Patellar tendinitis
- Not to be confused with Runner's knee which often affects runners; or Sinding-Larsen and Johansson syndrome and Osgood-Schlatter disease which primarily affect young athletes.
| Patellar tendinitis | |
|---|---|
 | |
| Specialty |
Rheumatology |
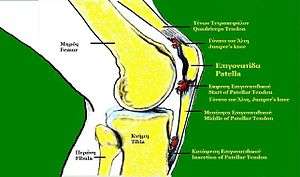
Patellar tendinitis (patellar tendinopathy, also known as jumper's knee), is a relatively common cause of pain in the inferior patellar region in athletes. It is common with frequent jumping and studies have shown it may be associated with stiff ankle movement and ankle sprains.[1][2]
Signs and symptoms
Jumper's knee (patellar tendinopathy, patellar tendinosis, patellar tendinitis) commonly occurs in athletes who are involved in jumping sports such as basketball and volleyball. Patients report anterior knee pain, often with an aching quality. The symptom onset is insidious. Rarely is a discrete injury described. Usually, involvement is infrapatellar at or near the infrapatellar pole, but it may also be suprapatellar.
Depending on the duration of symptoms, jumper's knee can be classified into 1 of 4 stages, as follows:
Stage 1 – Pain only after activity, without functional impairment
Stage 2 – Pain during and after activity, although the patient is still able to perform satisfactorily in his or her sport
Stage 3 – Prolonged pain during and after activity, with increasing difficulty in performing at a satisfactory level
Stage 4 – Complete tendon tear requiring surgical repair
It begins as inflammation in the patellar tendon where it attaches to the patella and may progress by tearing or degenerating the tendon. Patients present with an ache over the patella tendon. Most patients are between 10 and 16 years old. Magnetic resonance imaging can reveal edema (increased T2 signal intensity) in the proximal aspect of the patellar tendon.
Causes
It is an overuse injury from repetitive overloading of the extensor mechanism of the knee. The microtears exceed the body's healing mechanism unless the activity is stopped.
Among the risk factors for patellar tendonitis are low ankle dorsiflexion, weak gluteal muscles, and muscle tightness, particularly in the calves, quadriceps muscle, and hamstrings.[3]
The injury occurs to athletes in many sports.
Treatment
Early stages may be treated conservatively using the R.I.C.E methods.
- Rest
- Ice
- Compression
- Elevation
Exercises involving eccentric muscle contractions of the quadriceps on a decline board are strongly supported by extant literature.[4][5][6][7] A physical therapist may also recommend specific exercises and stretches to strengthen the muscles and tendons, eg. cycling or swimming. Use of a strap for jumper's knee and suspension inlays for shoes may also reduce the problems.
Should this fail, autologous blood injection, or platelet-rich plasma injection may be performed and is typically successful though not as successful as high volume saline injection (Crisp et al.). Uncommonly it may require surgery to remove myxoid degeneration in the tendon. This is reserved for patients with debilitating pain for 6–12 months despite conservative measures. Novel treatment modalities targeting the abnormal blood vessel growth which occurs in the condition are currently being investigated. New research shows that knee operations in most cases have no better effects than exercise programs, and that most knee operations thus can be avoided.
See also
References
- ↑ Marcus A (7 October 2011). "Stiff ankles tied to young athletes' painful knees". Reuters.
- ↑ Backman LJ, Danielson P (December 2011). "Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study". The American Journal of Sports Medicine. 39 (12): 2626–33. doi:10.1177/0363546511420552. PMID 21917610.
- ↑ Koban M (2013). Beating Patellar Tendonitis. pp. 20–25. ISBN 978-1491049730.
- ↑ Cannell LJ, Taunton JE, Clement DB, Smith C, Khan KM (February 2001). "A randomised clinical trial of the efficacy of drop squats or leg extension/leg curl exercises to treat clinically diagnosed jumper's knee in athletes: pilot study". British Journal of Sports Medicine. 35 (1): 60–4. doi:10.1136/bjsm.35.1.60. PMID 11157465.
- ↑ Purdam CR, Jonsson P, Alfredson H, Lorentzon R, Cook JL, Khan KM (August 2004). "A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy". British Journal of Sports Medicine. 38 (4): 395–7. doi:10.1136/bjsm.2003.000053. PMC 1724885. PMID 15273169.
- ↑ Kongsgaard M, Aagaard P, Roikjaer S, Olsen D, Jensen M, Langberg H, Magnusson SP (August 2006). "Decline eccentric squats increases patellar tendon loading compared to standard eccentric squats". Clinical Biomechanics. 21 (7): 748–54. doi:10.1016/j.clinbiomech.2006.03.004. PMID 16675081.
- ↑ Visnes H, Bahr R (April 2007). "The evolution of eccentric training as treatment for patellar tendinopathy (jumper's knee): a critical review of exercise programmes". British Journal of Sports Medicine. 41 (4): 217–23. doi:10.1136/bjsm.2006.032417. PMC 2658948. PMID 17261559.
Further reading
- Helms, Clyde (2009). Musculoskeletal MRI. ISBN 978-1-4160-5534-1. OCLC 909784879.
- Khan KM, Bonar F, Desmond PM, Cook JL, Young DA, Visentini PJ, Fehrmann MW, Kiss ZS, O'Brien PA, Harcourt PR, Dowling RJ, O'Sullivan RM, Crichton KJ, Tress BM, Wark JD (September 1996). "Patellar tendinosis (jumper's knee): findings at histopathologic examination, US, and MR imaging. Victorian Institute of Sport Tendon Study Group". Radiology. 200 (3): 821–7. doi:10.1148/radiology.200.3.8756939. PMID 8756939.
- Kettunen JA, Kvist M, Alanen E, Kujala UM (2017). "Long-term prognosis for jumper's knee in male athletes. A prospective follow-up study". The American Journal of Sports Medicine. 30 (5): 689–92. doi:10.1177/03635465020300051001. PMID 12239003.
- Crisp T, Khan F, Padhiar N, Morrissey D, King J, Jalan R, Maffulli N, Frcr OC (2009). "High volume ultrasound guided injections at the interface between the patellar tendon and Hoffa's body are effective in chronic patellar tendinopathy: A pilot study". Disability and Rehabilitation. 30 (20–22): 1625–34. doi:10.1080/09638280701830936. PMID 18608403.
- Järvinen TL, Guyatt GH (July 2016). "Arthroscopic surgery for knee pain". BMJ. 354: i3934. doi:10.1136/bmj.i3934. PMID 27439983.
External links
| Classification | |
|---|---|
| External resources |