Obstetrical dilemma
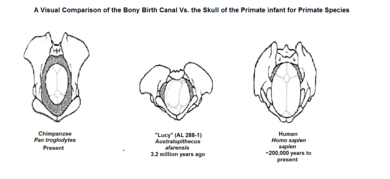
The obstetrical dilemma is a hypothesis to explain why humans often require assistance from other humans during childbirth to avoid complications, whereas most non-human primates give birth alone with relatively little difficulty. The obstetrical dilemma posits that this is due to the biological trade-off imposed by two opposing evolutionary pressures in the development of the human pelvis. As human ancestor species (hominids) developed bipedal locomotion (the ability to walk upright), decreasing the size of the bony birth canal, they also developed ever larger skulls, which required a wider obstetrical pelvic area to accommodate this trend in hominid infants.[1]
History
The term, obstetrical dilemma, was coined in 1960, by Sherwood Lerned Washburn (SL Washburn), a prominent early American physical anthropologist, in order to describe the evolutionary development of the human pelvis and its relation to childbirth and pregnancy in hominids and non-human primates.[2] In the intervening decades, the term has been used broadly among anthropologists, biologists, and other scientists to describe aspects of this hypothesis and related topics.
Evolution of human birth
Human pelvis
The obstetrical dilemma hypothesizes that when hominids began to develop bipedal locomotion, the conflict between these two opposing evolutionary pressures became greatly exacerbated. Because humans are currently the only recognized extant obligately bipedal primates, meaning our body shape requires to only use two legs, major evolutionary developments had to occur in order to alter to the shape of the female pelvis.[1] Human males evolved narrower hips optimized for locomotion, whereas female hips evolved to be a wider optimization because of childbirthing needs.[2][3][4] Human pelvises have no distinguishing skeletal markers for sex before puberty, meanwhile, with maturation, hormones and obstetrical demands alter the shape of the pelvis in females. Overall, through evolution of the species, a number of structures in the body have changed size, proportion, or location in order to accommodate bipedal locomotion and allow a person to stand upright and face forward. To help support the upper body, a number of structural changes were made to the pelvis. The ilial pelvic bone shifted forward and broadened, while the ischial pelvic bone shrank, narrowing the pelvic canal. These changes were occurring at the same time as humans were developing larger craniums.
Adaptations to ensure live birth
Early human ancestors, hominids, originally gave birth in a similar way that non-human primates do because early obligate quadrupedal individuals would have retained similar skeletal structure to great apes. Most non-human primates today have neonatal heads that are close in size to the mother’s birth canal, as evidenced by observing female primates who do not need assistance in birthing, often seeking seclusion away from others of their species.[5] In modern humans, parturition (childbirth) differs greatly from the rest of the primates because of both pelvic shape of the mother and neonatal shape of the infant. Further adaptations evolved to cope with bipedalism and larger craniums were also important such as neonatal rotation of the infant, shorter gestation length, assistance with birth, and a malleable neonatal head.
Neonatal rotation
During delivery neonatal rotation occurs when the body gets rotated to align head and shoulders transversely when entering the small pelvis (internal rotation) and then longitudinally to exit the birth canal (external rotation). This is an important mechanism because growth in the size of the cranium as well as the width of the shoulders makes it more difficult for the infant to fit through the pelvis.[1] This differs in non-human primates as there is no need for neonatal rotation in non-human primates because the birth canal is wide enough to accommodate the infant.[6]
Gestation length and altriciality
Gestation length in humans is shorter than most other primates. It is thought that this shorter gestation period is an adaptation to ensure the survival of mother and child because it leads to altriciality. The obstetrical dilemma hypothesis suggests that in order to successfully undergo childbirth, the infant must be born earlier and earlier, thereby making the child increasingly developmentally premature.[7] The concept of the infant being born underdeveloped is called altriciality. Humans are born with an underdeveloped brain; only 25% of their brains fully developed at birth as opposed to non-human primates where the infant is born with 45–50% brain development.[8]
Social assistance
Human infants are also almost always born with assistance from other humans because of the way that the pelvis is shaped. Since the pelvis and opening of birth canal face backwards, humans have difficulty giving birth themselves because they cannot guide the baby out of the canal. Non-human primates seek seclusion when giving birth because they do not need any help due to the pelvis and opening being more forward.[6] Human infants depend on their parents much more and for much longer than other primates.[3][7] Humans spend a lot of their time caring for their children as they develop whereas other species stand on their own from when they are born. The faster an infant develops, the higher the reproductive output of a female can be.[9] So in humans, the cost of slow development of their infants is that humans reproduce relatively slowly. This phenomenon is also known as cooperative breeding.
Malleable cranium
Humans are born with a very malleable fetal head which is not fully developed when the infant exits the womb.[1] This soft spot on the crown of the infant allows for the head to be compressed in order to better fit through the birth canal without obstructing it.[3] This allows for the head to develop more after birth and for the cranium to continue growing without affecting the birthing process.
Challenges to the obstetrical dilemma hypothesis
The obstetrical dilemma hypothesis has had several challenges to it, as more data is collected and analysized. Several different fields of study have taken an interest in understanding more about the human birth process and that of human ancestor species.
Early brain growth rates
Some studies have shown that higher brain growth rates happen earlier on in ontogeny than previously thought,[10] which challenges the idea that the explanation of the obstetrical dilemma is that humans are born with underdeveloped brains. This is because if brain growth rates were largest in early development, that is when the brain size would increase the most. Premature birth would not allow for a much larger head size if most of the growth had already happened. Also, it has been suggested that maternal pelvic dimensions are sensitive to some ecological factors.
Maternal heat stress
There has been a lot of evidence linking body mass to brain mass and determining maternal metabolism as a key factor in the growth of the fetus. Maternal constraints could be largely due to thermal stress or energy available. A larger brain mass in the neonate corresponds to more energy needed to sustain it. It takes much more energy for the mother if the brain fully develops in the womb. If maternal energy is the limiting factor then an infant can only grow as much as the mother can sustain. Also, because fetal size is positively correlated to maternal energy use, thermal stress is an issue because the larger the fetus the more the mother can suffer heat stress.[2]
Environmental effects
Additional studies suggest that other factors may further complicate the obstetrical dilemma hypothesis. One of these is dietary shifts, possibly due to the emergence of agriculture. This can be both due to change in diet as well as the increase in population density since agriculture was developed; more people leads to more disease.[2] Studies have also been done in twins to show that pelvic size may be due more to the environment in which they live than their genetics.[11] Another study disproves the thought that narrower hips are optimized for locomotion because it was found that a Late Stone Age population Southern Africa that survived largely on terrestrial mobility had women who had uncharacteristically small body size with large pelvic canals.[2]
Hormones
Moreover, the pelvis has the most favorable morphology for obstetrics between ages 25 and 30. Given that those are the ages of highest fertility, it may indicate that sex-biased autosomal gene expression, regulated by sex-specific hormones and sensitivity of hormone receptors, may obstruct the birth outside of that age range.
Energetics of gestation and growth hypothesis
The energetics of gestation and growth (EGG) hypothesis offers a direct challenge to the obstetrical dilemma hypothesis, equating the constraints on gestation and parturition to the energy restrictions of the mother. It has been shown that using both professional athletes and pregnant women, there is an upper limitation to the amount of energy a woman can produce before it cause deleterious effects: approximately 2.1x their basal metabolic rate. During pregnancy the growing brain mass and length in the neonate correspond to more energy needed to sustain it. This results in a competing balance between the fetus’s demand for energy and the maternal ability to meet that demand. At approximately 9 months gestation, the fetus’s energy needs surpasses the mother’s energy limitation, correlating with the average time of birth.[7] The newly born infant can then be sustained on breast milk, which is a more efficient, less energy demanding mechanism of nutrient transfer between mother and child.[12] Additionally, this hypothesis demonstrates that, contrary to the obstetrical dilemma, an increased pelvic size would not be deleterious to bipedalism. Studying the running mechanics of males and females, it was shown that an increased pelvic size related to neither an increased metabolic nor structural demand on a woman.[13]
Obstetrical dilemma revisited
The obstetrical dilemma hypothesis has also been challenged conceptually based on new studies. The authors argue that the obstetrical dilemma hypothesis assumes that human, and therefore hominid, childbirth has been a painful and dangerous experience through the species' evolution.[14] This assumption may be fundamentally false as many early analyses focused on maternal death data from primarily females of European-descent in Western Europe and the United States during the 19th and 20th century, a limited population in a time of great change. The study suggests the increase in maternal mortality during this time period was not due to evolutionary limitations as the creators of the obstetrical dilemma hypothesis thought, but due to the increased use of medical intervention, the medicalization of pregnancy and childbirth and restrictive socio-cultural practices of the Victorian era.[14] In a recent study a covariation between human pelvis shape, stature, and head size is reported. It is said that females with a large head possess a birth canal that can better accommodate large-headed neonates. Mothers with large heads usually give birth to neonates with large heads. Therefore, the detected pattern of covariation contributes to ease childbirth and has likely evolved in response to strong correlational selection.[15]
References
- 1 2 3 4 Wittman, A. B.; Wall, L. L. (2007). "The Evolutionary Origins of Obstructed Labor: Bipedalism, Encephalization, and the Human Obstetric Dilemma". Obstetrical & Gynecological Survey. 62 (11): 739–748. doi:10.1097/01.ogx.0000286584.04310.5c.
- 1 2 3 4 5 Wells, J. C. K.; Desilva, J. M.; Stock, J. T. (2012). "The obstetric dilemma: An ancient game of Russian roulette, or a variable dilemma sensitive to ecology?". American Journal of Physical Anthropology. 149: 40–71. doi:10.1002/ajpa.22160. PMID 23138755.
- 1 2 3 Rosenberg, K.; Trevathan, W. (2005). "Bipedalism and human birth: The obstetrical dilemma revisited". Evolutionary Anthropology. 4 (5): 161–168. doi:10.1002/evan.1360040506.
- ↑ "Why must childbirth be such hard labour? New evidence about why women give birth when they do has turned received opinion on its head by Alice Roberts, 2013-06-30".
- ↑ Isler, Karin; van Schaik, Caret (2012). "Allomaternal care, life history, and brain size evolution in mammals". Journal of Human Evolution. 63: 52–63. doi:10.1097/01.ogx.0000286584.04310.5c.
- 1 2 Rosenberg, Karen; Trevathan, Wenda (2003). "Birth, obstetrics and human evolution". BJOG. 109 (11): 1199–1206. doi:10.1046/j.1471-0528.2002.00010.x. PMID 12452455.
- 1 2 3 Dunsworth, H. M.; Warrener, A. G.; Deacon, T.; Ellison, P. T.; Pontzer, H. (2012). "Metabolic hypothesis for human altriciality". Proceedings of the National Academy of Sciences. 109 (38): 15212–15216. doi:10.1073/pnas.1205282109. PMC 3458333. PMID 22932870.
- ↑ Trevathan, Wenda (2011). Human Birth: An Evolutionary Perspective. Aldine Transaction. ISBN 1-4128-1502-9
- ↑ Garber, P.A.; Leigh, S.R. (1997). "Ontogenetic variation in small-bodied new world primates". Folia Primatologica. 68: 1–22. doi:10.1159/000157226. PMID 9170641.
- ↑ de Leon, Ponce; Marcia; et al. (2008). "Neanderthal brain size at birth proves insights into the evolution of human life history". PNAS. 105: 13764–13768. doi:10.1073/pnas.0803917105. PMC 2533682. PMID 18779579.
- ↑ Sharma, Krishan (2002). "Genetic basis of human female pelvic morphology: A twin study". American Journal of Physical Anthropology. 117: 327–333. doi:10.1002/ajpa.10055. PMID 11920368.
- ↑ Kane, Sunanda V.; Acquah, Letitia A. (2009). "Placenta transport of Immunoglobulins: A Clinical Review for Gastroenterologist Who Prescribe Therapeutic Monoclonal Antibodies to Women During Conception and Pregnancy". The American Journal of Gastroenterology. 104 (1): 228–33. doi:10.1038/ajg.2008.71. PMID 19098873.
- ↑ Warrener, Lisa; Lewton, Kristi L.; Pontzer, Herman; Lieberman, Daniel E. (March 1, 2015). "A Wider Pelvis Does Not Increase Locomotor Cost in Humans, with Implications for the Evolution of Childbirth". PLOS ONE. doi:10.1371/journal.pone.0118903. Retrieved July 19, 2016.
- 1 2 Stone, Pamela K. (January 25, 2016). "Biocultural Perspectives on Maternal Mortality and Obstetrical Death From the Past to the Present". American Journal of Physical Anthropology. 159 (S61): 150–171. doi:10.1002/ajpa.22906. PMID 26808103.
- ↑ Fischer, Barbara; Mitteroecker, Philipp (2015). "Covariation between human pelvis shape, stature, and head size alleviates the obstetric dilemma" (PDF). PNAS. 112 (18): 5655–5660. doi:10.1073/pnas.1420325112. PMC 4426453.