Pelvic examination
| Pelvic examination | |
|---|---|
 Line drawing showing palpation in pelvic exam. | |
| Specialty | gynaecology |
| ICD-9-CM | 89.26 |
A pelvic examination is the physical examination of the external and internal female pelvic organs.[1] It is called "bimanual exam" when two hands are used and "manual uterine palpation" (palpation meaning an examination by touch). It is frequently used in gynecology. It can also be done under general anesthesia.[2]
The examination can be uncomfortable. During the pelvic exam the vaginal wall is assessed for rugae, texture and weak spots.[3] In addition to a thorough pelvic exam, other tests may ordered to further determine the cause of symptoms that are concerning.[4] During the pelvic exam, samples of vaginal fluids may be taken to screen for sexually transmitted infections or other infections.[5]
Some clinicians combine a routine pelvic exam along with other preventative procedures like a breast examination and pap smear.[6] The American College of Physicians published guidelines against routine pelvic examination in adult women who are not pregnant and lack symptoms in 2014.[7] One exception being pelvic exams done as part of cervical cancer screening.[8] A pelvic examination can be part of the assessment of sexual assault.[6]
Medical uses
Previous to July 2014 the benefits of routine pelvic examinations were not clear and there was no consensus.[9] Since then, American College of Physicians (ACP) issued a guideline recommending against performing this examination to screen for conditions in asymptomatic, nonpregnant, adult women. (The guideline did not consider pap smears.) The ACP said that there was no evidence of benefit in support of the examination, but there was evidence of harm, including distress and unnecessary surgery. This was a strong recommendation, based on moderate-quality evidence.[7]
Pelvic exams are an occasion for gynecologists to recognize issues like incontinence and sexual dysfunction, and discuss patient concerns.[10]
External examination
The pelvic exam begins with an explanation of the procedure. The woman is asked to put on an examination gown, get on the examination table, lay on her back with her feet in stirrups.[6] Sliding down toward the end of the table is the best position for the clinician to do a visual examination.[4] A pelvic exam begins with an assessment of the reproductive organs that can be seen without the use of a speculum.[11] Many women may want to 'prepare' for the procedure.[4] Douching before the exam is discouraged because cells needed from the cervix to assess for cervical cell abnormalities may be washed out.[3] One possible reason for delaying an exam is if it is to be done during menstruation, but this is a preference of some women and not a requirement of the clinician.[4] The woman will probably will be asked to put on an examination gown and lay down on the examination table.[4] A girl or woman may ask to have another woman in the examination room during the exam. The clinician may want to perform pelvic examination and assessment of the vagina because there are unexplained symptoms of vaginal discharge, pelvic pain, unexpected bleeding, or urinary problems.[3][4]
The typical external examination begins with making sure that a woman is in a comfortable position and her privacy respected.
- If a woman is obese, different positioning and assistance may be required to keep tissue from blocking the view of the perineal area.[3]
- The pubic hair is inspected for pubic lice and hair growth patterns. Sparse hair patterns can exist in older and in some Asian women.[3]
- The labia majora are evaluated. Their position and symmetry are assessed. The expected finding in older women is that the labia majora can be thinner and smaller. The examiner is looking for ulcers, inflammation, warts and rashes. If drainage is present from these structures, its color, location and other characteristics are noted. Infection control is accomplished by frequent glove changes.[3]
- The labia minora are then evaluated. They should appear moist, smooth in texture and pink. The presence of tearing, inflammation and swelling is noted. Thinner and smaller labia minora are an expected finding in older women.
- The clitoris is assessed for size, position, symmetry, and inflammation.[3]
- The urethral opening is inspected. No urine should leak when the woman is asked to cough. Urine leakage may indicate stress incontinence and the weakening of pelvic structures. The opening should be midline, pink, and smooth. The presence of inflammation, or discharge which may indicate an infection. Excoriation can be present in obese women due to urinary incontinence.[3]
- The vaginal opening is inspected for position, presence of the hymen, and shape. The presence of bruising, tearing, inflammation and discharge. Pelvic examinations are usually procedures that are designed to obtain objective, measurable descriptions of what is observed. If sexual abuse is suspected, questions regarding this is discussed after the examination and not during it. When the woman is requested to 'bear down', the presence of prolapsed structures are documented. Prolapsed structures can appear when abdominal pressure increases or they can hang free without bearing down.[3]
- The perineum, the space between the vagina and the anus is inspected. It should be smooth, firm and free of disease. Scars from episiotomies are visible on women who have had the procedure during childbirth.[3][12]
- The anus is assessed for lesions, inflammation or trauma. It should appear dark, continuous and moist. In an obese women, excoriation may be present due to fecal incontinence.[3]
Internal examination

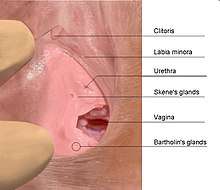
Before inserting the speculum, the vaginal wall, urethra, Skene's glands and Bartholin's glands are palpated through the vaginal wall. During the internal exam, the examiner describes the procedure while doing the assessment, making sure that the woman can anticipate where she will feel the palpations.[3]
- The woman is first informed that the examiner will insert their finger into the vagina. The palpation of the vagina is done by evaluating the condition of the vaginal walls. These should feel smooth, consistent and soft. The rugae can also be assessed by palpation.[3]
- The woman is again asked to bear down while the examiner continues the internal examination. The presence of bulging is assessed.[3]
- The position of the urethra is assessed by palpation with a finger through the vaginal wall.[3]
- The Skene's glands, located on each side of the urethra are palpated to produce secretion from the glands.[3]
- The Bartholin glands are also assessed internally by gently squeezing them with one finger placed externally, on the posterior labia majora and the other finger in the vagina.[3]
At this point of the pelvic exam, the examiner will insert the speculum to visualize other internal structures: the cervix, uterus, and ovaries.[3][13] If this is the first pelvic exam of the woman, the examiner will show the speculum to the woman, explain its use and answer any questions.
- The appropriate sized speculum is selected.[3] The speculum is slowly inserted in its collapsed state at a forty-five degree angle to match the slope of the vagina. The blades are then expanded until the cervix comes into view.[3] If the speculum is transparent, the vaginal walls can be seen.
- The cervix is then assessed. It should look moist, round, pink, and centered to the middle. The secretions of the cervix should be clear or whitish with no odor. The presence or absence of polyps, ulcers, and inflammation are noted.The appropriate sized speculum is selected. The speculum is slowly inserted in its collapsed state at a forty-five degree angle to match the slope of the vagina. The blades are then expanded until the cervix comes into view.[3]
- A swab or cytobrush will be used to collect or scrape cervical cells off of the surface of the cervix to be evaluated for changes. Other vaginal swabs can be taken at this time to test for sexually transmitted diseases.[3][11]
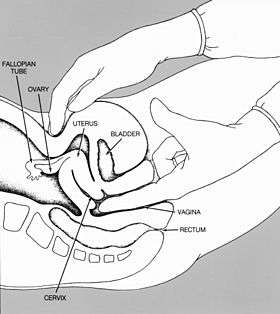
The next part of the pelvic exam is the Bimanual palpation and begins after the speculum is removed.
- The examiner informs and explains this part of the exam. Two fingers are used to palpate the cervix.[3]
- The cervix and fornices are assessed for mobility and the presence of lumps.[3]
- The uterus is palpated and evaluated to determine its position by leaving the fingers of one hand in the vagina while pressure to the abdomen is applied with the other hand. If the body tissue is too thick due to obesity, an ultrasound may be performed instead.[3]
- The ovaries can be palpated through the abdomen. They should be mobile, about the size of an almond but can vary in texture. Sometimes the ovaries cannot be palpated.[3]
- If the examiner can feel the fallopian tubes, this is not a normal finding.[3]
- The examiner removes their hands and puts on clean gloves to assess the rectum, and explains this part of the exam to the woman.[3]
- The rectum is assessed by having one finger in the vagina and the other in the rectum. The rectum should be smooth.[3]
The examiner removes their fingers, discards their gloves, washes their hands and helps the women get into an upright position. Any deviations from what is considered normal will be discussed.[3]
During pregnancy
Prenatal care includes regular pelvic exams during the pregnancy. Women with high risk pregnancies see their obstetrician more often. These are:
- Very young age or older than 35
- Overweight or underweight
- Problems in previous pregnancy
- Health conditions you have before you become pregnant, such as high blood pressure, diabetes, autoimmune disorders, cancer, and HIV
- Pregnancy with twins or other multiples[14]
The pelvic exam during pregnancy is similar to the exam for non-pregnant women. One difference is that more attention is give to the uterus and cervix. The growth of the uterus is measured each visit. As the due date approaches, the assessment of the cervix will indicate whether labor ahas begun or is progressing. Much time is spent determining the health of the fetus. A normal finding during the exam on the pregnant woman is that the vagina has a bluish tinge. If a bluish tinge is observed in the non-pregnant women, this is a sign of hypoxia.[3]
Informed consent
Part of the procedure is to inform that woman that she can stop the exam at any time.[6]
See also
References
- ↑ "Examination of the Female Pelvis". Archived from the original on 2001-11-15. Retrieved 2007-12-09.
- ↑ "Current Procedural Terminology - Pelvic examination under anesthesia (other than local) - Classes | NCBO BioPortal". bioportal.bioontology.org. Retrieved 2018-03-02.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 Damico D (2016). Health & physical assessment in nursing. Boston: Pearson. pp. 660–665 and 827–848. ISBN 978-0133876406.
- 1 2 3 4 5 6 "Pelvic exam - About - Mayo Clinic". www.mayoclinic.org. Retrieved 2018-01-04.
- ↑ "NCI Dictionary of Cancer Terms". National Cancer Institute. Retrieved 2018-01-04.
- 1 2 3 4 Williams gynecology. Hoffman, Barbara L. (2nd ed.). New York: McGraw-Hill Medical. 2012. pp. 2–6. ISBN 9780071716727. OCLC 779244257.
- 1 2 Qaseem, A; Humphrey, LL; Harris, R; Starkey, M; Denberg, TD; Clinical Guidelines Committee of the American College of, Physicians (Jul 1, 2014). "Screening pelvic examination in adult women: a clinical practice guideline from the American College of Physicians". Annals of Internal Medicine. 161 (1): 67–72. doi:10.7326/M14-0701. PMID 24979451. [Free text]
- ↑ "American Academy of Family Physicians | Choosing Wisely". www.choosingwisely.org. Retrieved 14 August 2018.
- ↑ Bibbins-Domingo, Kirsten; Grossman, David C.; Curry, Susan J.; Barry, Michael J.; Davidson, Karina W.; Doubeni, Chyke A.; Epling, John W.; García, Francisco A. R.; Kemper, Alex R.; Krist, Alex H.; Kurth, Ann E.; Landefeld, C. Seth; Mangione, Carol M.; Phillips, William R.; Phipps, Maureen G.; Silverstein, Michael; Simon, Melissa; Siu, Albert L.; Tseng, Chien-Wen (7 March 2017). "Screening for Gynecologic Conditions With Pelvic Examination". JAMA. 317 (9): 947. doi:10.1001/jama.2017.0807.
- ↑ ACOG Practice Advisory on Annual Pelvic Examination Recommendations June 30, 2014
- 1 2 "Your First Gynecologic Visit" (PDF). American College of Obstetricians and Gynecologists. May 2017.
- ↑ "NCI Dictionary of Cancer Terms". National Cancer Institute. Retrieved 2018-01-05.
- ↑ "Pelvic exam - MayoClinic.com". Retrieved 2007-12-09.
- ↑ "Prenatal care and tests | womenshealth.gov". womenshealth.gov. Retrieved 2018-01-05.