Homosalate
 | |
 | |
| Names | |
|---|---|
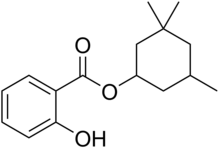
| IUPAC name
3,3,5-Trimethylcyclohexyl 2-hydroxybenzoate | |
| Other names
Homosalate | |
| Identifiers | |
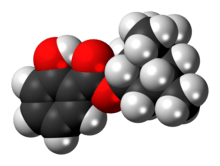
3D model (JSmol) |
|
| ChemSpider | |
| ECHA InfoCard | 100.003.874 |
| KEGG | |
PubChem CID |
|
| UNII | |
| |
| |
| Properties | |
| C16H22O3 | |
| Molar mass | 262.35 g·mol−1 |
| Density | 1.045 g/cm3 |
| Melting point | <25 °C |
| Boiling point | 161 to 165 °C (322 to 329 °F; 434 to 438 K) at 4 mmHg |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Homosalate is an organic compound used in some sunscreens. It is an ester formed from salicylic acid and 3,3,5-trimethylcyclohexanol, a derivative of cyclohexanol. Contained in 45% of U.S. sunscreens, it is used as a chemical UV filter.[2] The salicylic acid portion of the molecule absorbs ultraviolet rays with a wavelength from 295 nm to 315 nm, protecting the skin from sun damage. The hydrophobic cyclohexanol portion provides greasiness that prevents it from dissolving in water.
Safety
Similar to other UV filter compounds,[3] more homosalate is absorbed into the stratum corneum of the face (25% of applied dose) versus back of volunteers.[4] Homosalate has been identified as an antiandrogen in vitro,[5] as well as having estrogenic activity toward estrogen receptors α,[6] and general in vitro estrogenic activity.[7] Homosalate has been shown to be an antagonist toward androgen and estrogen receptors in vitro.[8] There is also evidence that homosalate, (and other UV filters) can break down into more toxic products.[9]
No evidence of toxicity or side effects have been documented in vivo.
References
- ↑ Homosalate, Merck Index, 11th Edition, 4660.
- ↑ Homosalate, ChemIDplus.
- ↑ Rougier A, Dupuis D, Lotte C, Roguet R, Wester RC, Maibach HI (1986). "Regional variation in percutaneous absorption in man: measurement by the stripping method". Arch. Dermatol. Res. 278 (6): 465–469. doi:10.1007/bf00455165. PMID 3789805.
- ↑ Benson HA, Sarveiya V, Risk S, Roberts MS. "Influence of anatomical site and topical formulation on skin penetration of sunscreens". Ther Clin Risk Manag. 1: 209–218. PMC 1661631. PMID 18360561.
- ↑ Ma et al., 2003.
- ↑ Gomez E, Pillon A, Fenet H, Rosain D, Duchesne MJ, Nicolas JC, Balaguer P, Casellas C. "Estrogenic activity of cosmetic components in reporter cell lines: parabens, UV screens, and musks". J Toxicol Environ Health A. 68: 239–251. doi:10.1080/15287390590895054. PMID 15799449.
- ↑ Schlumpf M, Schmid P, Durrer S, Conscience M, Maerkel K, Henseler M, Gruetter M, Herzog I, Reolon S, Ceccatelli R, Faass O, Stutz E, Jarry H, Wuttke W, Lichtensteiger W. "Endocrine activity and developmental toxicity of cosmetic UV filters--an update". Toxicology. 205: 113–122. doi:10.1016/j.tox.2004.06.043. PMID 15458796.
- ↑ Schreurs RH, Sonneveld E, Jansen JH, Seinen W, van der Burg B (February 2005). "Interaction of polycyclic musks and UV filters with the estrogen receptor (ER), androgen receptor (AR), and progesterone receptor (PR) in reporter gene bioassays". Toxicol. Sci. 83: 264–272. doi:10.1093/toxsci/kfi035. PMID 15537743.
- ↑ Klimova, et al. (2013). "Current problems in the use of organic UV filters to protect skin from excessive sun exposure" (PDF). Acta Chimica Slovaca. 6 (1): 82–88. doi:10.2478/acs-2013-0014.