Dialectical behavior therapy

Dialectical behavior therapy (DBT) is an evidence-based[1] psychotherapy designed to help people suffering from borderline personality disorder (BPD). It has also been used to treat mood disorders as well as those who need to change patterns of behavior that are not helpful, such as self-harm, suicidal ideation, and substance abuse.[2] This approach works towards helping people increase their emotional and cognitive regulation by learning about the triggers that lead to reactive states and helping to assess which coping skills to apply in the sequence of events, thoughts, feelings, and behaviors to help avoid undesired reactions.
A modified form of cognitive behavioral therapy (CBT), DBT was developed in the late 1980s by Marsha M. Linehan,[3] a psychology researcher at the University of Washington, to treat people with borderline personality disorder and chronically suicidal individuals. Research on its effectiveness in treating other conditions has been fruitful;[4] DBT has been used to treat people with depression, drug and alcohol problems,[5] post-traumatic stress disorder (PTSD),[6] traumatic brain injuries (TBI), binge-eating disorder,[1] and mood disorders.[7][8] Research indicates DBT might help patients with symptoms and behaviors associated with spectrum mood disorders, including self-injury.[9] Recent work also suggests its effectiveness with sexual abuse survivors[10] and chemical dependency.[11]
DBT combines standard cognitive behavioral techniques for emotion regulation and reality-testing with concepts of distress tolerance, acceptance, and mindful awareness largely derived from Buddhist meditative practice. DBT is based upon the biosocial theory and is the first therapy that has been experimentally demonstrated to be generally effective in treating BPD.[12][13] The first randomized clinical trial of DBT showed reduced rates of suicidal gestures, psychiatric hospitalizations, and treatment drop-outs when compared to treatment as usual.[8] A meta-analysis found that DBT reached moderate effects in individuals with borderline personality disorder.[14]
Overview
Linehan observed "burn-out" in therapists after coping with "non-motivated" patients who repudiated cooperation in successful treatment. Her first core insight was to recognize that the chronically suicidal patients she studied had been raised in profoundly invalidating environments, and, therefore, required a climate of loving-kindness and somewhat unconditional acceptance (not Carl Rogers' positive humanist approach, but Thích Nhất Hạnh's metaphysically neutral one), in which to develop a successful therapeutic alliance.[note 1] Her second insight involved the need for a commensurate commitment from patients, who needed to be willing to accept their dire level of emotional dysfunction.
DBT strives to have the patient view the therapist as an ally rather than an adversary in the treatment of psychological issues. Accordingly, the therapist aims to accept and validate the client's feelings at any given time, while, nonetheless, informing the client that some feelings and behaviors are maladaptive, and showing them better alternatives.[8] DBT focuses on the client acquiring new skills and changing their behaviors,[15] with the ultimate goal of achieving a "life worth living", as defined by the patient.[16]
In DBT's biosocial theory of BPD, clients have a biological predisposition for emotional dysregulation, and their social environment validates maladaptive behavior.[17]
Linehan and others combined a commitment to the core conditions of acceptance and change through the principle of dialectics (in which thesis + antithesis → synthesis) and assembled an array of skills for emotional self-regulation drawn from Western psychological traditions, such as cognitive behavioral therapy and an interpersonal variant, "assertiveness training", and Eastern meditative traditions, such as Buddhist mindfulness meditation. One of her contributions was to alter the adversarial nature of the therapist-client relationship in favor of an alliance based on intersubjective tough love.
All DBT can be said to involve 4 components:
- Individual – The therapist and patient discuss issues that come up during the week (recorded on diary cards) and follow a treatment target hierarchy. Self-injurious and suicidal behaviors, or life-threatening behaviors, take first priority. Second in priority are behaviors which, while not directly harmful to self or others, interfere with the course of treatment. These behaviors are known as therapy-interfering behaviors. Third in priority are quality of life issues and working towards improving one's life generally. During the individual therapy, the therapist and patient work towards improving skill use. Often, a skills group is discussed and obstacles to acting skillfully are addressed.
- Group – A group ordinarily meets once weekly for two to two and a half hours and learns to use specific skills that are broken down into four skill modules: core mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance.
- Therapist Consultation Team – A therapist consultation team includes all therapists providing DBT. The meeting occurs weekly and serves to support the therapist in providing the treatment.
- Phone Coaching – Phone coaching is designed to help generalize skills into the patient's daily life. Phone coaching is brief and limited to a focus on skills.
No one component is used by itself; the individual component is considered necessary to keep suicidal urges or uncontrolled emotional issues from disrupting group sessions, while the group sessions teach the skills unique to DBT, and also provide practice with regulating emotions and behavior in a social context. DBT skills training alone is being used to address treatment goals in some clinical settings,[18] and the broader goal of emotion regulation that is seen in DBT has allowed it to be used in new settings, for example, supporting parenting.[19]
Four modules
Mindfulness
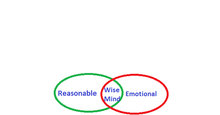
Mindfulness is one of the core ideas behind all elements of DBT. It is considered a foundation for the other skills taught in DBT, because it helps individuals accept and tolerate the powerful emotions they may feel when challenging their habits or exposing themselves to upsetting situations. The concept of mindfulness and the meditative exercises used to teach it are derived from traditional Buddhist practice, though the version taught in DBT does not involve any religious or metaphysical concepts. Within DBT it is the capacity to pay attention, nonjudgmentally, to the present moment; about living in the moment, experiencing one's emotions and senses fully, yet with perspective. The practice of mindfulness can also be intended to make people more aware of their environments through their 5 senses: touch, smell, sight, taste, and sound.[20] Mindfulness relies heavily on the principle of acceptance, sometimes referred to as "radical acceptance".[4] Acceptance skills rely on the patient’s ability to view situations with no judgment, and to accept situations and their accompanying emotions.[4] This causes less distress overall, which can result in reduced discomfort and symptomology.
Acceptance and Change
The first few sessions of DBT introduce the dialectic of acceptance and change. The patient must first become comfortable with the idea of therapy; once the patient and therapist have established a trusting relationship, DBT techniques can flourish. An essential part of learning acceptance is to first grasp the idea of radical acceptance: radical acceptance embraces the idea that one should face situations, both positive and negative, without judgment.[21] Acceptance also incorporates mindfulness and emotional regulation skills, which depend on the idea of radical acceptance. These skills, specifically, are what set DBT apart from other therapies.
Often, after a patient becomes familiar with the idea of acceptance, they will accompany it with change. DBT has five specific states of change which the therapist will review with the patient: precontemplation, contemplation, preparation, action, and maintenance[22]. Precontemplation is the first stage, in which the patient is completely unaware of their problem. In the second stage, contemplation, the patient realizes the reality of their illness: this is not an action, but a realization. It is not until the third stage, preparation, that the patient is likely to take action, and prepares to move forward. This could be as simple as researching or contacting therapists. Finally, in stage 4, the patient takes action and receives treatment. In the final stage, maintenance, the patient must strengthen their change in order to prevent relapse. After grasping acceptance and change, a patient can fully advance to mindfulness techniques.
"What" skills
- Observe
- This is used to nonjudgmentally observe one's environment within or outside oneself. It is helpful in understanding what is going on in any given situation.
- DBT recommends developing a "teflon mind", the ability to let feelings and experiences pass without sticking in the mind.[23]
- Describe
- This is used to express what one has observed with the observe skill. It is to be used without judgmental statements. This helps with letting others know what one has observed. Once the environment or inner state of mind has been observed with 5 senses, the individual can put words to observations and thus better understand the environment.[24]
- Participate
- This is used to become fully focused on, and involved in, the activity that one is doing.
"How" skills
How to do Mindful Meditation. There are many "scripted" meditations available on YouTube; for example: The 3 Minute Meditation; or The Body Scan. How to do it (The Body Scan): You listen to the body scan and you allow your mind to focus on each aspect of your physical self, usually starting at your toes and ending at the top of your head. As you listen to the body scan and allow your mind to focus in on the body, you will notice your "busy mind" will come into consciousness. You will notice that thoughts and feelings will attempt to distract you from focusing on each part of your body. You will notice that some of the thoughts and feelings may be distressing to you. You may want to stop the meditation because it might be very painful emotionally or physically or because you are having negative or busy thoughts. Sometimes memories may surface and they may also be difficult emotionally to accept. How to do Mindful Meditation involves learning to acknowledge the thoughts, feelings and memories without needing to fight them or chase them away. The paradox: If we try to fight them, they seem to get bigger; but when we move into acceptance, they seem to get smaller. We enter the mindfulness meditation body scan, 3 minute meditation or other meditation sessions with no goals and with a non-striving stance. Again, if we enter with a goal to "fix my problems by meditating", that goal and pressure to fix something tends to make the problems bigger. To enter the meditation with a non-goal/non-striving attitude, so having no expectations, paradoxically, usually results in a reduction of stress, pain and other symptoms.
- Nonjudgmentally
- This is the action of describing the facts, and not thinking in terms of "good" or "bad," "fair," or "unfair." These are judgments, not factual descriptions. Being nonjudgmental helps you to get your point across in an effective manner without adding a judgment that someone else might disagree with.
- One-mindfully
- This is used to focus on one thing. One-mindfully is helpful in keeping one's mind from straying into "emotion" by a lack of focus.
- Effectively
- This is simply doing what works. It is a very broad-ranged skill and can be applied to any other skill to aid in being successful with said skill.[25]
Distress tolerance
Many current approaches to mental health treatment focus on changing distressing events and circumstances such as dealing with the death of a loved one, loss of a job, serious illness, terrorist attacks and other traumatic events.[26] They have paid little attention to accepting, finding meaning for, and tolerating distress. This task has generally been tackled by psychodynamic, psychoanalytic, gestalt, or narrative therapies, along with religious and spiritual communities and leaders. Dialectical behavior therapy emphasizes learning to bear pain skillfully.
Distress tolerance skills constitute a natural development from DBT mindfulness skills. They have to do with the ability to accept, in a non-evaluative and nonjudgmental fashion, both oneself and the current situation. Since this is a non-judgmental stance, this means that it is not one of approval or resignation. The goal is to become capable of calmly recognizing negative situations and their impact, rather than becoming overwhelmed or hiding from them. This allows individuals to make wise decisions about whether and how to take action, rather than falling into the intense, desperate, and often destructive emotional reactions that are part of borderline personality disorder.[25]
- Distract with ACCEPTS
- This is a skill used to distract oneself temporarily from unpleasant emotions.
- Activities – Use positive activities that you enjoy.
- Contribute – Help out others or your community.
- Comparisons – Compare yourself either to people that are less fortunate or to how you used to be when you were in a worse state.
- Emotions (other) – cause yourself to feel something different by provoking your sense of humor or happiness with corresponding activities.
- Push away – Put your situation on the back-burner for a while. Put something else temporarily first in your mind.
- Thoughts (other) – Force your mind to think about something else.
- Sensations (other) – Do something that has an intense feeling other than what you are feeling, like a cold shower or a spicy candy.[25]
- Self-soothe
- This is a skill in which one behaves in a comforting, nurturing, kind, and gentle way to oneself. You use it by doing something that is soothing to you. It is used in moments of distress or agitation.[25] New York Jets wide receiver Brandon Marshall, who was diagnosed with BPD in 2011 and is a strong advocate for DBT, cited activities such as prayer and listening to jazz music as instrumental in his treatment.
- IMPROVE the moment
- This skill is used in moments of distress to help one relax.
- Imagery – Imagine relaxing scenes, things going well, or other things that please you.
- Meaning – Find some purpose or meaning in what you are feeling.
- Prayer – Either pray to whomever you worship, or, if not religious, chant a personal mantra.
- Relaxation – Relax your muscles, breathe deeply; use with self-soothing.
- One thing in the moment – Focus your entire attention on what you are doing right now. Keep yourself in the present.
- Vacation (brief) – Take a break from it all for a short period of time.
- Encouragement – Cheerlead yourself. Tell yourself you can make it through this and cope as it will assist your resilience and reduce your vulnerability.[25]
- Pros and cons
- Think about the positive and negative things about not tolerating distress.[25]
- Radical acceptance
- Let go of fighting reality. Accept your situation for what it is.[25]
- Turning the mind
- Turn your mind toward an acceptance stance. It should be used with radical acceptance.[25]
- Willingness vs. willfulness
- Be willing and open to do what is effective. Let go of a willful stance which goes against acceptance. Keep your eye on the goal in front of you.[25]
Emotion regulation
Individuals with borderline personality disorder and suicidal individuals are frequently emotionally intense and labile. They can be angry, intensely frustrated, depressed, or anxious. This suggests that these clients might benefit from help in learning to regulate their emotions. Dialectical behavior therapy skills for emotion regulation include:[27][28]
- Identify and label emotions
- Identify obstacles to changing emotions
- Reduce vulnerability to emotion mind
- Increase positive emotional events
- Increase mindfulness to current emotions
- Take opposite action
- Apply distress tolerance techniques[25]
Emotional regulation skills are based on the theory that intense emotions are a conditioned response to troublesome experiences, the conditioned stimulus, and therefore, are required to alter the patient’s conditioned response.[4] These skills can be categorized into four modules: understanding and naming emotions, changing unwanted emotions, reducing vulnerability, and managing extreme conditions.[4]
In learning how to understand and name emotions, the patient focuses on recognizing their feelings. This segment relates directly to mindfulness, which also exposes a patient to their emotions. In changing unwanted emotions, the therapist emphasizes the use of opposite-reactions, fact-checking, and problem solving to regulate emotions. In changing unwanted emotions, the therapist emphasizes the use of opposite-reactions, fact-checking, and problem solving to regulate emotions. While using opposite-reactions, the patient targets distressing feelings by responding with the opposite emotion. In reducing vulnerability, the patient learns to accumulate positive emotions and to plan coping mechanisms in advance, in order to better handle difficult experiences in the future. In managing extreme conditions, the patient focuses on incorporating their use of mindfulness skills to their current emotions, in order to remain stable and alert in a crisis situation.[4]
Story of emotion
- This skill is used to understand what kind of emotion one is feeling.
- Prompting event
- Interpretation of the event
- Body sensations
- Body language
- Action urge
- Action
- Emotion name, based on previous items on list[25]
PLEASE
- This skill concerns ineffective health habits can make one more vulnerable to emotion mind. This skill is used to maintain a healthy body, so one is more likely to have healthy emotions.
- PhysicaL illness (treat) – If you are sick or injured, get proper treatment for it.
- Eating (balanced) – Make sure you eat a proper healthy diet, and eat in moderation.
- Avoid mood-altering drugs – Do not take other non-prescribed medication or drugs. They may be very harmful to your body, and can make your mood unpredictable.
- Sleep (balanced) – Do not sleep too much or too little. Eight hours of sleep is recommended per night for the average adult.
- Exercise – Make sure you get an effective amount of exercise, as this will both improve body image and release endorphins, making you happier.[25]
Build mastery
- Try to do one thing a day to help build competence and control.[25]
Opposite action
- This skill is used when you have an unjustified emotion, one that doesn't belong in the situation at hand. You use it by doing the opposite of your urges in the moment. It is a tool to bring you out of an unwanted or unjustified emotion by replacing it with the emotion that is opposite.[25]
Problem solving
- This is used to solve a problem when your emotion is justified. It is used in combination with other skills.[25]
Letting go of emotional suffering
- Observe and experience your emotion, accept it, then let it go.[25]
Interpersonal effectiveness
Interpersonal response patterns taught in DBT skills training are very similar to those taught in many assertiveness and interpersonal problem-solving classes. They include effective strategies for asking for what one needs, saying no, and coping with interpersonal conflict.
Individuals with borderline personality disorder frequently possess good interpersonal skills in a general sense. The problems arise in the application of these skills to specific situations. An individual may be able to describe effective behavioral sequences when discussing another person encountering a problematic situation, but may be completely incapable of generating or carrying out a similar behavioral sequence when analyzing their own situation.
The interpersonal effectiveness module focuses on situations where the objective is to change something (e.g., requesting that someone do something) or to resist changes someone else is trying to make (e.g., saying no). The skills taught are intended to maximize the chances that a person's goals in a specific situation will be met, while at the same time not damaging either the relationship or the person's self-respect.
- DEEAR MAN – conveying one's needs to another person
- This acronym is used to aid one in getting what one wants when asking.
- Describe one's situation using specific factual statements about a recent situation.
- Express the emotions experienced when the situation occurred, why this is an issue and how one feels about it.
- Empathy acknowledge what the other person experienced and their emotions
- Assert one's self by asking clearly and specifically for what behavior change the person seeks.
- Reinforce one's position by offering a positive consequence if one were to get what one wants.
- Mindful of the situation by focusing on what one wants and disregard distractions through validation/empathy and redirecting back to the point.
- Appear confident and assertive, even if one doesn't feel confident.
- Negotiate with a hesitant person and come to a comfortable compromise on one's request.
- GIVE – giving something
- This skill set aids one maintaining one's relationships, whether they are with friends, co-workers, family, romantic partners, etc. It is to be used in conversations.
- Gentle: Use appropriate language, no verbal or physical attacks, no put downs, avoid sarcasm unless one is sure the person is alright with it, and be courteous and non-judgmental.
- Interested: When the person one is speaking to is talking about something, act interested in what is being said. Maintain eye contact, ask questions, etc. Avoid the use of a cell phone during an in-person conversation.
- Validate: Show understanding and sympathy of a person's situation. Validation can be shown through words, body language and/or facial expressions.
- Easy Manner: Be calm and comfortable during conversation; use humor; smile.
- FAST – keeping self-respect
- This is a skill to aid one in maintaining one's self-respect. It is to be used in combination with the other interpersonal effectiveness skills.
- Fair: Be fair to both oneself and the other person.
- Apologies (few): Don't apologize more than once for what one has done ineffectively or for something that was ineffective.
- Stick to One's Values: Stay true to what one believes in and stand by it. Don't allow others to encourage action against one's own values.
- Truthful: Don't lie. Lying can only pile up and damage relationships and one's self-respect.[25]
This list does not include the "problem solving" module, the purpose of which is to practice being one's own therapist.
Tools
Diary cards
Specially formatted cards for tracking therapy interfering behaviors that distract or hinder a patient's progress. Diary cards can be filled out daily, 2–3 times a day, or once per week.
Chain analysis
Chain analysis is a form of functional analysis of behavior but with increased focus on sequential events that form the behavior chain. It has strong roots in behavioral psychology in particular applied behavior analysis concept of chaining.[29] A growing body of research supports the use of behavior chain analysis with multiple populations.[30]
Milieu
The milieu, or the culture of the group involved, plays a key role in the effectiveness of DBT.
Efficacy
Borderline personality disorder
DBT is the therapy that has been studied the most for treatment of borderline personality disorder, and there have been enough studies done to conclude that DBT is helpful in treating borderline personality disorder.[31] A 2009 Canadian study compared the treatment of borderline personality disorder with dialectical behavior therapy against general psychiatric management. A total of 180 adults, 90 in each group, were admitted to the study and treated for an average of 41 weeks. Statistically significant decreases in suicidal events and non-suicidal self-injurious events were seen overall (48% reduction, p=0.03; and 77% reduction, p=0.01; respectively). No statistically-significant difference between groups were seen for these episodes (p=.64). Emergency department visits decreased by 67% (p<0.0001) and emergency department visits for suicidal behavior by 65% (p<0.0001), but there was also no statistically significant difference between groups.[32]
Depression
A Duke University study of compared treatment of depression by antidepressant medication to treatment by antidepressants and dialectical behavior therapy. A total of 34 chronically depressed individuals over age 60 were treated for 28 weeks. Six months after treatment, statistically-significant differences were noted in remission rates between groups, with a greater percentage of patients treated with antidepressants and dialectical behavior therapy in remission.[33]
See also
Notes
- ↑ Described by Thích Nhất Hạnh in his second moral precept of Zen Buddhism as loving kindness.
References
- 1 2 Chapman, AL (2006). "Dialectical behavior therapy: current indications and unique elements". Psychiatry (Edgmont). 3 (9): 62–8. PMC 2963469. PMID 20975829.
- ↑ "An Overview of Dialectical Behavior Therapy – Psych Central". 17 May 2016. Retrieved 2015-01-19.
- ↑ "What is DBT?". The Linehan Institute. Retrieved 2015-08-29.
- 1 2 3 4 5 6 Linehan, Marsha M. (2014). "DBT Skills Training Manual" (PDF). www.guilford.com (2nd ed.). Guilford Press. Retrieved 11 December 2016.
- ↑ Dimeff, LA; Linehan, MM (2008). "Dialectical behavior therapy for substance abusers". Addict Sci Clin Pract. 4 (2): 39–47. doi:10.1151/ascp084239. PMC 2797106. PMID 18497717.
- ↑ "What is Dialectical Behavior Therapy (DBT)? – Behavioral Tech". behavioraltech.org.
- ↑ Janowsky, David S. (1999). Psychotherapy indications and outcomes. Washington, DC: American Psychiatric Press. p. 100. ISBN 0-88048-761-5.
- 1 2 3 Linehan, M. M.; Dimeff, L. (2001). "Dialectical Behavior Therapy in a nutshell" (PDF). The California Psychologist. 34: 10–13.
- ↑ Brody, J. E. (2008, May 6). The growing wave of teenage self-harm. New York Times. Retrieved July 1, 2008.
- ↑ Decker, S.E.; Naugle, A.E. (2008). "DBT for Sexual Abuse Survivors: Current Status and Future Directions" (PDF). Journal of behavior Analysis of Offender and Victim: Treatment and Prevention. 1 (4): 52–69. Archived from the original (PDF) on 2010-12-29.
- ↑ Linehan, Marsha M.; Schmidt, Henry III; Dimeff, Linda A.; Craft, J. Christopher; Kanter, Jonathan; Comtois, Katherine A. (1999). "Dialectical Behavior Therapy for Patients with Borderline Personality Disorder and Drug-Dependence" (PDF). The American Journal on Addictions. pp. 279–292. Retrieved 2014-03-31.
- ↑ Linehan, M. M.; Armstrong, H. E.; Suarez, A.; Allmon, D.; Heard, H. L. (1991). "Cognitive-behavioral treatment of chronically parasuicidal borderline patients". Archives of General Psychiatry. 48 (12): 1060–64. doi:10.1001/archpsyc.1991.01810360024003.
- ↑ Linehan, M. M.; Heard, H. L.; Armstrong, H. E. (1993). "Naturalistic follow-up of a behavioural treatment of chronically parasuicidal borderline patients". Archives of General Psychiatry. 50 (12): 971–974. doi:10.1001/archpsyc.1993.01820240055007. PMID 8250683.
- ↑ Kliem, S.; Kröger, C. & Kossfelder, J. (2010). "Dialectical behavior therapy for borderline personality disorder: A meta-analysis using mixed-effects modeling". Journal of Consulting and Clinical Psychology. 78 (6): 936–951. doi:10.1037/a0021015. PMID 21114345.
- ↑ Choi-Kain, Lois W.; Finch, Ellen F.; Masland, Sara R.; Jenkins, James A.; Unruh, Brandon T. (3 February 2017). "What Works in the Treatment of Borderline Personality Disorder". Current Behavioral Neuroscience Reports. 4 (1): 21–30. doi:10.1007/s40473-017-0103-z. PMC 5340835. PMID 28331780.
- ↑ "What is Dialectical Behavior Therapy (DBT)?". Behavioral Tech. Retrieved 30 November 2017.
- ↑ Little, Hannah; Tickle, Anna; das Nair, Roshan (16 October 2017). "Process and impact of dialectical behaviour therapy: A systematic review of perceptions of clients with a diagnosis of borderline personality disorder". Psychology and Psychotherapy: Theory, Research and Practice. doi:10.1111/papt.12156. PMID 29034599.
- ↑ Valentine, Sarah E.; Bankoff, Sarah M.; Poulin, Renée M.; Reidler, Esther B.; Pantalone, David W. (January 2015). "The Use of Dialectical Behavior Therapy Skills Training as Stand-Alone Treatment: A Systematic Review of the Treatment Outcome Literature". Journal of Clinical Psychology. 71 (1): 1–20. doi:10.1002/jclp.22114.
- ↑ Zalewski, Maureen; Lewis, Jennifer K; Martin, Christina Gamache (June 2018). "Identifying novel applications of dialectical behavior therapy: considering emotion regulation and parenting". Current Opinion in Psychology. 21: 122–126. doi:10.1016/j.copsyc.2018.02.013. PMID 29529427.
- ↑ "What is Mindfulness? – The Linehan Institute". www.linehaninstitute.org. Retrieved 2017-09-21.
- ↑ Linehan, Marsha M. (2014). "DBT Skills Training Manual" (PDF). www.guilford.com (2nd ed.). Guilford Press. Retrieved 11 December 2016.
- ↑ Ellen., Astrachan-Fletcher, (2009). The dialectical behavior therapy skills workbook for bulimia using DBT to break the cycle and regain control of your life. New Harbinger Publications. ISBN 9781608822560. OCLC 955646721.
- ↑ Young, Kathleen (2010-03-11), "Mindfulness and DBT: "What skills"", Dr. Kathleen Young: Treating Trauma in Tucson
- ↑ "Core Mindfulness in Dialectical Behavior Therapy". GoodTherapy.org Therapy Blog. 2013-02-15. Retrieved 2017-09-21.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Lisa Dietz (2003). "DBT Skills List". Retrieved 2010-04-26.
- ↑ ""Road To Resiliance" Article: What is resilience?". American Psychological Association.
- ↑ Stone, M.H. (1987) In A. Tasman, R. E. Hales, & A. J. Frances (eds.), American Psychiatric Press review of psychiatry (vol. 8, pp. 103–122). Washington DC: American Psychiatric Press.
- ↑ Holmes, P.; Georgescu, S. & Liles, W. (2005). "Further delineating the applicability of acceptance and change to private responses: The example of dialectical behavior therapy" (PDF). The Behavior Analyst Today. 7 (3): 301–311.
- ↑ Sampl, S.; Wakai, S.; Trestman, R. & Keeney, E.M. (2008). "Functional Analysis of Behavior in Corrections: Empowering Inmates in Skills Training Groups" (PDF). Journal of Behavior Analysis of Offender and Victim: Treatment and Prevention. 1 (4): 42–51. doi:10.1037/h0100455.
- ↑ "Self Awareness and Insight Through Dialectical Behavior Therapy: The Chain Analysis". www.parkslopetherapy.net.
- ↑ Stoffers, JM; Völlm, BA; Rücker, G; Timmer, A; Huband, N; Lieb, K (15 August 2012). "Psychological therapies for people with borderline personality disorder" (PDF). The Cochrane Database of Systematic Reviews. 8 (8): CD005652. doi:10.1002/14651858.CD005652.pub2. PMID 22895952.
- ↑ McMain, Shelley (1 December 2009). "A Randomized Trial of Dialectical Behavior Therapy Versus General Psychiatric Management for Borderline Personality Disorder". American Journal of Psychiatry. 166 (12): 1365–1374. doi:10.1176/appi.ajp.2009.09010039. Retrieved 16 November 2017.
- ↑ Lynch, Thomas (January–February 2003). "Dialectical Behavior Therapy for Depressed Older Adults: A Randomized Pilot Study". The American Journal of Geriatric Psychiatry. 11 (1): 33–45. doi:10.1097/00019442-200301000-00006. PMID 12527538.
Sources
- Linehan, M.M.; Comtois, K.A.; Murray, A.M.; Brown, M.Z.; Gallop, R.J.; Heard, H.L.; Korslund, K.E.; Tutek, D.A.; Reynolds, S.K.; Lindenboim, N. (2006). "Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder". Arch Gen Psychiatry. 63 (7): 757–66. doi:10.1001/archpsyc.63.7.757. PMID 16818865.
- Linehan, M.M.; Heard, H.L. (1993). ""Impact of treatment accessibility on clinical course of parasuicidal patients": Reply". Archives of General Psychiatry. 50 (2): 157–158. doi:10.1001/archpsyc.1993.01820140083011.
- Linehan, M.M.; Tutek, D.A.; Heard, H.L.; Armstrong, H.E. (1994). "Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients". American Journal of Psychiatry. 151 (12): 1771–1776. doi:10.1176/ajp.151.12.1771.
- Linehan, M.M.; Schmidt, H.; Dimeff, L.A.; Craft, J.C.; Kanter, J.; Comtois, K.A. (1999). "Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence". American Journal on Addiction. 8 (4): 279–292. doi:10.1080/105504999305686.
- Linehan, M.M.; Dimeff, L.A.; Reynolds, S.K.; Comtois, K.A.; Welch, S.S.; Heagerty, P.; Kivlahan, D.R. (2002). "Dialectical behavior therapy versus comprehensive validation plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder". Drug and Alcohol Dependence. 67 (1): 13–26. doi:10.1016/s0376-8716(02)00011-x. PMID 12062776.
- Koons, C.R.; Robins, C.J.; Tweed, J.L.; Lynch, T.R.; Gonzalez, A.M.; Morse, J.Q.; Bishop, G.K.; Butterfield, M.I.; Bastian, L.A. (2001). "Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder". Behavior Therapy. 32 (2): 371–390. doi:10.1016/s0005-7894(01)80009-5.
- van den Bosch, L.M.C.; Verheul, R.; Schippers, G.M.; van den Brink, W. (2002). "Dialectical Behavior Therapy of borderline patients with and without substance use problems: Implementation and long-term effects". Addictive Behaviors. 27 (6): 911–923. doi:10.1016/s0306-4603(02)00293-9.
- Verheul, R.; van den Bosch, L.M.C.; Koeter, M.W.J.; de Ridder, M.A.J.; Stijnen, T.; van den Brink, W. (2003). "Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomised clinical trial in the Netherlands". British Journal of Psychiatry. 182 (2): 135–140. doi:10.1192/bjp.182.2.135.
- Linehan et al. (2006) NIMH 3 Two-Year Randomized Control Trial and Follow up of DBT
- Amy Lopez LCSW, Cheryl A. Chessick MD. (2013) DBT Graduate Group Pilot Study: A Model to Generalize Skills to Create a “Life Worth Living”. Social Work in Mental Health 11:2, pages 141-153.
Further reading
- The Miracle of Mindfulness by Thích Nhất Hạnh. ISBN 0-8070-1239-4.
- Skills Training Manual for Treating Borderline Personality Disorder by Marsha M. Linehan. 1993. ISBN 0-89862-034-1.
- Cognitive Behavioral Treatment of Borderline Personality Disorder by Marsha M. Linehan. 1993. ISBN 0-89862-183-6.
- Fatal Flaws: Navigating Destructive Relationships with People with Disorders of Personality and Character by Stuart C. Yudovsky. ISBN 1-58562-214-1.
- The High Conflict Couple: A Dialectical Behavior Therapy Guide to Finding Peace, Intimacy, & Validation by Alan E. Fruzzetti. ISBN 1-57224-450-X.
- Dialectical Behavior Therapy with Suicidal Adolescents by Alec L. Miller, Jill H. Rathus, and Marsha M. Linehan. Foreword by Charles R. Swenson. ISBN 978-1-59385-383-9.
- Dialectical Behavior Therapy Workbook: Practical DBT Exercises for Learning Mindfulness, Interpersonal Effectiveness, Emotion Regulation, & Distress Tolerance (New Harbinger Self-Help Workbook) by Matthew McKay, Jeffrey C. Wood, and Jeffrey Brantley. ISBN 978-1-57224-513-6.
- Don't Let Your Emotions Run Your Life: How Dialectical Behavior Therapy Can Put You in Control (New Harbinger Self-Help Workbook) by Scott E. Spradlin. ISBN 978-1-57224-309-5.
- Depressed and Anxious: The Dialectical Behavior Therapy Workbook for Overcoming Depression & Anxiety by Thomas Marra. ISBN 978-1-57224-363-7.
External links
| Wikibooks has a book on the topic of: Dialectical Behavioral Therapy |