anaplastic | 33% EFS | 33% | Immediate nephrectomy + lymph node sampling followed by abdominal radiotherapy, whole-lung radiotherapy, and regimen I | |
| Diffuse anaplastic (preoperative treatment) | 31% EFS | 44% | Preoperative treatment with regimen I followed by nephrectomy + lymph node sampling followed by abdominal radiotherapy, whole-lung radiotherapy | |
| Stage V[17] | Overall | 61% EFS | 80% | |
| Favorable histology | 65% | 87% | Preoperative treatment with regimen DD-4A, followed by nephron sparing surgery or nephrecomy, staging of tumors, and chemotherapy and/or radiotherapy based on pathology and staging | |
| Focal anaplastic | 76% | 88% | Preoperative treatment with regimen DD-4A, followed by nephron sparing surgery or nephrecomy, staging of tumors, and chemotherapy and/or radiotherapy based on pathology and staging | |
| Diffuse anaplastic | 25% | 42% | Preoperative treatment with regimen DD-4A, followed by nephron sparing surgery or nephrecomy, staging of tumors, and chemotherapy and/or radiotherapy based on pathology and staging |
In case of relapse of Wilms tumor, the 4-year survival rate for children with a standard-risk has been estimated to be 80%.[18]
Epidemiology
Wilms tumour affects approximately one person per 10,000 worldwide before the age of 15 years.[19] People of African descent may have slightly higher rates of Wilms tumor.[20] The peak age of Wilms tumour is 3 to 4 years and most cases occur before the age of 10 years.[21] A genetic predisposition to Wilms Tumor in individuals with aniridia has been established, due to deletions in the p13 band on chromosome 11.[22]
History
Dr. Sidney Farber, founder of Dana-Farber Cancer Institute, and his colleagues achieved the first remissions in Wilms tumor in the 1950s. By employing the antibiotic actinomycin D in addition to surgery and radiation therapy, they boosted cure rates from 40 to 89 percent.
See also
References
- ↑ EBSCO database verified by URAC; accessed from Mount Sinai Hospital, New York
- ↑ WhoNamedIt.com: Max Wilms
- ↑ Williams, Vijai; Munikoty, Vinay; Trehan, Amita (2018-03-23). "Varicocele with an Abdominal Mass". The Journal of Pediatrics. doi:10.1016/j.jpeds.2018.02.023. ISSN 1097-6833. PMID 29580678.
- ↑ Guaragna, Mara Sanches; Soardi, Fernanda Caroline; Assumpção, Juliana Godoy; Zambaldi, Lílian de Jesus Girotto; Cardinalli, Izilda Aparecida; Yunes, José Andrés; De Mello, Maricilda Palandi; Brandalise, Silvia Regina; Aguiar, Simone dos Santos (2010). "The Novel WT1 Gene Mutation p.H377N Associated to Denys-Drash Syndrome". Journal of Pediatric Hematology/Oncology. 32 (6): 486–8. doi:10.1097/MPH.0b013e3181e5e20d. PMID 20562648.
- ↑ Call, Katherine M.; Glaser, Tom; Ito, Caryn Y.; Buckler, Alan J.; Pelletier, Jerry; Haber, Daniel A.; Rose, Elise A.; Kral, Astrid; Yeger, Herman; Lewis, William H.; Jones, Carol; Housman, David E. (1990). "Isolation and characterization of a zinc finger polypeptide gene at the human chromosome 11 Wilms' tumor locus". Cell. 60 (3): 509–20. doi:10.1016/0092-8674(90)90601-A. PMID 2154335.
- ↑ Huff, Vicki (1998). "Wilms tumor genetics". American Journal of Medical Genetics. 79 (4): 260–7. doi:10.1002/(SICI)1096-8628(19981002)79:4<260::AID-AJMG6>3.0.CO;2-Q. PMID 9781905.
- ↑ Maiti, S; Alam, R; Amos, C. I.; Huff, V (2000). "Frequent association of beta-catenin and WT1 mutations in Wilms tumors". Cancer Research. 60 (22): 6288–92. PMID 11103785.
- ↑ Rivera, M. N.; Kim, W. J.; Wells, J.; Driscoll, D. R.; Brannigan, B. W.; Han, M.; Kim, J. C.; Feinberg, A. P.; Gerald, W. L.; Vargas, S. O.; Chin, L.; Iafrate, A. J.; Bell, D. W.; Haber, D. A. (2007). "An X Chromosome Gene, WTX, is Commonly Inactivated in Wilms Tumor". Science. 315 (5812): 642–5. Bibcode:2007Sci...315..642R. doi:10.1126/science.1137509. PMID 17204608.
- ↑ Ruteshouser, E. Cristy; Robinson, Stephen M.; Huff, Vicki (2008). "Wilms tumor genetics: Mutations in WT1, WTX, and CTNNB1 account for only about one-third of tumors". Genes, Chromosomes and Cancer. 47 (6): 461–70. doi:10.1002/gcc.20553. PMC 4332772. PMID 18311776.
- ↑ "How is Wilms tumor staged?". www.cancer.org. Retrieved 2015-11-15.
- ↑ "Wilms Tumor - Childhood - Stages". Cancer.Net. Retrieved 2015-11-15.
- ↑ "Treatment by type and stage of Wilms tumor". www.cancer.org. Retrieved 2015-11-13.
- ↑ Stewenius, Y.; Jin, Y.; Ora, I.; De Kraker, J.; Bras, J.; Frigyesi, A.; Alumets, J.; Sandstedt, B.; Meeker, A. K.; Gisselsson, D. (2007). "Defective Chromosome Segregation and Telomere Dysfunction in Aggressive Wilms' Tumors". Clinical Cancer Research. 13 (22): 6593–602. doi:10.1158/1078-0432.CCR-07-1081. PMID 18006759.
- ↑ Tournade, M. F.; Com-Nougué, C; De Kraker, J; Ludwig, R; Rey, A; Burgers, J. M.; Sandstedt, B; Godzinski, J; Carli, M; Potter, R; Zucker, J. M.; International Society of Pediatric Oncology Nephroblastoma Trial Study Committee (2001). "Optimal duration of preoperative therapy in unilateral and nonmetastatic Wilms' tumor in children older than 6 months: Results of the Ninth International Society of Pediatric Oncology Wilms' Tumor Trial and Study". Journal of Clinical Oncology. 19 (2): 488–500. doi:10.1200/jco.2001.19.2.488. PMID 11208843.
- ↑ Messahel, Boo; Williams, Richard; Ridolfi, Antonia; a’Hern, Roger; Warren, William; Tinworth, Lorna; Hobson, Rachel; Al-Saadi, Reem; Whyman, Gavin; Brundler, Marie-Anne; Kelsey, Anna; Sebire, Neil; Jones, Chris; Vujanic, Gordan; Pritchard-Jones, Kathy; Children's Cancer Leukaemia Group (CCLG) (2009). "Allele loss at 16q defines poorer prognosis Wilms tumour irrespective of treatment approach in the UKW1–3 clinical trials: A Children's Cancer and Leukaemia Group (CCLG) study". European Journal of Cancer. 45 (5): 819–26. doi:10.1016/j.ejca.2009.01.005. PMID 19231157.
- ↑ Grundy, P. E.; Breslow, N. E.; Li, S; Perlman, E; Beckwith, J. B.; Ritchey, M. L.; Shamberger, R. C.; Haase, G. M.; d'Angio, G. J.; Donaldson, M; Coppes, M. J.; Malogolowkin, M; Shearer, P; Thomas, P. R.; MacKlis, R; Tomlinson, G; Huff, V; Green, D. M.; National Wilms Tumor Study Group (2005). "Loss of Heterozygosity for Chromosomes 1p and 16q is an Adverse Prognostic Factor in Favorable-Histology Wilms Tumor: A Report from the National Wilms Tumor Study Group". Journal of Clinical Oncology. 23 (29): 7312–21. doi:10.1200/JCO.2005.01.2799. PMID 16129848.
- 1 2 3 4 5 6 7 8 9 10 Unless otherwise specified in boxes, then reference is: Treatment of Wilms Tumor at National Cancer Institute. Last Modified: 03/29/2012
- ↑ Spreafico, Filippo; Pritchard Jones, Kathy; Malogolowkin, Marcio H; Bergeron, Christophe; Hale, Juliet; de Kraker, Jan; Dallorso, Sandro; Acha, Thomás; de Camargo, Beatriz; Dome, Jeffrey S; Graf, Norbert (2014). "Treatment of relapsed Wilms tumors: lessons learned". Expert Review of Anticancer Therapy. 9 (12): 1807–1815. doi:10.1586/era.09.159. ISSN 1473-7140.
- ↑ Breslow, N; Olshan, A; Beckwith, JB; Green, DM (1993). "Epidemiology of Wilms tumor". Medical and pediatric oncology. 21 (3): 172–81. doi:10.1002/mpo.2950210305. PMID 7680412.
- ↑ Breslow, N; Olshan, A; Beckwith, JB; Green, DM (1993). "Epidemiology of Wilms tumor". Medical and pediatric oncology. 21 (3): 172–81. doi:10.1002/mpo.2950210305. PMID 7680412.
- ↑ Breslow, NE; Beckwith, JB; Perlman, EJ; Reeve, AE (September 2006). "Age distributions, birth weights, nephrogenic rests, and heterogeneity in the pathogenesis of Wilms tumor". Pediatric blood & cancer. 47 (3): 260–7. doi:10.1002/pbc.20891. PMC 1543666. PMID 16700047.
- ↑ Pritchard-Jones, Kathryn; Fleming, Stewart; Davidson, Duncan; Bickmore, Wendy; Porteous, David; Gosden, Christine; Bard, Jonathan; Buckler, Alan; Pelletier, Jerry; Housman, David; Van Heyningen, Veronica; Hastie, Nicholas (1990). "The candidate Wilms' tumour gene is involved in genitourinary development". Nature. 346 (6280): 194–7. Bibcode:1990Natur.346..194P. doi:10.1038/346194a0. PMID 2164159.
External links
| Classification | |
|---|---|
| External resources |