Fresh frozen plasma
|
A bag containing one unit of fresh frozen plasma | |
| Clinical data | |
|---|---|
| Synonyms | Plasma frozen within 24 hours after phlebotomy (FP24)[1] |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category | |
| ATC code | |
| Identifiers | |
| ChemSpider |
|
Fresh frozen plasma (FFP) is a blood product made from the liquid portion of whole blood.[3] It is used to treat conditions in which there are low blood clotting factors (INR>1.5) or low levels of other blood proteins.[3][1] It is also used as part of plasma exchange.[2] The specific batch typically needs to be tested for compatibility before it is given.[3] Use as a volume expander is not recommended.[3] It is given by injection into a vein.[2]
Side effects include nausea and itchiness.[3] Rarely there may be allergic reactions, blood clots, or infections.[3][1] It is unclear if use during pregnancy or breastfeeding is safe for the baby.[2] Greater care should be taken in people with protein S deficiency, IgA deficiency, or heart failure.[2] Fresh frozen plasma is made up of a complex mixture of water, proteins, carbohydrates, fats, and vitamins.[1] When frozen it lasts about a year.[1]
Plasma first came into medical use during the Second World War.[1] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[4] In the United Kingdom it costs about £30 per unit.[5] A number of other versions also exist including plasma frozen within 24 hours after phlebotomy, cryoprecipitate reduced plasma, and solvent detergent plasma.[1]
Definition
In the United States it refers to the fluid portion of one unit of human blood that has been centrifuged, separated, and frozen solid at −18 °C (0 °F) or colder within eight hours of collection.[6] The phrase "FFP" is often used to mean any transfused plasma product. The other commonly transfused plasma, PF24, has similar indications as those for FFP with the exception of heat-sensitive proteins in the plasma such as factor V.
Medical uses
There are few specific indications for FFP. These generally are limited to the treatment of deficiencies of coagulation proteins for which specific factor concentrates are unavailable or undesirable. In many clinical practices, fresh and frozen plasma contains proteins with two important coagulation factors in it—the V and the VIII. Other documentations indicate FFP has not enough beneficial effect when it is used as a transfusion to stop massive bleeding.[7] In addition, circumstances exist in which FFP has been employed and is believed to be of therapeutic value, but data supporting its efficacy are limited or unavailable (e.g., multiple coagulation protein deficiencies in uncontrollably bleeding). Because such people are often critically ill and satisfactory alternative therapy may not be at hand, FFP may be appropriate.
Indications for the use of FFP include the following:
- Replacement of isolated factor deficiencies FFP is used to treat rare bleeding disorders when specific factor concentrates are not available. FFP is the usual treatment for factor V deficiency.[8]
- Reversal of warfarin effect Patients who are anticoagulated with warfarin are deficient in the functional vitamin K dependent coagulation factors II, VII, IX, and X, as well as proteins C and S. These functional deficiencies can be reversed by the administration of vitamin K. For anticoagulated patients who are actively bleeding or who require emergency surgery prothrombin complex concentrate should be used if available.[9] FFP (or single-donor plasma) should only be used if more effective alternative treatments are not available. The ASA task force recommends starting with 5-8 mL/kg of FFP for warfarin reversal and rechecking laboratory values.[9]
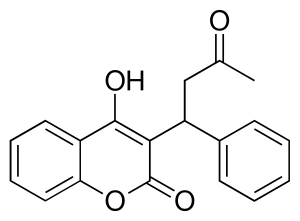 Warfarin
Warfarin - Use in antithrombin III deficiency FFP can be used as a source of antithrombin III in patients who are deficient of this inhibitor and are undergoing surgery or who require heparin for treatment of thrombosis.
- Treatment of immunodeficiencies FFP is useful in infants with secondary immunodeficiency associated with severe protein-losing enteropathy and in whom total parenteral nutrition is ineffectual. FFP also can be used as a source of immunoglobulin for children and adults with humoral immunodeficiency. However, the development of a purified immune globulin for intravenous use largely has replaced Fresh frozen plasma
- Treatment of thrombotic thrombocytopenic purpura FFP may be beneficial for the treatment of thrombotic thrombocytopenic purpura.
FFP is not recommended unless there is ongoing bleeding or there is a significant blood clotting problem. That is, FFP is not used in people to reverse warfarin if there is no bleeding, even for an INR > 9 unless they need urgent surgery. It is also not used in elective surgery, or non-emergent surgery.[10]
Risks
The risks of FFP include disease transmission, anaphylactoid reactions, and excessive intravascular volume, as well as transfusion related acute lung injury (TRALI) and an increase in infections (including surgical wound infections). The potential viral infectivity of FFP probably is similar to that of whole blood and red blood cells. The rate of posttransfusion hepatitis depends on many factors, including donor selection. In rare instances, human immunodeficiency virus (HIV) is transmitted by blood transfusions and possibly by FFP. Allergic or anaphylactoid reactions can occur in response to FFP administration and may vary from hives to fatal noncardiogenic pulmonary edema.
FFP should be blood type-matched to ensure compatibility, as agglutination reactions are possible, though rare. As with any intravenously administered fluid, excessive amounts of FFP may result in hypervolemia and cardiac failure.
Chemistry
FFP is made by centrifugation followed by freezing and preservation.
Frequency of use
The use of plasma and its products has evolved over a period of four decades. The use of FFP has increased tenfold in the United States from between the years 2000-2010 and has reached almost 2 million units annually. This trend may be attributable to multiple factors, possibly including decreased availability of whole blood due to widespread acceptance of the concept of component therapy.
Alternatives
Evidence indicates that other plasma components (e.g., single-donor plasma) that do not meet the criteria of FFP may have adequate levels of coagulation factors and are suitable for patients in whom FFP is indicated. Single-donor plasma is efficacious in the treatment of mild deficiencies of stable clotting factors. It also is of value in treatment of multiple deficiencies as in reversal of warfarin effects or in liver disease.
Safe and effective alternative treatment often exists so that FFP is no longer the therapy of choice in many conditions. Cryoprecipitate should be used when fibrinogen or von Willebrand factor is needed. For treatment of hemophilia A, cryoprecipitate or factor VIII concentrates, heated or unheated, are available. For treatment of severe hemophilia B, factor IX complex is preferable. Both of these concentrates are prepared from pooled plasma, and the risk of virus transmission is negligible as there hasn't been an infection since 1985 when techniques were developed to kill off viruses including HIV. The factor IX concentrate carries the additional hazard of thrombogenicity.
Crystalloid, colloid solutions containing human serum albumin or plasma protein fraction, hydroxyethyl starch, and dextran are preferable to FFP for volume replacement. The practice of administering both packed red cells and FFP to the same patient should be discouraged, as this adds to the cost and doubles the infection rate. When conditions are appropriate, whole blood should be given.
For nutritional support, amino acid solutions and dextrose are available.The most important alternative to the use of FFP is a comprehensive program of blood conservation. This includes measures such as autologous donation before elective surgery, the infusion of shed blood, and the realization that in many patients normovolemic anemia is not an indication for transfusion.
References
- 1 2 3 4 5 6 7 Shaz, Beth H.; Hillyer, Christopher D.; Roshal, Mikhail; Abrams, Charles S. (2013). Transfusion Medicine and Hemostasis: Clinical and Laboratory Aspects. Newnes. pp. 209–212. ISBN 9780123977885. Archived from the original on 2017-09-23.
- 1 2 3 4 5 "Plasma Intravenous Advanced Patient Information - Drugs.com". www.drugs.com. Archived from the original on 11 January 2017. Retrieved 10 January 2017.
- 1 2 3 4 5 6 British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 172. ISBN 9780857111562.
- ↑ "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- ↑ Yentis, Steven M.; Hirsch, Nicholas P.; Ip, James (2013). Anaesthesia and Intensive Care A-Z: An Encyclopedia of Principles and Practice. Elsevier Health Sciences. p. 147. ISBN 9780702053757. Archived from the original on 2017-09-23.
- ↑ Sally V. Rudmann (18 February 2005). Textbook of blood banking and transfusion medicine. Elsevier Health Sciences. pp. 247–. ISBN 978-0-7216-0384-1. Archived from the original on 30 May 2013. Retrieved 16 November 2010.
- ↑ "Fresh Frozen Plasma: Is it beneficial?". Archived from the original on November 25, 2011. Retrieved October 3, 2011.
- ↑ Mumford, Andrew D.; Ackroyd, Sam; Alikhan, Raza; Bowles, Louise; Chowdary, Pratima; Grainger, John; Mainwaring, Jason; Mathias, Mary; O'Connell, Niamh (2014-11-01). "Guideline for the diagnosis and management of the rare coagulation disorders". British Journal of Haematology. 167 (3): 304–326. doi:10.1111/bjh.13058. ISSN 1365-2141. PMID 25100430. Archived from the original on 2016-04-19.
- 1 2 Keeling, David; Baglin, Trevor; Tait, Campbell; Watson, Henry; Perry, David; Baglin, Caroline; Kitchen, Steve; Makris, Michael; British Committee for Standards in Haematology (2011-08-01). "Guidelines on oral anticoagulation with warfarin – fourth edition". British Journal of Haematology. 154 (3): 311–324. doi:10.1111/j.1365-2141.2011.08753.x. ISSN 1365-2141. PMID 21671894. Archived from the original on 2016-04-21.
- ↑ "Society for the Advancement of Blood Management | Choosing Wisely". www.choosingwisely.org. Retrieved 1 August 2018.
Further reading
- British Committee for Standards in Haematology, Blood Transfusion Task Force (J. Duguid, Chairman); O'Shaughnessy, D. F.; Atterbury, C.; Bolton Maggs, P.; Murphy, M.; Thomas, D.; Yates, S.; Williamson, L. M. (1 July 2004). "Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant". British Journal of Haematology. 126 (1): 11–28. doi:10.1111/j.1365-2141.2004.04972.x. ISSN 1365-2141. Retrieved 3 October 2016.