Hemoptysis
| Hemoptysis | |
|---|---|
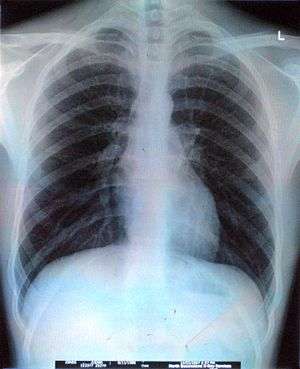 | |
| Hemoptysis can be discovered with the help of radiology. | |
| Pronunciation |
|
| Classification and external resources | |
| Specialty | Pulmonology |
| ICD-10 | R04.2 |
| ICD-9-CM | 786.30 |
| DiseasesDB | 5578 |
| MedlinePlus | 003073 |
| Patient UK | Hemoptysis |
| MeSH | D006469 |
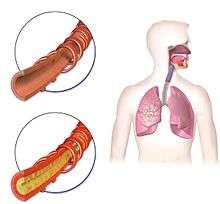
Hemoptysis, also spelled haemoptysis, is the coughing up of blood or blood-stained mucus from the bronchi, larynx, trachea, or lungs. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia, and certain cardiovascular conditions. Hemoptysis is considered massive at 300 mL (11 imp fl oz; 10 US fl oz). In such cases, there are always severe injuries. The primary danger comes from choking, rather than blood loss.[1]
Diagnosis

- Past history, history of present illness, family history
- history of tuberculosis, bronchiectasis, chronic bronchitis, mitral stenosis, etc.
- history of cigarette smoking, occupational diseases by exposure to silica dust, etc.
- Blood
- duration, frequency, amount
- Amounts of blood: large amounts of blood, or is there blood-streaked sputum
- Probable source of bleeding: Is the blood coughed up, or vomited?
- Bloody sputum
- color, characters: blood-streaked, fresh blood, frothy pink, bloody gelatinous.
- Accompanying symptoms
- fever, chest pain, coughing, purulent sputum, mucocutaneous bleeding, jaundice.
- Imaging examination
- chest X-ray, CT scan and 3D reconstruction images or CT virtual bronchoscopy, bronchial angiography.
- Laboratory tests
- blood test: WBC
- Sputum: cells and bacterial examinations, sputum culture
- Bronchial fiber endoscopy[2]
Differential diagnosis
Conditions which commonly involve hemoptysis include bronchitis and pneumonia, lung cancers and tuberculosis. Other possible underlying causes include aspergilloma, bronchiectasis, coccidioidomycosis, pulmonary embolism, pneumonic plague, and cystic fibrosis. Rarer causes include hereditary hemorrhagic telangiectasia (HHT or Rendu-Osler-Weber syndrome), Goodpasture's syndrome, and granulomatosis with polyangiitis. In children, hemoptysis is commonly caused by the presence of a foreign body in the airway. The condition can also result from over-anticoagulation from treatment by drugs such as warfarin.
Blood-laced mucus from the sinus or nose area can sometimes be misidentified as symptomatic of hemoptysis (such secretions can be a sign of nasal or sinus cancer, but also a sinus infection). Extensive non-respiratory injury can also cause one to cough up blood. Cardiac causes like congestive heart failure and mitral stenosis should be ruled out.
The origin of blood can be identified by observing its color. Bright-red, foamy blood comes from the respiratory tract, whereas dark-red, coffee-colored blood comes from the gastrointestinal tract. Sometimes hemoptysis may be rust-colored.
The most common cause of minor hemoptysis is bronchitis.[1]
- Lung cancer, including both non-small cell lung carcinoma and small cell lung carcinoma.[3][4]
- Sarcoidosis[5]
- Aspergilloma[6]
- Tuberculosis[7]
- Histoplasmosis[8]
- Pneumonia
- Pulmonary edema
- Foreign body aspiration and aspiration pneumonia
- Goodpasture's syndrome[9]
- Granulomatosis with polyangiitis[10]
- Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)
- Bronchitis[11]
- Bronchiectasis[11]
- Pulmonary embolism[12]
- Anticoagulant use[12]
- Trauma[12]
- Lung abscess[12]
- Mitral stenosis
- Tropical eosinophilia
- Bleeding disorders
- Hughes-Stovin syndrome and other variants of Behçet's disease
- Squamous cell carcinoma of esophagus
- Pulmonary arteriovenous malformations
Treatment
Treatment depends on the underlying cause. Treatments include iced saline, and topical vasoconstrictors such as adrenalin or vasopressin. Selective bronchial intubation can be used to collapse the lung that is bleeding. Also, endobronchial tamponade can be used. Laser photocoagulation can be used to stop bleeding during bronchoscopy. Angiography of bronchial arteries can be performed to locate the bleeding, and it can often be embolized.[13] Surgical option is usually the last resort, and can involve, removal of a lung lobe or removal of the entire lung. Non–small-cell lung cancer can also be treated with erlotinib or gefitinib.[14] Cough suppressants can increase the risk of choking.[1]
References
- 1 2 3 Sabatine, [edited by] Marc S. (2014). Pocket medicine (Fifth ed.). [S.l.]: Aspen Publishers, Inc. ISBN 978-1451193787.
- ↑ Richard F.LeBlond (2004). Diagnostics. US: McGraw-Hill Companies, Inc. ISBN 978-0-07-140923-0.
- ↑ Google Health – Google
- ↑ Google Health – Google
- ↑ Sarcoidosis Signs & Symptoms – Sarcoidosis – HealthCommunities.com
- ↑ MedlinePlus Encyclopedia Pulmonary aspergilloma
- ↑ Google Health – Google
- ↑ Histoplasmosis Symptoms – Diseases and Conditions – Mayo Clinic
- ↑ Pediatric Goodpasture Syndrome at eMedicine
- ↑ "Granulomatosis with Polyangiitis". www.mayoclinic.org. Mayo Foundation for Medical Education and Research. Retrieved 3 March 2018.
- 1 2 Hemoptysis Causes – Hemoptysis – HealthCommunities.com
- 1 2 3 4 Other Causes of Hemoptysis – Hemoptysis – HealthCommunities.com
- ↑ Uppsala Academic Hospital > Guidelines for treatment of acute lung diseases. August 2004. Authors: Christer Hanson, Carl-Axel Karlsson, Mary Kämpe, Kristina Lamberg, Eva Lindberg, Lavinia Machado Boman, Gunnemar Stålenheim
- ↑ Welcome to Elgg
External links
- Corey, Ralph (1990). "Hemoptysis". Clinical Methods: The History, Physical, and Laboratory Examinations. Butterworths. Retrieved 26 June 2018.