X-ray of hip dysplasia
Projectional radiography ("X-ray") is one of the two main modalities of medical imaging to diagnose hip dysplasia, the other one being medical ultrasonography.[1].[2] Ultrasound imaging yields better results defining the anatomy until the cartilage is ossified. When the infant is around 3 months old a clear roentgenographic image can be achieved. Unfortunately the time the joint gives a good x-ray image is also the point at which nonsurgical treatment methods cease to give good results.
In children
Image quality checking

Reliability of measurements increases if indicators of pelvic alignment are taken into account:
- Tönnis introduced a quotient of pelvic rotation by dividing the horizontal diameter of the obturator foramen of the right side and that of the left. In neutral rotation the ratio is 1 but is considered to be acceptable when it is between 0.56 and 1.8.[3]
- The symphysis os-ischium angle of Tönnis evaluates the pelvic position in the sagittal plane. Lines are drawn from the highest point of the ischium to the most prominent point of the symphysis, joining at the inside of the pelvis. The range of normal values is from 90 to 135° and is related to the infant’s age.[3]
Measurements in children
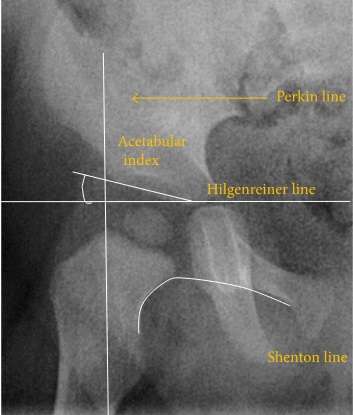
The most useful lines and angles that can be drawn in the pediatric pelvis assessing hip dysplasia are as follows:[3]
- (A) Hilgenreiner Line. It is considered a basal line joining the top aspect of the triradiate cartilages. This line is used to measure the acetabular angle and as a reference for Perkin line.
- (B) Perkin line is perpendicular to Hilgenreiner line, touching the lateral margin of the acetabulum. This leads to four quadrants and a normal femoral head has to be located in the inferomedial quadrant. We can measure the lateral displacement of the femoral head with regard to the Perkin line by dividing the width of the head that crosses the Perkin line by the diameter of the head. The value for patients under 3 years must be 0 and in older children this ranges from 0 to 22%.
- (C) Shenton line is a continuous arc drawn from the inner edge of the femoral neck to the superior margin of the obturator foramen. This should be smooth and undisrupted; otherwise it may indicate a fracture or hip dysplasia.
- (D) The acetabular index measures the acetabular roof slope. It is the most useful measure of acetabular dysplasia until 6 years of age. It is formed between Hilgenreiner line and the acetabular roof. In newborns, values of in males and in females are considered normal. Gradually this angle becomes smaller, with a mean value of in males and in females at 1 year of age.
- (E) The medial articular joint space is measured between the medial border of the femoral head or neck (when epiphysis is not ossified) and the acetabular platform. Normal values range between 5 and 12 mm. Differences greater than 1.5 mm between the two sides are considered abnormal.
In adults

In the adult hip there are important landmarks to be recognized on plain film radiographs (Figure 5):[3]
- (A) Iliopectineal or iliopubic line is formed by the arcuate line of the ilium and the superior border of the superior pubic ramus up to the pubic symphysis. It conforms to the inner margin of the pelvic ring and it is part of the anterior column of the acetabulum.
- (B) The ilioischial line of Köhler begins at the medial border of the iliac wing and extends along the medial border of the ischium to end at the ischial tuberosity. It is part of the posterior column of the acetabulum.
- (C) Acetabular Floor. In normal conditions the floor of the acetabular fossa is lateral to the ilioischial line by 2 mm in men and 1 mm in women. When the acetabular floor overlaps or overpasses the ilioischial line, the diagnosis of coxa profunda can be made. Nevertheless, coxa profunda had been found in 76% of asymptomatic hips, mainly in women. Therefore, this as an isolate criterion is not enough to make the diagnosis of pincer-type impingement. A more severe condition is protrusio acetabuli, diagnosed when the femoral head overlaps or overpasses the ilioischial line (Figure 5).
- (D) The teardrop represents a summation of shadows. Its medial aspect corresponds to the inner cortex of the pelvis and the lateral edge with the acetabular notch and the anteroinferior portion of the quadrilateral plate. It is not present at birth but gradually develops due to pressure of the femoral head.
In the adult hip, normal joint space ranges from 3 to 5 mm and must be uniform. Values under 2 mm are consistent with joint space narrowing. The most important measurements are detailed in Figure 6 and Table 1.[3]
| Measurement | Target | Normal value |
|---|---|---|
| Acetabular depth ratio | Deepness of acetabulum | >250 |
| Center-edge angle | Coverage of acetabulum | 20–40 |
| Tönnis angle | Slope of the sourcil | 0–10° |
| Sharp angle | Acetabular slope | <45° |
| Crossing ratio | Percentage of acetabular walls crossing | <20% |
| Alpha angle | Degree of bulging of the femoral head-neck junction |
|
| Femoral head-neck offset | Offset of the femoral head with regard to most prominent aspect of the femora neck | >10 mm |
| Offset percentage | Femoral head-neck offset related to femoral head diameter | >0.18 |
%2C_ilioischial_line_(yellow)%2C_tear_drop_(blue)%2C_acetabular_fossa_(brown)%2C_and_anterior_(white)_and_posterior_(green)_wall_of_the_acetabuli.jpg)
Figure 6:
 (a) Acetabular depth ratio.[3]
(a) Acetabular depth ratio.[3] (b) Center-edge angle of Wiberg.[3]
(b) Center-edge angle of Wiberg.[3]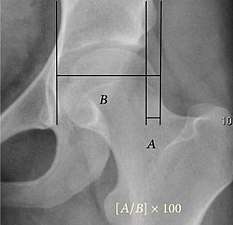 (c) Femoral extrusion index.[3]
(c) Femoral extrusion index.[3] (d) Tönnis angle.[3]
(d) Tönnis angle.[3] (e) Sharp angle.[3]
(e) Sharp angle.[3]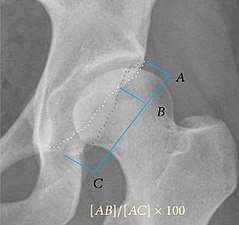 (f) Crossing ratio.[3]
(f) Crossing ratio.[3] (g) Alpha angle measured in 45° Dunn view.[3]
(g) Alpha angle measured in 45° Dunn view.[3]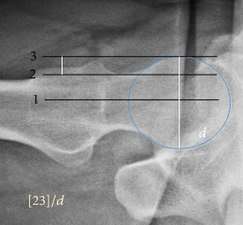 (h) Offset percentage measured in cross-lateral view.[3]
(h) Offset percentage measured in cross-lateral view.[3] (i) Cervical diaphyseal angle.[3]
(i) Cervical diaphyseal angle.[3]
Acetabular depth value under 250 characterizes the dysplastic hip.[3]
In normal conditions the acetabulum covers 75% of the femoral head. This coverage can be determined by three different measurements: lateral center-edge angle of Wiberg, anterior center-edge angle, and femoral extrusion index. Femoral extrusion index measures the percentage of the femoral head that lies outside of the acetabular roof. This percentage must be inferior to 25% in adults.[3]
Center-edge Wiberg’s angle measures the superior-lateral coverage of the femoral head. It is useful in children older than 5 years and in adulthood. For children between 5 and 10 years the minimum normal value is 15°, and in adults it is about 20°, although after 55 years this minimum increases to 24°. Values over 40° indicate overcoverage.[3]
Anterior center-edge Lequesne’s angle can be measured in a false profile view of the hip or in a sagittal CT scan. In this case the tangent line touches the anterior rim of the acetabulum. Values under 20° indicate undercoverage of the femoral head.[3]
The acetabular slope can also be measured by different methods. The Tönnis angle quantifies the slope of the sourcil (the sclerotic weight-bearing portion of the acetabulum). Values over 10° are considered a risk factor for instability, while values under 0° are considered a risk factor for pincer impingement.[3]
The Sharp angle is a global way to measure the acetabular slope. Angles over 45° are indicative of acetabular dysplasia.[3]
Normal acetabulum is oriented in anteversion. Its value ranges from 15 to 20° in the equatorial plane of the acetabulum and decreases gradually towards the acetabular roof, where normal values range from 0 to 5°. Retroversion of the upper part of the acetabulum has been related with pincer type impingement. In radiography the presence of a “crossover sign” is produced when the posterior wall of the acetabulum crosses the anterior wall before reaching the acetabular roof. It is a sign of acetabular retroversion and it has been linked with overcoverage and pincer impingement. Nevertheless, this sign has been described in 6% of the normal population. Therefore, more important than its presence is the percentage of crossing. This ratio is considered significant if it is over 20%.[3]
Other signs associated with acetabular retroversion are the sciatic spine and posterior wall signs. The first one is considered positive when the sciatic spine is projected medial to the iliopectineal line in an AP radiography of the spine, indicating that it is not just the acetabulum but the whole hemipelvis that is twisted into retroversion. The second sign is considered positive when the posterior wall edge is medial to the center of the femoral head, indicating deficiency of the posterior wall.[3]
In normal conditions there is a symmetric concave contour at the junction of the anterior and posterior profile of the femoral head and neck. Loss of this concavity or bone bulging may lead to cam type impingement. The degree of this deformity can be measured by the alpha angle. Although it can be measured in the cross-lateral view, the 45° Dunn view is considered more sensitive and the frog leg view more specific in determining pathologic values. Debate about which values are considered normal is still in progress. Based on the Copenhagen Osteoarthritis Study, a recent work defined three ranges of values for the α-angle: pathological (≥83° in men and ≥57° in women), borderline (69° to 82° in men, 51° to 56° in women), and normal (≤68° in men and ≤50° in women).[3]
The offset between the neck and femoral head can also be calculated in the lateral projection of the hip. A value of less than 10 mm is considered pathologic. The percentage is calculated by dividing the distance between the femoral head and the neck lines by the femoral head diameter. If this percentage is under 0.18 there is high probability of cam type impingement.[3]
The angle formed between the femoral neck and femoral diaphysis ranges from 120° to 140°. Coxa valga is diagnosed if the angle is higher and coxa vara if the angle is lower than this normal range.[3]
Although femoral version or torsion can be measured by radiographs, CT overcomes the inconsistencies demonstrated in the measurements made by biplane radiography.[3]
Crowe classification
In 1979 Dr. John F. Crowe et al. proposed a classification to define the degree of malformation and dislocation. Grouped from least severe Crowe I dysplasia to most severe Crowe IV.[4] This classification is very useful for studying treatment results.
Rather than using the Wiberg angle because it makes it difficult to quantify the degree of dislocation they used 3 key elements to determine the degree of subluxation: A reference line at the lower rim of the "teardrop", junction between the femoral head and neck of the respective joint and the height of the pelvis (vertical measurement). They studied anteroposterior pelvic x-rays and drew horizontal lines through the lower rim of a feature called "teardrop". The distance between this line and the middle lines of the junction between femur head and neck gave them a measure of the degree of femur head subluxation. They further established that a "normal" diameter of the femur head measures 20% of the height of the pelvis. If the middle line of the neck-head junction was more than 10% of the pelvis height above the reference line they considered the joint to be more than 50% dislocated.[4]
The following types resulted:[4]
| Class | Description | Dislocation |
| Crowe I | Femur and acetabulum show minimal abnormal development. | Less than 50% dislocation |
| Crowe II | The acetabulum shows abnormal development. | 50% to 75% dislocation |
| Crowe III | The acetabula is developed without a roof. A false acetabulum develops opposite the dislocated femur head position. The joint is fully dislocated. | 75% to 100% dislocation |
| Crowe IV | The acetabulum is insufficiently developed. Since the femur is positioned high up on the pelvis this class is also known as "high hip dislocation". | 100% dislocation |
References
- ↑ "Ultrasound Detection of DDH - International Hip Dysplasia Institute".
- ↑ "X-Ray Screening for Developmental Dysplasia of the Hip - International Hip Dysplasia Institute".
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 Initially largely copied from: Ruiz Santiago, Fernando; Santiago Chinchilla, Alicia; Ansari, Afshin; Guzmán Álvarez, Luis; Castellano García, Maria del Mar; Martínez Martínez, Alberto; Tercedor Sánchez, Juan (2016). "Imaging of Hip Pain: From Radiography to Cross-Sectional Imaging Techniques". Radiology Research and Practice. 2016: 1–15. doi:10.1155/2016/6369237. ISSN 2090-1941. Attribution 4.0 International (CC BY 4.0) license
- 1 2 3 Crowe JF, Mani VJ, Ranawat CS (1979). "Total hip replacement in congenital dislocation and dysplasia of the hip". J Bone Joint Surg Am. 61 (1): 15–23. doi:10.2106/00004623-197961010-00004. PMID 365863.