Ian Donald
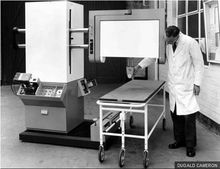
Ian Donald CBE FRFPSGlas FRCOG FRCP (27 December 1910 in Liskeard – 19 June 1987) was an English physician who was most notable for pioneering the diagnostic use of ultrasound in obstetrics, enabling the visual discovery of abnormalities in pregnancy.[2] Donald was Regius Professor of Obstetrics and Gynaecology at the University of Glasgow.[3] Donald's work was characterised by a series of remarkable collaborations between clinicians and engineers that strove to build instruments to enable the examination of the unborn[4] and that eventually enabled him to build the world's first obstetric ultrasound machine, the Diasonograph in 1963.[5] His other great achievement was to secure the construction of the Queen Mother's Maternity Hospital that was built next to the Royal Hospital for Children in Glasgow.[6]
Professor Sir Ian Donald | |
|---|---|
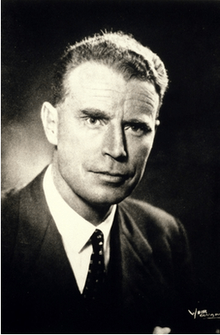 Portrait of Ian Donald | |
| Born | 27 December 1910 |
| Died | 19 June 1987 (aged 76) |
| Resting place | St Peters, Paglesham, Essex[1] |
| Nationality | English, British |
| Education | Fettes College, University of Cape Town, University of London, University of Glasgow |
| Known for | Developing obstetric ultrasound |
| Awards | CBE |
| Scientific career | |
| Fields | Obstetrics and Gynaecology |
| Institutions | St Thomas's Hospital Medical School, Royal Free Hospital, Western Infirmary |
| Influences | Arthur Joseph Wrigley |
Life
Donald was born to John Donald and Helen née Barron Wilson in 1910.[2] His father was a general practitioner who came from a paisley medical family.[7] His grandfather was also a GP. His mother was a concert pianist. Donald was the eldest of four children and his siblings were Margaret, Alison, and Malcolm.[8] His sister Alison Munro would later become a leading headmistress.[9]
Donald took his early education at the Warriston School preparatory school in Moffat and then his secondary education was completed at Fettes College, Edinburgh.[2] However, Donald never completed his education in Scotland as the family decided to move to South Africa due to his father's poor health.[10] Donald continued his secondary education at Diocesan College in Rondebosch where he studied the classics as well as music, philosophy, and languages.[8] In 1927 Donald's mother and two of his siblings contracted diphtheria and his mother died of a myocardial infarction.[8] Three months later Donald's father died. Maud Grant, the housekeeper, with a trust fund was left to care for the children.[8] Also in the same year, Donald achieved a Bachelor of Arts (BA) in arts and music at the University of Cape Town graduating with a First-class honours.[8] Achieving a BA is considered a traditional route to start medical school.[2]
In 1930 the family moved back to London and Donald matriculated at the University of London to study medicine at the St Thomas's Hospital Medical School.[8] In 1937 Donald achieved a Bachelor of Medicine, Bachelor of Surgery at St Thomas's becoming the third generation of doctors in Donald's family.[8]
At the end of his graduate education, Donald married Alix Mathilde de Chazal Richards [8] a farmer's daughter from the Orange Free State.[11] Donald retired on 1 October 1976. He was offered a consultancy at Nuclear Enterprises in Edinburgh, a position he held until 1981. After he fully retired, he moved to Paglesham, an area known for sailing and yachting, which he loved doing all his life. Donald passed away quietly on 19 June 1987. He was survived by his wife, his four daughters and thirteen grandchildren.[1] He was buried in the churchyard at St Peters Church, in Paglesham, Essex.[1]
Career
Donald started his postgraduate medical training at the end of the 1930s planning to specialise in Obstetrics with a position in Obstetrics and Gynaecology at St Thomas's and in 1939 he started his residency.[8]
Donald's medical career was interrupted by the arrival of World War II and on May 1942 he was drafted into the Royal Air Force as a medical officer to do his bit.[3] He was so successful in the role that he was mentioned in dispatches[3] for bravery after he pulled several airmen from an bomber that had crashed and had set on fire[2] while the bombs were still in the airframe.[12] In 1946 he was awarded a MBE for bravery.[3] During his time with the RAF, Donald became aware of a variety of techniques involving Radar and Sonar.[12]
In 1946 Donald completed his war service and returned to work at St Thomas's.[2] In 1949 he was appointed as a tutor in the department of obstetrics and gynaecology. By 1949 the National Health Service was in operation for three years and instead of the continual search for money for patient care, money now came from government taxes, so the hospital's role changed from a needs based approach to a focus on research. Specifically each doctor now had to conduct a research project as part of their remit.[8]
Negative-pressure respirator
In partnership with Maureen Young a specialist in perinatal physiology, Donald conducted a study of respiratory disorders in infants.[8] Donald's study included an examination of available medical respirators and he was not satisfied with the design and efficiency of operation of the current models.[8] Donald had an interest in mechanical and technological devices from childhood, so he decided to build a new respirator.[13] By 1952 Donald and Young had built a new medical negative-pressure respirator that they demonstrated at the meeting of the Physiological Society in a room at the Royal Free Hospital.[14]
Trip Spirometer
Later in 1952 Donald resigned his role at St Thomas's to take up a position as a reader at the Institute of Obstetrics and Gynecology at Royal Postgraduate Medical School located in Hammersmith Hospital.[15] At the medical school Donald continued his research into neonatal breathing disorders. Donald worked to improve the Servo patient-cycled respirator as the device that Donald and Young had built.[15] Later working with Josephine Lord, a registrar, Donald built a new piece of equipment called the Trip Spirometer later called the Spirometer whose purpose was to measure the respiratory efficiency of a neonate.[15] As well as being a diagnostic device, Donald used the device to make a quantitative determination of normal respiration with the goal of determining the physiology and pathology of neonatal pulmonary disease.[15]
Puffer
In 1953 Donald published a review of the best practice in neonatal resuscitation of the newborn.[16] While at the school, Donald worked on a third device, a positive-pressure respirator. Donald found that the negative-pressure device he had built with Young was not ideal as it was complicated to setup and difficult to use, requiring more than one person to operate.[15] Indeed, the Servo respirator seemed to be ideally suited to long term treatment of babies with breathing difficulties.[15] His rationale for creating a new device was based on the idea that a respirator was needed that could be used with a mask applied to a child in a cot or incubator.[15] He built a positive-pressure respirator that was later known in Hammersmith Hospital as the Puffer.[17] The Puffer device sent a stream of oxygen mixture to the baby's face and the device could be applied to an ailing baby in under a minute.[15] After treating several babies, colleagues requested that he convert the device to treat adults which he did with successful outcomes. This work came to the notice of the British Oxygen Company who wanted to commercially develop the positive-pressure respirator.[15]
In May 1954, Donald delivered the Blair-Bell Lecture at the Royal College of Obstetricians and Gynaecologists.[8] He spoke about Atelectasis Neonatorum and how his respirator could improve the management of the condition.[8] In the same period he met the biologist, electrical engineer and inventor John J. Wild in London. Wild had discussed the use of ultrasound with him. Wild had used pulse-echo ultrasound to visualize abnormal tissue in the human breast.[8] In September 1954 he was appointed by Hector Hetherington to Regius Professor of Midwifery.[1] Hetherington had to confirm the position with the Secretary of State for Scotland as it was a government appointment and Donald was proud of his commission that was signed personally by the Queen. Although Donald was impressed by Hetherington, Donald made it a condition of his employment that Hetherington had to promise to build a new maternity hospital in Glasgow, which he did.[18]
Obstetric Ultrasound
Whilst Professor of Regius Midwifery at Glasgow University, he first explored the use of obstetric ultrasound in the 1950s and through collaboration with John MacVicar, a registrar and obstetrician in the Department of Obstetrics and Gynaecology at the Western Infirmary and Tom Brown an industrial engineer who worked for Kelvin & Hughes Scientific Instrument Company, developed the first contact compound sector scanner[2] and an article in The Lancet called Investigation of Abdominal Masses by Pulsed Ultrasound.[19] The article contained the first ultrasound image of a fetus ever published.[20]
The development of Donald's interest in ultrasound started when one of his patients introduced her husband to Donald. The patient's husband was the director of the boiler fabrication company Babcock and Wilcox and he offered a tour of the plant to Donald who accepted.[8] Babcock and Wilcox in Renfrew was a large user of industrial ultrasound that was used to check for crack and flaws in welds. Donald's purpose in making the visit to Renfrew on 21 July 1955[21] was to determine if the industrial detecting equipment could be used to differentiate types of tissue.[13] Donald arrived at the plant with a number of fibroids and a large ovarian cyst taken from gynaecology patients. When Donald came across Bernard Donnelly, an employee in the research department of the boilermaker, Donald asked him to demonstrate the devices use by taking an ultrasound image of the bone of his thumb.[8] Donald experimented with the tissue samples along with a huge steak the company had provided for a control[13] and thereby confirmed the fact that ultrasound could be used to scan biological material. The results surprised him. He stated:
- All I wanted to know, quite simply, was whether these various masses differed in their ultrasonic echo characteristics. The results were beyond my wildest dreams and even with the primitive apparatus of those days clearly showed that a cyst produced echoes only at depth from the near and far walls, whereas a solid tumour progressively attenuated echoes at increasing depths of penetration.[21]
When he returned to hospital, Donald's goal was to find an ultrasound machine that he could continue to experiment with. He obtained a Kelvin Hughes Mark lIb supersonic flaw detector from William Valentine Mayneord at the Royal Cancer Hospital.[21] While Mayneord had been experimenting with the machine, trying to image the brain, he had been unsuccessful in his efforts, Donald hoped he could replicate and improve upon his previous success.[13] However, he found that when using the machine it could not produce echoes from less than 8 cm from the face of the transducer, making it almost useless for obstetric diagnostics.[13] Donald experimented with balloons and condoms filled with water, to use up the 8 cm gap with little success.[21] At the time Donald was being assisted by John Lenihan, a Professor of Clinical Physics, who was helping him to form image but the Mark IIb was insufficient for the task[13] and the images produced were of very poor quality.[2]
Experiments with A-mode scanner
It was in late 1956 when Tom Brown, a research engineer with Kelvin & Hughes, became involved. Brown although relatively young at twenty-three, had previously worked on an automatic flaw detector for testing of industrial products.[13] It was while working in the Western Infirmary installing a bulb in a theatre that Brown found out that Donald was using the flaw detector.[22] Brown immediately looked up Donald in the Infirmary directory, phoned him and arranged a meeting.[22] When they met, Brown noticed that the Mark lIb was not manufactured by Kelvin & Hughes but instead had been manufactured under contract. He also noticed that the machine had been converted from using a double probe, one to produce pulses and one to receive the pulses to a single probe.[22] Not wanting to insult Donald by explaining why the machine was not working correctly, Brown offered to try and source another machine from somewhere.[22] Brown phoned Alex Rankin, the man who collaborated with Brown on the automatic flaw detector for help and who would later be director of the department of Medical Ultrasonics at the company.[22] Rankin offered to gift the latest Mk IV Flaw Detector which was subsequently forwarded to Glasgow Central station from the Barkingside Labs location of Messrs Kelvin & Hughes, for delivery to Brown.[22] Rankin also spoke to the three directors at the company who decided to vote £500, a not inconsiderable sum on those days to support experiments.
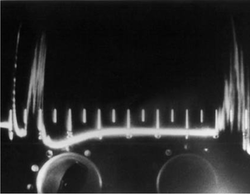
The new machine was considerably improved on the older machine with the difference being described as chalk and cheese by Donald. It was a double transducer probe machine.[22] At the same time Brown was able to scrounge a 'Cossor' oscilloscope camera which enabled images to be recorded on 35mm film.[22] For Donald the camera was particularly significant as it enabled a record to be kept, an archive of images to created and they could be printed in published works. Donald set about establishing a framework of use for the device, how it could be used, what the information on the screen meant.[13]
In 1956 the obstetrician John MacVicar was appointed as a registrar at the Western Infirmary and joined the team.[23] He would later become the Foundation Professor of Obstetrics and Gynaecology at the University of Leicester.[23]
By 1956 Donald and MacVicar had built up considerable experience of using the machine and had scanned 250 patients. For most of that period, Donald and MacVicar had tried to differentiate why particular scans produced a particular image.[24] They found that if there was fluid in the abdomen, e.g. an Ovarian cyst, there would be a clear gap in the image, until the ultrasound reached other side of the cyst.[24] They then tried to distinguish between different ascites, by matching images to particular type of ascites.[24] They also investigated the shape of image, in the presence of uterine fibroids.[24] It was about that time that Edward Johnson Wayne of the Department of Medicine at the Western Infirmary had heard of Donald's research and was keen on a demonstration of the technique.[24] Wayne would later be Regius Professor of the Practice of Medicine at Glasgow University. Wayne invited Donald to use his detector on a women who was dying from supposed stomach cancer. She was vomiting and losing weight rapidly and a barium x-ray had confirmed the diagnosis.[24] Donald had agreed with the diagnosis of ascites and applied the probe. What amused them was while they could use the old and well understood technique of Abdominal palpation to differentiate masses, Donald was using machinery to achieve the same result.[13] MacVicar not knowing the background of the case, commented, It looks like a cyst. Donald had to apologise to his colleagues as the diagnosis of a cyst was preposterous.[24] After a meeting to discuss the case, it was agreed that a Laparotomy should be performed and Donald would do it.[24] To his surprise, he discovered it was a pseudomucinous cyst that was filling the whole abdomen and was histologically benign.[24]
Donald and MacVicar was pleased with the results from the machine and continued to experiment in how it could be used for diagnosis but recognised that single dimension A-mode scanning was limited.[25] The images produced by the device were still of poor quality and many still felt there was no future in the new machine.[2] Donald learned of the work of Douglass Howry in the United States that an echo could only return to the probe and be recorded if the echo struck the reflecting surface at right angles, as the laws of optics required.[26] At this point, Tom Brown came on the scene and offered to help.[26] For Brown who was looking at the problem as an engineer in a clinical environment, he felt that the A-scope presentation was incompatible with the nature of the problem.[23] Brown thought the image displayed did not correspond closely enough to the condition to enable a correct diagnosis.[23] He believed that too much information was being returned in the image. The problem for him was that there was a myriad number of different echoes that were returned based on the sheer number of body structures. Even the patient breathing or moving on the table affected the image. Brown saw this as a problem and he planned to build a scanner that created an image that would be more useful for gynaecological diagnosis.[13] They agreed to build a machine that used a rotating compound scanning search technique, rather like radar scanning a sector to increase the amount of echo information available.[26]
Contact B-mode scanner
The solution proposed by Tom was to plot the position of the probe's echoes and create a two-dimensional picture.[23] This type of device was known as a B-mode device. Unlike the A-mode device which used a single or double transducer and the function of depth to obtain a reading, the B-mode devices uses a linear array of transducers that simultaneously scans a plane through the body that can be viewed as a two-dimensional image on screen.[27] Donald and Brown set out to create such a device.[27]
In 1956, to start the process of building the new scanner, Donald agreed to approach Kelvin and Hughes, now part of Smiths Industries and sent a letter to Ted Smith, a London-based salesman of the company.[13] At the same time, Brown also approached deputy chairman Bill Slater who sent Brown to see Bill Halliday, the company's chief research scientist for an opinion on building the machine.[28] After Brown delivered his spiel to Halliday it was several months before Brown received a reply in the form of a memo which stated that £500 had been allocated by Smiths for the development and that Brown was able to spend half a day per week working with Donald.[13]
The new B-mode scanner was also known by the name Bed-Table Scanner and was built out of an amalgamation of medical and industrial parts. Brown managed to scrounge an older Mark IV flaw detector in Glasgow along with a 6-inch electrostatically-deflected Cathode-ray tube taken from the company stores in Glasgow. From the companies Barkingside R&D department, Brown found an experimental weld-testing machine. Both these machines were cannibalised for parts. To measure the position of the transducer, Brown selected an 'X-Y' orthogonal measuring frame system. This was measured in place by a sine/cosine potentiometer that was used to calculate the position of the transducer from the angle of its rotations. This was an exceedingly expensive piece of electronic kit and cost more than their £500 budget. However, Brown managed to scrounge a damaged component and repaired it. The machine was built on top an old hospital bed and made extensive use of Meccano chains and sprockets.[13] By late 1957 the first contact B-mode scanner was constructed and in clinical use by that year.[13] The A-mode scanner was moved to the Royal Maternity Hospital at Rottenrow where James Willocks, who joined the team in 1958 and Tom Duggan, a physicist who was hired by Donald himself in 1959, began to investigate fetal development with the instrument.[13]
The initial test of the device was ultrasound of John MacVicar's abdomen.[29] In the same year, Donald started to experiment with taking images of pregnancy.[30] They also found that their original theories about ascites were correct.[30]
In a landmark paper in 7 June 1958, published by Donald, McVicar and Brown discussed the development of the A-mode scanner and decisions that led up to the B-mode scanner.[31] Donald and McVicar also described the first successful diagnosis using obstetric ultrasound with the B-mode machine. This occurred when a women patient was diagnosed with terminal cancer of the stomach using traditional clinical methods, palpation and by X-ray.[13] Donald diagnosed the women with an Ovarian cyst and when the women was sent for a Laparotomy, a large cyst was discovered and removed, vindicating Donald's diagnosis.[32] The paper highlighted the importance of the instant feedback that was available from the operating room to improve the quality of the image.[33] In the paper Donald referenced the work of ultrasound pioneers, Douglass Howry in Denver, United States and Yoshimitsu Kikuchi in Japan in the early 1950s, alongside the work of John J. Wild and John M Reid.[31] Also described in the paper was a description of testing of ultrasound on the brains of kittens to determine if there was any obvious changes in tissue structure. There was none.[13] The team's enthusiasm in the success of the B-mode and the publication of the paper resulted in a change in attitudes in the medical community and more confirmed that medical diagnosis could be made.[13]
Automatic scanner
In the period between 1958 and 1959 Donald became increasingly worried about scanning tissue deliberately to ensure he received sufficient detail, from fear of missing them.[34] Donald along with MacVicar had been trying unsuccessfully to image hydatidiform moles, which involved increasing the amplification of the signal, which resulted in an increase in what Donald called electronic grass.[13] He stated:
- With high gain settings we were confronted with the danger of being deceived by 'electronic grass'. This danger now seemed so great that we decided to eliminate at least this error from over amplification and observer error by having an automatic scanner which would operate at a completely standardised speed[13][35]
In 1958, Brown and the engineers at Hughes started work on the new automatic scanner.[13] The automatic scanner was built to standardize the compound scanning process and to remove, as far as possible, operator bias from the results.[36]
The probe was mounted in a steel ball that was connected to a column suspended from a gantry. In motion, it rocked to and fro. When it was 30° from the perpendicular to the skin, sensed by what Brown described as rather indelicate looking projections on either side of the ball, the motion was reversed and, simultaneously, the gantry supporting the column itself moved about 15mm, and the process was repeated. The scans could be done in the longitudinal plane, i.e. up or down the abdomen lengthways, rather than only across the width.[13] The machine had to be capable of scanning all the different sizes and shapes of the female form. In addition, the scanner had to not only cope with the convex shape of a women's abdomen, but also with women who were perhaps ill or had some other form of pathology or were pregnant or very rotund.[13] The way Brown designed this motion of maintaining contact with the body's surface was the use of another motor which would reposition the probe either up or down as required. This coupled with a pressure sensitive switch enabled the probe to stay in constant contact with the skin. Thus the machine had two motors, one for the vertical and one for the horizontal. However, the climbing of steep curves of heavier women presented its own problem. An elaborate control circuit was created that could switch between the two motors. The final part was the introduction of a joystick which enabled the initial position to be set on the body for the scan.[13]
This was the only automatic scanner built, in part due to funding problems and in part due to the complex nature of the machine, with continual tweaking needed to keep the valve electronics working.[13] In December 1959, Donald meet with William Slater at the Kelvin Hughes factory and the Slater expressed a desire to pull out of the development of the new automatic scanner due to the increasing and what they saw as out of control costs.[34] The original £500 allocated to the project has stretched into thousands of pounds and they could no longer afford it.[13] The running costs for the project were being met by the Scottish Endowments Hospital Trust but did not provide funding capital expenditure.[34] Donald consulted with Hector Hetherington, who immediately produced £750 pounds as a temporary measure while other funds were sought.[34] Donald then approached the Scottish Hospital Endowments Research Trust and the Department of Health for Scotland. Slater and Donald attended a lunch party with the trust who provided a grant of £4000 pounds.[34] The Trust asked to seek help at the National Research Development Corporation in London who provided them an immediate grant of £4000[34] that was later supplemented with additional funding up to a level of £10000 over several years.[13] The financial security was to last until 1965.[13]
For much of this period, Donald used his position as Regius Professor and his personal charisma and presence to sell the machine, or more accurately the potential of the ultrasound machine. The very idea of ultrasound and its benefits had to be disseminated to the medical community.[13] In 1959, a Swedish obstetrician Bertil Sundén of Lund University, Sweden visited Glasgow on a quest to find a subject for his MD thesis.[37] Glasgow University had established links with Lund University since the time of John Martin Munro Kerr.[37] Lars Leksell of Lund has been experimenting with Ultrasound since the 1950s and had been using a Kelvin and Hughes supersonic detector to experiment with. Leksell's work had been well known to obstetrics and gynaecology professor Alf Sjövall, who was friends with Donald and more importantly, knew his work. It was Sjövall who decided to send Sundén to Glasgow.[37] The outcome of the visit was that Sundén wanted to reproduce Donald's work from scratch. Despite the fact that the automatic scanner was almost completed, Sundén wanted an exact copy of the machine which Donald had used to produce his first publications, i.e. bed table scanner.[37] The result was an order for a new ultrasound machine costing £2500. This was the first direct-contact scanning machine built anywhere in the world and was a hybrid between the manually operated bed-table machine and the automatic scanner.[37] This was a new prototype and became the basis for the Diasonograph that became the first commercially produced machine[37] in 1965.
Donald at around this time embarked on a series of lectures in the US.[13] In 1960 Donald, MacVicar, and Brown demonstrated their scanner at a medical exhibition in Olympia, London, England.[8]
During this period Donald and his team scanned many hundreds of patients who were both pregnant and non-pregnant.[38] Donald found that fetal echoes were visible for an early stage and this led to the distinction between a case of threatened abortion with bleeding and a case with a hydatidiform mole also with bleeding.[38] The image showed a curious speckled picture, whereas the fetus produced strong echoes floating in space containing liquor.[38] Very quickly Donald was swamped for requests for differential diagnosis, so the work was eventually moved to the X-ray department.[38] At the same time Donald started to notice the very sharp echoes that were being produced at the sides of a babies head and this lead to the use of a hand-held probe and the A-mode scanner to detect the presentation of the fetus.[38] Donald's ward sister at Rottenrow, Marjory Marr rapidly made use of the technique to test doubtful cases in her antenatal ward, [38] and was able to tell Donald in advance during his Friday morning obstetric rounds where the fetus lay.[13] This led Donald to think about measuring the distance between the echoes as an index of the head or more specifically measuring the Biparietal diameter.[38] Experiments proved the idea as being feasible. The medical physicist Tom Duggan who was working with Donald, created a ranging unit in which the distance between echoes could be calculated in centimetres and millimetres.[38] James Willocks, a physician who worked with Donald in the same department at Rottenrow, undertook many hundreds of experiments using the new technique resulting in errors of less than 2% over 75% of cases.[38] The use of serial measurements of the fetal head was the first study to use ultrasound to measure fetal growth anywhere in the world.[39] Donald presented the results of the experiments at a meeting of the Royal Society of Medicine on 12 January 1962.[39]
By 1970, Donald was able to image fetal development during pregnancy using the Diasonograph, which led to new criteria to diagnose pregnancy failure, that resulted in his techniques being widely adopted as standard clinical practice in the 1970s.[8]
Queen Mother's Maternity Hospital
The idea of a new maternity hospital had been on Donald's mind when he was interviewed for his position as professor when he was asked what plans he had, should he be appointed.[40] He was in charge of a maternity unit at the Glasgow Royal Maternity and Women's Hospital, that was colloquially known as Rottenrow, that was already very old and unfit for purpose.[40]
Donald's first objective was to obtain the money to build the hospital. He harried the Scottish Office relentlessly until he received funding but it was insufficient to build the whole hospital.[40] A sum of £800,000 was needed.[41] Donald then turned to Glasgow University to request the final block of funding and it was through the help of Hetherington that this was secured.[40] The power that Glasgow University held in the planning process was illustrated when the Western Regional Hospital Board decided to build the hospital in the grounds of the old Robroyston hospital in the north-east of Glasgow. In a planning meeting when it was announced, Hetherington quietly stood up and stated: You must excuse me, gentleman, for you must know that if the proposal goes ahead the university can have no further interest in the project. Good afternoon.[40] This shocked the planning board who realised the vast sum of money that was being taken away with the university principal, so they reversed their position and agreed to build the hospital in Yorkhill, next to the Royal Hospital for Children.[40] In early 1958, Donald appointed the architect JL Gleave and together they produced a new design for a 112 bed maternity hospital that provided many new innovations.[40]
Traditionally maternity hospitals had consisted of two wards, antenatal and postnatal.[40] Antenatal wards were for undelivered patients, postnatal for patients who were recovering from delivery.[40] Wards were communal with privacy guaranteed by curtains. Generally deliveries would take place in the labour ward and only complicated deliveries or Caesarean sections were taken to the operating theatre.[40] Donald's plan was for a hospital with a central block with four wings. The central block had separate nursing, medical and anaesthetist staff and a separate delivery room for each women and two operating rooms for complicated cases.[40] The east wing had a separate room for each women and was reserved for complicated cases. The other wings were shared among senior consultants with their own junior staff in small four and six bed wards. Antenatal and postnatal women were mixed.[40] At the end of the hospital was the university department and tower block for residents and nursing staff.[40]
Construction began in June 1960 and Donald by some contrivance managed to appoint his ward sister in Rottenrow, Miss Marjory Marr to be the Master of Works who would report the progress of works to Donald each day.[40] The name of the new hospital was chosen by Donald who was a great admirer of Queen Elizabeth, The Queen Mother.[13] The hospital was the first of its kind to have a separate ultrasound examination room.[13]
In 1961 Donald wrote a detailed article for the Scottish Medical Journal for a series on hospital planning, in which he described the acute need for new maternity beds in Glasgow, the design of the new hospital, why the Yorkhill site was chosen and why he believed that the increasing and rapid pace of medical research would make the new hospital obsolete within 25 years.[42] The new hospital opened on 11 January 1964, with the first baby being born there on 12 January 1964. The hospital finally closed on 13 January 2010. Slightly longer than the 25 years envisioned by Donald.[43][44]
Health
For much of his life, Donald suffered from valvular heart disease,[20] that was a result of him and his sister Margaret becoming infected with Rheumatic fever when he was young.[45] His sister had died from a mitral valve replacement surgery that was still in the early stages of development.[45] In the Autumn of 1961, Donald collapsed in New York with atrial fibrillation. He decided to travel back to the Western Infirmary for treatment with a mitral valve replacement.[45] The condition meant that he suffered many debilitating illnesses, attacks and conditions like pressure sores, blot clots and hematomas that led to further cardiac deterioration, necessitating a new operation.[45]
Over a period of four years, Donald underwent three major heart operations at Hammersmith Hospital. For the third operation, a mitral valve replacement from a pig[45], with a homograft that had lasted since 1969 was replaced with a Starr Edwards artificial valve in 1976. Donald had published personal accounts of his second and third cardiac operations.[46]
Bibliography
- Donald, Ian (25 June 2016). "Sonar: What it Can and Cannot Do in Obstetrics". Scottish Medical Journal. 19 (5): 203–210. doi:10.1177/003693307401900501.
- Donald, Ian; Macvicar, J; Brown, T.G (June 1958). "Investigation of Abdominal Masses by Pulsed Ultrasound". The Lancet. 271 (7032): 1188–1195. doi:10.1016/S0140-6736(58)91905-6. PMID 13550965.
- Ainsworth, Steve (March 2005). "Good vibrations". The practising midwife. England. 8 (3): 50. ISSN 1461-3123. PMID 16250436.
- Nicolson, M; Fleming J; Spencer I (February 2005). "Hyaline membrane and neonatal radiology--Ian Donald's first venture into imaging research". Scottish Medical Journal. Scotland. 50 (1): 35–7. doi:10.1177/003693300505000115. ISSN 0036-9330. PMID 15792390.
- Donald, Ian; Brown T G (July 1995). "Localisation using physical devices, radioisotopes and radiographic methods. I.--Demonstration of tissue interfaces within the body by ultrasonic echo sounding. 1961". The British Journal of Radiology. ENGLAND. 68 (811): H129–36. ISSN 0007-1285. PMID 7640920.
- MacVicar, John; Donald, Ian (June 1963). "SONAR IN THE DIAGNOSIS OF EARLY PREGNANCY AND ITS COMPLICATIONS". BJOG: An International Journal of Obstetrics and Gynaecology. 70 (3): 387–395. doi:10.1111/j.1471-0528.1963.tb04920.x.
Awards and honours
References
- Adrian M. K. Thomas; Arpan K. Banerjee; Uwe Busch (23 November 2004). Classic Papers in Modern Diagnostic Radiology. Springer Science & Business Media. pp. 214–215. ISBN 978-3-540-21927-9. Retrieved 24 July 2019.
- "Ian Donald". Munks Roll – Lives of the Fellows. Royal College of Physicians: Royal College of Physicians. VIII: 136. 20 June 1987. Retrieved 5 July 2019.
- "Ian Donald". The University of Glasgow Story. University Roles: University of Glasgow 2018. Retrieved 5 July 2019.
- Tilli Tansey; Daphne Christie, eds. (2000), Looking at the Unborn: Historical aspects of obstetric ultrasound, Wellcome Witnesses to Contemporary Medicine, History of Modern Biomedicine Research Group, ISBN 978-1-84129-011-9, Wikidata Q29581634
- Hinds, Alice (18 June 2019). "How the first scans of pioneering doctors transformed treatment of babies before birth". DC Thomson Publishing. The Sunday Post. Retrieved 12 July 2019.
- "Papers of Ian Donald, obstetrician and developer of ultrasound, Glasgow, Scotland". JISC. NHS Greater Glasgow and Clyde Archives: Archive Hub GB 812 HB110. Retrieved 2 December 2019.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. p. 1. OCLC 57382713.
- Erjavic, Nicole (30 January 2018). "Ian Donald (1910–1987)". The Embryo Project Encyclopedia. The Embryo Project at Arizona State University. Retrieved 5 July 2019.
- "Donald, Ian". Oxford Dictionary of National Biography (online ed.). Oxford University Press. doi:10.1093/ref:odnb/40066. (Subscription or UK public library membership required.)
- Kurjak, A. (June 2000). "Ultrasound scanning – Prof. Ian Donald (1910–1987)". European Journal of Obstetrics & Gynecology and Reproductive Biology. 90 (2): 187–189. doi:10.1016/S0301-2115(00)00270-0.
- James Willocks; Wallace Barr (December 2004). Ian Donald: A Memoir. RCOG. p. 102. ISBN 978-1-904752-00-4. Retrieved 5 July 2019.
- James Willocks; Wallace Barr (December 2004). Ian Donald: A Memoir. RCOG. p. 16. ISBN 978-1-904752-00-4. Retrieved 12 July 2019.
- Nicholson, Deborah (2003). Secrets of success:the development of obstetric ultrasound in Scotland, 1963-1990 (PDF) (Phd Thesis). University of Glasgow. Retrieved 18 July 2019.
- Donald, Ian; Young, Maureen I. (19 January 1952). "PROCEEDINGS of the physiological society Department of physiology, Royal Free Hospital School of Medicine, Hunter Street and Institute of Ophthalmology, Judd Street, London, W.C.1. 19 January 1952". The Journal of Physiology. 116 (4): 41P–52P. PMC 1392055. PMID 14946717.
- Malcolm Nicolson; John E. E. Fleming (2013). Imaging and Imagining the Fetus: The Development of Obstetric Ultrasound. JHU Press. pp. 73–76. ISBN 978-1-4214-0793-7. Retrieved 25 July 2019.
- Donald, Ian (1953). "Resuscitation of the newborn" (PDF). Postgraduate Medical Journal. 29 (331): 247–253. doi:10.1136/pgmj.29.331.247. PMC 2500395. PMID 13055546.
- Donald, Ian (May 1954). "Augmented Respiration". The Lancet. 263 (6818): 895–899. doi:10.1016/S0140-6736(54)91522-6. PMID 13153139.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. pp. 13–14. OCLC 57382713.
- Donald, Ian; Macvicar, J; Brown, T.G (June 1958). "Investigation of Abdominal Masses by Pulsed Ultrasound". The Lancet. 271 (7032): 1188–1195. doi:10.1016/S0140-6736(58)91905-6. PMID 13550965.
- Nicolson, Malcolm (2000). "Ian Donald – Diagnostician and Moralist". Royal College of Physicians of Edinburgh. Edinburgh. Retrieved 19 July 2019.
- Donald, I (March 1974). "Apologia: how and why medical sonar developed". Annals of the Royal College of Surgeons of England. 54 (3): 132–40. PMC 2388393. PMID 4593690.
- Brown, Tom (Unpublished article) Development of ultrasonic scanning techniques in Scotland 1956-1979, 1994
- "Looking at the Unborn: Historical Aspects of Obstetric Ultrasound" (PDF). The History of Modern Biomedicine Research Group. Wellcome Institute for the History of Medicine: Wellcome Trust. 10 March 1998. pp. 17–19. Retrieved 6 August 2019.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. pp. 70–73. OCLC 57382713.
- Donald, Ian (1974). "Apologia: how and why medical sonar developed". Annals of the Royal College of Surgeons of England. 54. PMC 2388393.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. p. 74. OCLC 57382713.
- Carovac A, Smajlovic F, Junuzovic D (September 2011). "Application of ultrasound in medicine". Acta Inform Med. 19 (3): 168–71. doi:10.5455/aim.2011.19.168-171. PMC 3564184. PMID 23408755.
- "Looking at the Unborn: Historical Aspects of Obstetric Ultrasound" (PDF). The History of Modern Biomedicine Research Group. Wellcome Institute for the History of Medicine: Wellcome Trust. 10 March 1998. p. 11,38. Retrieved 6 August 2019.
- "Looking at the Unborn: Historical Aspects of Obstetric Ultrasound" (PDF). The History of Modern Biomedicine Research Group. Wellcome Institute for the History of Medicine: Wellcome Trust. 10 March 1998. p. 47. Retrieved 6 August 2019.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. p. 75. OCLC 57382713.
- Donald, Ian; Macvicar, J; Brown, T.G (June 1958). "INVESTIGATION OF ABDOMINAL MASSES BY PULSED ULTRASOUND". The Lancet. 271 (7032): 1188–1195. doi:10.1016/S0140-6736(58)91905-6.
- Donald, Ian; Macvicar, J; Brown, T.G (June 1958). "Investigation Of Abdominal Masses By Pulsed Ultrasound". The Lancet. 271 (7032): 1188–1195. doi:10.1016/S0140-6736(58)91905-6.
- Dastur, Adi E; Tank, PD (December 2008). "Ian Donald : the pioneer of ultrasound in medicine" (PDF). J Obstet Gynecol India. 8 (6).
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. pp. 75–76. OCLC 57382713.
- Donald, Ian (March 1974). "Sonar—The story of an experiment". Ultrasound in Medicine & Biology. 1 (2): 113. doi:10.1016/0301-5629(74)90001-5.
- "Looking at the Unborn: Historical Aspects of Obstetric Ultrasound" (PDF). The History of Modern Biomedicine Research Group. Wellcome Institute for the History of Medicine: Wellcome Trust. 10 March 1998. p. 10. Retrieved 6 August 2019.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. p. 82. OCLC 57382713.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. pp. 77–78. OCLC 57382713.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. p. 85. OCLC 57382713.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. pp. 46–63. OCLC 57382713.
- Cameron, Alan (November 2009). "The Vision of Ian Donald – 45 years of The Queen Mother's Hospital". Scottish Medical Journal. 54 (4): 2–2. doi:10.1258/rsmsmj.54.4.2.
- Donald, Ian (1961). "The New Yorkhill Maternity Hospital". Scottish Medical Journal. 164. 6: 164–169.CS1 maint: location (link)
- "Queen Mother's maternity hospital closes doors". BBC News. BBC. 13 January 2010. Retrieved 2 December 2019.
- "Queen Mother's Closes Its Doors". NHS Greater Glasgow and Clyde. 11 January 2010. Retrieved 2 December 2019.
- Willocks, James; Barr, Wallace (2004). Ian Donald : a memoir. London: RCOG Press. pp. 122–134. OCLC 57382713.
- Donald, Ian (1 April 1976). "At the Receiving End: A Doctor's Personal Recollections of Second — Time Cardiac Valve Replacement". Scottish Medical Journal. 21 (2): 49–57. doi:10.1177/003693307602100205.