Urinary bladder
The urinary bladder or simply bladder is a hollow muscular organ in humans and vertebrates that collects and stores urine from the kidneys before disposal by urination. In the human the bladder is a hollow muscular, and distensible (or elastic) organ, that sits on the pelvic floor. Urine enters the bladder via the ureters and exits via the urethra. The typical human bladder will hold between 300 and 500 mL (10.14 and 16.91 fl oz) before the urge to empty occurs, but can hold considerably more.[1][2]
| Urinary bladder | |
|---|---|
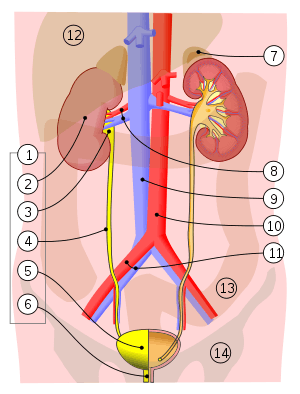 1. Human urinary system: 2. Kidney, 3. Renal pelvis, 4. Ureter, 5. Urinary bladder, 6. Urethra. (Left side with frontal section) 7. Adrenal gland Vessels: 8. Renal artery and vein, 9. Inferior vena cava, 10. Abdominal aorta, 11. Common iliac artery and vein With transparency: 12. Liver, 13. Large intestine, 14. Pelvis | |
| Details | |
| Precursor | urogenital sinus |
| System | Urinary system |
| Artery | Superior vesical artery Inferior vesical artery Umbilical artery Vaginal artery |
| Vein | Vesical venous plexus |
| Nerve | Vesical nervous plexus |
| Identifiers | |
| Latin | vesica urinaria |
| MeSH | D001743 |
| TA | A08.3.01.001 |
| FMA | 15900 |
| Anatomical terminology | |
Structure
In humans, the bladder is a hollow muscular organ situated at the base of the pelvis. Urine collects in the bladder, fed from the two ureters that connect the bladder with the kidneys. Urine leaves the bladder via the urethra, a single muscular tube ending in an opening – the urinary meatus, where it exits the body.
Anatomists divide the bladder into:.[3]
- a broad fundus
- a body
- an apex
- a neck
The apex (prev.vertex) is directed forward toward the upper part of the pubic symphysis, and from there the median umbilical ligament continues upward on the back of the anterior abdominal wall to the umbilicus. The peritoneum is carried by it from the apex on to the abdominal wall to form the middle umbilical fold.
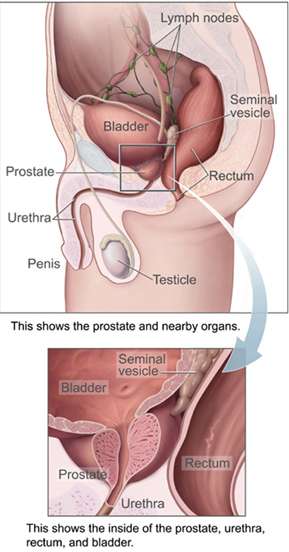
The neck of the bladder is the area at the base of the trigone that surrounds the internal urethral orifice that leads to the urethra.[3] In males the neck of the urinary bladder is adjacent to the prostate gland.
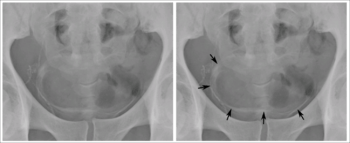
The three openings, two ureteric orifices, and the internal urethral orifice mark the triangular area called the trigone of the bladder. These openings have mucosal flaps in front of them that act as valves in preventing the backflow of urine into the ureters,[4] known as vesicoureteral reflux. Between the two ureteric openings is a raised area of tissue called the interureteric crest.[3] This makes the upper boundary of the trigone. The trigone is a smooth-muscle area that forms the floor of the bladder above the urethra.[5] It is an area of smooth tissue for the easy flow of urine into and from this part of the bladder - in contrast to the irregular surface formed by the rugae.
In men, the prostate gland lies outside the opening for the urethra. The middle lobe of the prostate causes an elevation in the mucous membrane behind the internal urethral orifice called the uvula of urinary bladder. The uvula can enlarge when the prostate becomes enlarged.
The bladder is situated below the peritoneal cavity near the pelvic floor and behind the pubic symphysis. In men, it lies in front of the rectum, separated by the recto-vesical pouch, and is supported by fibres of the levator ani and of the prostate gland. In women, it lies in front of the uterus, separated by the vesico-uterine pouch, and is supported by the elevator ani and the upper part of the vagina. The wall of the urinary bladder is normally 3–5 mm thick.[6] When well distended, the wall is normally less than 3 mm.[6]
The inner walls have a series of ridges, thick mucosal folds known as rugae that allow for the expansion of the bladder.
The Latin phrase for "urinary bladder" is vesica urinaria, and the term vesical or prefix vesico - appear in connection with associated structures such as vesical veins. The modern Latin word for "bladder" – cystis – appears in associated terms such as cystitis (inflammation of the bladder).
Microanatomy
The outside of the bladder is protected by a serous membrane.[7] The bladder wall itself is smooth muscle.[7] The inner side of the bladder is lined with a mucous membrane consisting of a surface glycocalyx that protects the cells beneath it from urine, the urothelium (a form of transitional epithelium), a basement membrane, and the lamina propria.[8][7][9] The mucosal lining also offers a urothelial barrier against the passing of infections.[10]
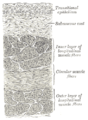 Vertical section of bladder wall
Vertical section of bladder wall- Layers of the urinary bladder wall and cross-section of the detrusor muscle
 Anatomy of the male bladder, showing transitional epithelium and part of the wall in a histological cut-out
Anatomy of the male bladder, showing transitional epithelium and part of the wall in a histological cut-out
Detrusor muscle
The detrusor muscle is a layer of the urinary bladder wall made of smooth muscle fibers arranged in spiral, longitudinal, and circular bundles.
Stretch receptors in the bladder signal the parasympathetic nervous system to stimulate the muscarinic receptors in the detrusor to contract the muscle when the bladder is extended.[11] This encourages the bladder to expel urine through the urethra. The main receptor activated is the M3 receptor, although M2 receptors are also involved and whilst outnumbering the M3 receptors they are not so responsive.[12]
The main relaxant pathway is via the adenylyl cyclase cAMP pathway, activated via the β3 adrenergic receptors. The β2 adrenergic receptors are also present in the detrusor and even outnumber β3 receptors, but they do not have as important an effect in relaxing the detrusor smooth muscle.[13][14][15]
The detrusor muscle is unusually able to change its length. It can also contract for a long time whilst voiding, and it stays relaxed whilst the bladder is filling.[13] The urothelium and lamina propria (also termed the bladder mucosa) line the inside of the detrusor muscle, and can release regulators to influence general contractility of the detrusor muscle, maintain normal bladder tone, and potentially mediate bladder diseases such as overactive bladder.[16]
Blood and lymph supply
The bladder is supplied by the vesical arteries and drained by the vesical veins.[17] The superior vesical artery supplies blood to the upper part of the bladder. The lower part of the bladder is supplied by the inferior vesical artery in males and by the vaginal artery in females, both of which are branches of the internal iliac arteries.[17] In females, the uterine arteries provides additional blood supply.[17] Venous drainage begins in a network of small vessels on the lateral and posterior surfaces of the bladder, which coalesce and pass backwards along the lateral ligaments of the bladder into the internal iliac veins.[17]
The lymph drained from the bladder begins in a series of networks throughout the mucosal, muscular and serosal layers. These then form three sets of vessels: one set near the trigone draining the bottom of the bladder; one set draining the top of the bladder; and another set draining the outer undersurface of the bladder. The majority of these vessels drain into the external iliac lymph nodes.[17]
Nerve supply
The bladder receives motor innervation from both sympathetic fibers, most of which arise from the superior and inferior hypogastric plexuses and nerves, and from parasympathetic fibers, which come from the pelvic splanchnic nerves.[18]
Sensation from the bladder is transmitted to the central nervous system (CNS) via general visceral afferent fibers (GVA). GVA fibers on the superior surface follow the course of the sympathetic efferent nerves back to the CNS, while GVA fibers on the inferior portion of the bladder follow the course of the parasympathetic efferents.[18]
For the urine to exit the bladder, both the autonomically controlled internal sphincter and the voluntarily controlled external sphincter must be opened. The internal sphincter is controlled via the hypogastric nerve, predominantly through the alpha-1 receptor; the external sphincter is controlled by the pudendal nerve.[15] Problems with these sphincters can lead to incontinence.[19]
Development
The human urinary bladder derives from the urogenital sinus, and it is initially continuous with the allantois. The upper and lower parts of the bladder develop separately and join together around the middle part of development.[5] At this time the ureters move from the mesonephric ducts to the trigone.[5] In males, the base of the bladder lies between the rectum and the pubic symphysis. It is superior to the prostate, and separated from the rectum by the recto-vesical pouch. In females, the bladder sits inferior to the uterus and anterior to the vagina; thus its maximum capacity is lower than in males. It is separated from the uterus by the vesico-uterine pouch. In infants and young children the urinary bladder is in the abdomen even when empty.[20]
Function
Urine, excreted by the kidneys, collects in the bladder before disposal by urination (micturition). The urinary bladder usually holds 300–350 mL of urine. As urine accumulates, the rugae flatten and the wall of the bladder thins as it stretches, allowing the bladder to store larger amounts of urine without a significant rise in internal pressure.[21] Urination is controlled by the pontine micturition center in the brainstem.[22]
Clinical significance
Inflammation and infection
Bacteriuria is the presence of bacteria in the urine which can indicate a urinary tract infection such as cystitis.
Incontinence and retention
Frequent urination can be due to excessive urine production, small bladder capacity, irritability or incomplete emptying. Males with an enlarged prostate urinate more frequently. One definition of an overactive bladder is when a person urinates more than eight times per day.[23] An overactive bladder can often cause urinary incontinence. Though both urinary frequency and volumes have been shown to have a circadian rhythm, meaning day and night cycles,[24] it is not entirely clear how these are disturbed in the overactive bladder. Urodynamic testing can help to explain the symptoms. An underactive bladder is the condition where there is a difficulty in passing urine and is the main symptom of a neurogenic bladder. Frequent urination at night may indicate the presence of bladder stones.
Disorders of or related to the bladder include:
- Bladder exstrophy
- Bladder sphincter dyssynergia, a condition in which the sufferer cannot coordinate relaxation of the urethra sphincter with the contraction of the bladder muscles
- Paruresis
- Trigonitis
- Urinary retention
Disorders of bladder function may be dealt with surgically, by re-directing the flow of urine or by replacement with an artificial urinary bladder. The volume of the bladder may be increased by bladder augmentation. An obstruction of the bladder neck may be severe enough to warrant surgery.
Cancer

- Bladder cancer – the most common type is transitional cell carcinoma.[25]
Investigation
Urodynamic testing can help to explain the symptoms.
Other animals
Reptiles
In all reptiles, the urinogenital ducts and the anus both empty into an organ called a cloaca. In some reptiles, a midventral wall in the cloaca may open into a urinary bladder, but not all. It is present in all turtles and tortoises as well as most lizards but is lacking in the monitor lizard, the legless lizards. It is absent in the snakes, alligators, and crocodiles.[26]:p. 474
Many turtles, tortoises, and lizards have proportionally very large bladders. Charles Darwin noted that the Galapagos tortoise had a bladder which could store up to 20% of its body weight.[27] Such adaptations are the result of environments such as remote islands and deserts where water is very scarce.[28]:143 Other desert-dwelling reptiles have large bladders that can store a long-term reservoir of water for up to several months and aid in osmoregulation.[29]
Turtles have two or more accessory urinary bladders, located lateral to the neck of the urinary bladder and dorsal to the pubis, occupying a significant portion of their body cavity.[30] Their bladder is also usually bilobed with a left and right section. The right section is located under the liver, which prevents large stones from remaining in that side while the left section is more likely to have calculi.[31]
Amphibians
Most aquatic and semi-aquatic amphibians have a membranous skin which allows them to absorb water directly through it. Some semi-aquatic animals also have similarly permeable bladder membrane.[32] As a result, they tend to have high rates of urine production to offset this high water intake, and have urine which is low in dissolved salts. The urinary bladder assists such animals to retain salts. Some aquatic amphibian such as Xenopus do not reabsorb water, to prevent excessive water influx.[33] For land-dwelling amphibians, dehydration results in reduced urine output.[34]:p. 184
The amphibian bladder is usually highly distensible and among some land-dwelling species of frogs and salamanders may account for between 20% and 50% of their total body weight.[34]:p. 184
Fish
The gills of most teleost fish help to eliminate ammonia from the body, and fish live surrounded by water, but most still have a distinct bladder for storing waste fluid. The urinary bladder of teleosts is permeable to water, though this is less true for freshwater dwelling species than saltwater species.[27]:p. 219 Most fish also have an organ called a swim-bladder which is unrelated to the urinary bladder except in its membranous nature. The loaches, pilchards, and herrings are among the few types of fish in which a urinary bladder is poorly developed. It is largest in those fish which lack an air bladder, and is situated in front of the oviducts and behind the rectum.[35]
Mammals
All mammals have a urinary bladder. This structure begins as an embryonic cloaca. In the vast majority, this eventually becomes differentiated into a dorsal part connected to the intestine and a ventral part which becomes associated with the urinogenital passage and urinary bladder. The only mammals in which this does not take place are the platypus and the spiny anteater both of which retain the cloaca into adulthood.[26]
The mammalian bladder is an organ that regularly stores a hyperosmotic concentration of urine. It therefore is relatively impermeable and has multiple epithelial layers. The urinary bladder of the cetaceans (whales and dolphins) is proportionally smaller than that of land-dwelling mammals.[36]
Birds
In nearly all bird species, there is no urinary bladder per se.[37] Although all birds have kidneys, the ureters open directly into a cloaca which serves as a reservoir for urine, fecal matter, and eggs.[38]
Crustaceans
Unlike the urinary bladder of vertebrates, the urinary bladder of crustaceans both stores and modifies urine.[39] The bladder consists of two sets of lateral and central lobes. The central lobes sit near the digestive organs and the lateral lobes extend along the front and sides of the crustacean's body cavity.[39] The tissue of the bladder is thin epithelium.[39]
Additional images
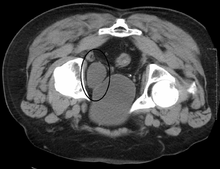
 Urinary bladder (black butterfly-like shape) and hyperplastic prostate (BPH) visualized by medical ultrasound
Urinary bladder (black butterfly-like shape) and hyperplastic prostate (BPH) visualized by medical ultrasound
See also
- Alpha blocker
- Cystitis glandularis
- UPK1B
- Ureterocele
References
- Boron, Walter F.; Boulpaep, Emile L. (2016). Medical Physiology. 3: Elsevier Health Sciences. p. 738. ISBN 9781455733286. Retrieved 1 June 2016.CS1 maint: location (link)
- Walker-Smith, John; Murch, Simon (1999). Cardozo, Linda (ed.). Diseases of the Small Intestine in Childhood (4 ed.). CRC Press. p. 16. ISBN 9781901865059. Retrieved 1 June 2016.
- Netter, Frank H. (2014). Atlas of Human Anatomy Including Student Consult Interactive Ancillaries and Guides (6th ed.). Philadelphia, Penn.: W B Saunders Co. pp. 346–8. ISBN 978-14557-0418-7.
- "SEER Training:Urinary Bladder". training.seer.cancer.gov.
- Viana R, Batourina E, Huang H, Dressler GR, Kobayashi A, Behringer RR, Shapiro E, Hensle T, Lambert S, Mendelsohn C (October 2007). "The development of the bladder trigone, the center of the anti-reflux mechanism". Development. 134 (20): 3763–9. doi:10.1242/dev.011270. PMID 17881488.
- Page 12 in: Uday Patel (2010). Imaging and Urodynamics of the Lower Urinary Tract. Springer Science & Business Media. ISBN 9781848828360.
- Fry, CH; Vahabi, B (October 2016). "The Role of the Mucosa in Normal and Abnormal Bladder Function". Basic & Clinical Pharmacology & Toxicology. 119 Suppl 3: 57–62. doi:10.1111/bcpt.12626. PMC 5555362. PMID 27228303.
- Stromberga, Z; Chess-Williams, R; Moro, C (7 March 2019). "Histamine modulation of urinary bladder urothelium, lamina propria and detrusor contractile activity via H1 and H2 receptors". Scientific Reports. 9 (1): 3899. Bibcode:2019NatSR...9.3899S. doi:10.1038/s41598-019-40384-1. PMC 6405771. PMID 30846750.
- Merrill L, Gonzalez EJ, Girard BM, Vizzard MA (April 2016). "Receptors, channels, and signalling in the urothelial sensory system in the bladder". Nat Rev Urol. 13 (4): 193–204. doi:10.1038/nrurol.2016.13. PMC 5257280. PMID 26926246.
- Janssen, DA (January 2013). "The distribution and function of chondroitin sulfate and other sulfated glycosaminoglycans in the human bladder and their contribution to the protective bladder barrier". The Journal of Urology. 189 (1): 336–42. doi:10.1016/j.juro.2012.09.022. PMID 23174248.
- Giglio, D; Tobin, G (2009). "Muscarinic receptor subtypes in the lower urinary tract". Pharmacology. 83 (5): 259–69. doi:10.1159/000209255. PMID 19295256.
- Uchiyama, T; Chess-Williams, R (December 2004). "Muscarinic receptor subtypes of the bladder and gastrointestinal tract". Journal of Smooth Muscle Research = Nihon Heikatsukin Gakkai Kikanshi. 40 (6): 237–47. doi:10.1540/jsmr.40.237. PMID 15725706.
- Andersson KE, Arner A (July 2004). "Urinary bladder contraction and relaxation: physiology and pathophysiology". Physiol. Rev. 84 (3): 935–86. CiteSeerX 10.1.1.324.7009. doi:10.1152/physrev.00038.2003. PMID 15269341.
- Moro, Christian; Tajouri, Lotti; Chess-Williams, Russ (2013). "Adrenoceptor Function and Expression in Bladder Urothelium and Lamina Propria". Urology. 81 (1): 211.e1–211.e7. doi:10.1016/j.urology.2012.09.011. PMID 23200975.
- Chancellor, M. B.; Yoshimura, N. (2004). "Neurophysiology of Stress Urinary Incontinence". Rev. Urol. 6 Suppl 3: S19–28. PMC 1472861. PMID 16985861.
- Moro, Christian; Uchiyama, Jumpei; Chess-Williams, Russ (2011). "Urothelial/Lamina Propria Spontaneous Activity and the Role of M3 Muscarinic Receptors in Mediating Rate Responses to Stretch and Carbachol". Urology. 78 (6): 1442.e9–1442.e15. doi:10.1016/j.urology.2011.08.039. PMID 22001099.
- Gray's 2008, p. 1249.
- Moore, Keith; Anne Agur (2007). Essential Clinical Anatomy, Third Edition. Lippincott Williams & Wilkins. pp. 227–228. ISBN 978-0-7817-6274-8.
- "Urinary Incontinence – Causes". NHS. Retrieved 21 August 2013.
- Moore, Keith L.; Dalley, Arthur F (2006). Clinically Oriented Anatomy (5th ed.). Lippincott Williams & Wilkins.
- Marieb, Mallatt. "23". Human Anatomy (5th ed.). Pearson International. p. 700.
- Purves, Dale (2011). Neuroscience (5. ed.). Sunderland, Mass.: Sinauer. p. 471. ISBN 978-0-87893-695-3.
- "Overactive Bladder". Cornell Medical College. Retrieved 21 August 2013.
- Negoro, Hiromitsu (2012). "Involvement of urinary bladder Connexin43 and the circadian clock in coordination of diurnal micturition rhythm". Nature Communications. 3: 809. Bibcode:2012NatCo...3..809N. doi:10.1038/ncomms1812. PMC 3541943. PMID 22549838.
- "Bladder Cancer". National Cancer Institute. 1 January 1980. Archived from the original on 17 July 2017.
- Herbert W. Rand (1950). The Chordates. Balkiston.
- P.J. Bentley (14 March 2013). Endocrines and Osmoregulation: A Comparative Account in Vertebrates. Springer Science & Business Media. ISBN 978-3-662-05014-9.
- Paré, Jean (11 January 2006). "Reptile Basics: Clinical Anatomy 101" (PDF). Proceedings of the North American Veterinary Conference. 20: 1657–1660.
- Davis, Jon R.; DeNardo, Dale F. (15 April 2007). "The urinary bladder as a physiological reservoir that moderates dehydration in a large desert lizard, the Gila monster Heloderma suspectum". Journal of Experimental Biology. 210 (8): 1472–1480. doi:10.1242/jeb.003061. ISSN 0022-0949. PMID 17401130.
- Wyneken, Jeanette; Witherington, Dawn (February 2015). "Urogenital System" (PDF). Anatomy of Sea Turtles. 1: 153–165.
- Divers, Stephen J.; Mader, Douglas R. (2005). Reptile Medicine and Surgery. Amsterdam: Elsevier Health Sciences. pp. 481, 597. ISBN 9781416064770.
- Urakabe, Shigeharu; Shirai, Dairoku; Yuasa, Shigekazu; Kimura, Genjiro; Orita, Yoshimasa; Abe, Hiroshi (1976). "Comparative study of the effects of different diuretics on the permeability properties of the toad bladder". Comparative Biochemistry and Physiology Part C: Comparative Pharmacology. 53 (2): 115–119. doi:10.1016/0306-4492(76)90063-0. PMID 5237.
- Shibata, Yuki; Katayama, Izumi; Nakakura, Takashi; Ogushi, Yuji; Okada, Reiko; Tanaka, Shigeyasu; Suzuki, Masakazu (2015). "Molecular and cellular characterization of urinary bladder-type aquaporin in Xenopus laevis". General and Comparative Endocrinology. 222: 11–19. doi:10.1016/j.ygcen.2014.09.001. PMID 25220852.
- Laurie J. Vitt; Janalee P. Caldwell (25 March 2013). Herpetology: An Introductory Biology of Amphibians and Reptiles. Academic. ISBN 978-0-12-386920-3.
- Owen, Richard (1843). Lectures on the comparative anatomy and physiology of the invertebrate animals. London: Longman, Brown, Green, and Longmans. pp. 283–284.
- John Hunter (26 March 2015). The Works of John Hunter, F.R.S. Cambridge University. p. 35. ISBN 978-1-108-07960-0.
- Cornell University. Laboratory of Ornithology (19 September 2016). Handbook of Bird Biology. John Wiley & Sons. ISBN 978-1-118-29105-4.
- Charles Knight (1854). The English Cyclopaedia: A New Dictionary of Universal Knowledge. Bradbury and Evans. p. 136.
- Nonmammalian animal models for biomedical research. Woodhead, Avril D. Boca Raton, Fla.: CRC Press. 1989. pp. 51–52. ISBN 0-8493-4763-7. OCLC 18816053.CS1 maint: others (link)
- Books
- editor-in-chief, Susan Standring; section editors, Neil R. Borley et al., ed. (2008). Gray's anatomy : the anatomical basis of clinical practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
- Britton, the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston; illustrated by Robert (2010). Davidson's principles and practice of medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
External links
| Wikimedia Commons has media related to Urinary bladder. |
- Histology at KUMC epithel-epith09 "Urinary Bladder"
- Anatomy photo: Urinary/mammal/bladder/bladder1 - Comparative Organology at University of California, Davis – "Mammal, bladder (LM, Medium)"
- Virtual Slidebox at Univ. Iowa Slide 445
- Anatomy photo:43:07-0100 at the SUNY Downstate Medical Center – "The Female Pelvis: The Urinary bladder"
- Anatomy photo:44:04-0103 at the SUNY Downstate Medical Center – "The Male Pelvis: The Urinary bladder"
- Bladder (ISSN 2327-2120) – An open-access journal on bladder biology and diseases.