Parathyroidectomy
| Parathyroidectomy | |
|---|---|
 Parathyroidectomy for parathyroid adenoma | |
| ICD-9-CM | 06.8 |
| MeSH | D016105 |
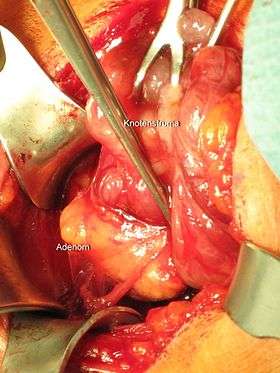
Parathyroidectomy is the surgical removal of one or more parathyroid glands. This procedure is used to remove primary tumors or hyperplasia of the glands, especially when they produce excessive parathyroid hormone (hyperparathyroidism). The location of the glands is generally behind the thyroid, but there is a lot of variation. Usually, the location of an enlarged gland has been confirmed via a sestamibi scan or on ultrasound.
Indications
The main indication for parathyroidectomy is primary hyperparathyroidism, where one or more of the parathyroid glands autonomously produce parathyroid hormone. Not all cases of primary hyperparathyroidism require surgery, but it is recommended if the condition causes significant symptoms or if it affects the kidneys (nephrocalcinosis) or bone health (osteoporosis), and also in people under 50 even if they do not have symptoms.[1] It is not always possible to anticipate if a parathyroid tumor is malignant (i.e. capable of invading other tissues or spreading elsewhere. Any suspicion of parathyroid carcinoma is therefore also an indication for surgery.[1]
Parathyroidectomy may also be required in secondary hyperparathyroidism. This situation arises mainly in people with severe chronic kidney disease in which the parathyroid glands are overactive to compensate for the low calcium and vitamin D levels often present in CKD. In many cases, the parathyroid hormone production improves when these abnormalities are treated with medication. A small proportion, however, have persistently raised hormone levels 6 months after treatment has started, thought to be autonomous production of hormone by the glands and loss of feedback mechanisms. In this situation surgical parathyroidectomy may be required, especially if calcium and phosphate levels remain elevated, there is calcium deposition on the blood vessels (calciphylaxis in severe cases) or there is worsening bone disease. In people on dialysis, parathyroidectomy can improve their survival. It does appear that the procedure may be underused.[2]
Procedure
The operation requires a general anesthetic (unconscious and pain free) or a local anesthetic (pain free). The surgeon makes an incision around an inch long in the neck just under the Adam's apple and locates the offending parathyroid glands. Preoperative testing using sestamibi scanning can help identify the location of glands. It can also be used to limit the extent of surgical exploration when used in conjunction with intraoperative PTH hormone monitoring.[3] The particular problem or disease process will determine how many of the parathyroid glands are removed. Some parathyroid tissue must be left in place to help prevent hypoparathyroidism.
Recovers after the operation tends to be swift. The PTH level is back to normal within 10–15 minutes, and can be confirmed by intraoperative rapid assessment during the operation. However, the remaining parathyroid glands may take hours to several weeks to return to their normal functioning levels (as they may have become dormant). Calcium supplements are therefore often required to prevent symptoms of hypocalcemia and to restore lost bone mass.
Complications
While mild hypocalcemia is common after parathyroidectomy, some people experience persistent prolonged low calcium levels as osteoclast cells in the bones remove large amounts of calcium from the bloodstream when the continuous presence of PTH is abruptly removed. This is called hungry bone syndrome. Prolonged calcium supplementation may be required. Hungry bone syndrome is particularly common in people who are on long-term regular dialysis.[2][4]
See also
References
- 1 2 Wilhelm, Scott M.; Wang, Tracy S.; Ruan, Daniel T.; Lee, James A.; Asa, Sylvia L.; Duh, Quan-Yang; Doherty, Gerard M.; Herrera, Miguel F.; Pasieka, Janice L.; Perrier, Nancy D.; Silverberg, Shonni J.; Solórzano, Carmen C.; Sturgeon, Cord; Tublin, Mitchell E.; Udelsman, Robert; Carty, Sally E. (1 October 2016). "The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism". JAMA Surgery. 151 (10): 959–968. doi:10.1001/jamasurg.2016.2310. PMID 27532368.
- 1 2 Lau, WL; Obi, Y; Kalantar-Zadeh, K (7 June 2018). "Parathyroidectomy in the Management of Secondary Hyperparathyroidism". Clinical Journal of the American Society of Nephrology. 13 (6): 952–961. doi:10.2215/CJN.10390917 (inactive 2018-08-30). PMC 5989682. PMID 29523679.
- ↑ Augustine, MM; Bravo, PE; Zeiger, MA (Mar–Apr 2011). "Surgical treatment of primary hyperparathyroidism". Endocrine Practice. 17 Suppl 1: 75–82. doi:10.4158/EP10359.RA. PMID 21324817.
- ↑ Jain, Nishank; Reilly, Robert F. (July 2017). "Hungry bone syndrome". Current Opinion in Nephrology and Hypertension. 26 (4): 250–255. doi:10.1097/MNH.0000000000000327. PMID 28375869.
External links
- Information from the American Association of Endocrine Surgeons
- Lee, J.A. (2006-10-16). "Parathyroidectomy". Medical Encyclopedia. Medline Plus. Retrieved 2007-11-02.