Menstrual cup

A menstrual cup is a feminine hygiene product that is inserted into the vagina during menstruation. Its purpose is to prevent menstrual fluid (blood from uterine lining) from leaking onto clothes. Menstrual cups are usually made of flexible medical grade silicone and shaped like a bell with a stem. The stem is used for insertion and removal. The bell-shaped cup seals against the vaginal wall just below the cervix. Every 4–12 hours (depending on the amount of flow), the cup is removed, emptied, rinsed, and reinserted. After each period, the cup should be boiled for at least 5 minutes and stored for use the next month.[1][2]
Unlike tampons and pads, cups collect menstrual fluid rather than absorbing it.[3][4][5] One cup is reusable for up to five years or more. This makes their long-term cost lower than that of disposable tampons or pads, though the initial cost is higher. Menstrual cups are also promoted as more practical and eco-friendly than pads and tampons. Given that the menstrual cup is reusable, its use greatly decreases the amount of waste generated from menstrual cycles, as there is no daily waste and the amount of discarded packaging decreases as well.
Most menstrual cup brands sell a smaller and a larger size. Menstrual cups are sold colorless and translucent, but several brands also offer colored cups, such as pink or purple.
The use of menstrual cups is considered a safe option relative to other forms of menstrual hygiene.[6][7]
Use
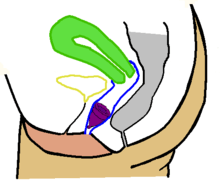
The menstrual cup is first folded or pinched and then inserted into the vagina. It will normally unfold automatically and create a light seal against the vaginal walls. In some cases, the user may need to twist the cup or flex the vaginal muscles to ensure the cup is fully open. The cup should sit around the cervix. If correctly inserted, the cup shouldn't leak or cause any discomfort. In comparison with a tampon, the menstrual cup should be placed lower in the vaginal canal.[8] The stem should be completely inside the vagina. There are various folding techniques for insertion; common folds include the c-fold, as well as the punch-down fold.[9]
If lubrication is necessary for insertion, it should be water-based, as silicone lubricant can be damaging to the silicone.
After 4–24 hours of use (depending on the amount of flow), the cup is removed by reaching up to its stem to find the base. Simply pulling on the stem is not recommended to remove the cup, as that can create suction. The base of the cup is pinched to release the seal, and the cup is removed.[8] After emptying, a menstrual cup should be rinsed or wiped and reinserted. It can be washed with a mild soap, and sterilized in boiling water for a few minutes at the end of the cycle. Alternatively, sterilizing solutions (usually developed for baby bottles and breast pump equipment) may be used to soak the cup. Specific cleaning instructions vary by brand.
Advantages
- When using a menstrual cup, the menstrual fluid is collected after it flows from the cervix and is held in liquid form. With tampons, liquid is absorbed and held in semi-coagulated form against the cervix.[10] This reduces odors.
- Menstrual cups collect menstrual fluid inside the vagina and generally do not leak (if emptied often enough and inserted properly). Some women have experienced leakage due to improper use or cup size. For example, a menstrual cup may leak if it is not inserted correctly and does not pop open completely and seal against the walls of the vagina.
- If a user needs to track the amount of menses she is producing (e.g., for medical reasons), a menstrual cup allows her to do so accurately. Some cups even have measuring marks on them.
Acceptability studies

A 2011 randomized controlled trial in Canada investigated whether silicone menstrual cups are a viable alternative to tampons and found that approximately 91% of women in the menstrual cup group said they would continue to use the cup and recommend it to others.[11] In a 1991 clinical study involving 51 women, 23 of the participants (45%) found rubber menstrual cups to be an acceptable way of managing menstrual flow.[12]
In a randomized controlled feasibility study in rural western Kenya, adolescent primary school girls were provided with menstrual cups or sanitary pads instead of traditional menstrual care items of cloth or tissue.[13] Girls provided with menstrual cups had a lower prevalence of sexually transmitted infections than control groups. Also, the prevalence of bacterial vaginosis was lower among cup users compared with sanitary pad users or those continuing other usual practice.[13] After six months, menstrual cup users were free from embarrassing leakage or odor, and could engage in class activities and sport without humiliation or being teased.[14]
Access to water and hygiene

- Cleaning a menstrual cup in a public toilet can pose problems as the handwashing sinks are usually, though not always, in a public space rather than in the toilet cubicle. Some manufacturers suggest wiping out the cup with a clean tissue and cleaning the cup at the next private opportunity. The user could also carry a small bottle of water to rinse the cup privately over the toilet. Another option is to use wet wipes. Since menstrual cups may only need to be emptied every 6–24 hours, many users do not have to empty them in public restrooms but rather in the comfort of their own home.
- A lack of clean water and soap for handwashing, needed before inserting the cup, presents a problem to women in developing countries.[14] Insertion requires thorough washing of the cup and hands to avoid introducing new bacteria into the vagina, which may heighten the risk of UTIs and other infections.[15] Disposable and reusable pads do not demand the same hand hygiene, though reusable pads also require access to water for washing out pads.
- Due to the fact that menstrual cups require boiling once a month, this can be a problem in developing countries if there is a lack of water, fire wood and good hygiene practices.[16] However, other options currently in use, such as rags that are washed, may be less hygienic.
- Removing a menstrual cup can be messy. Sometimes menstrual blood can spill during removal, although many women remove the device while hovering over a toilet to catch such spillage.
When using a urine-diverting dry toilet, menstrual blood can be emptied into the part that receives the feces. If any menstrual blood falls into the funnel for urine, it can be rinsed away with water.[17]
Safety
Menstrual cups are safe when used as directed and no health risks related to their use have been found.[7][18]
No medical research was conducted to ensure that menstrual cups were safe prior to introduction on the market.[19] Early research in 1962 evaluated 50 women using a bell-shaped cup. The researchers obtained vaginal smears, gram stains, and basic aerobic cultures of vaginal secretions. Vaginal speculum examination was performed, and pH was measured. No significant changes were noted. This report was the first containing extensive information on the safety and acceptability of a widely used menstrual cup that included both preclinical and clinical testing and over 10 years of post-marketing surveillance.[20]
One case report noted the development of endometriosis and adenomyosis in one menstrual cup user.[21] Additionally, one survey with a small sample size indicated a possible link. Therefore, two organizations have issued a combined statement that urged further research.[19] However, the U.S. Food and Drug Administration declined to remove menstrual cups from the market, saying that there was insufficient evidence of risk.[22]
A 2011 randomized controlled trial measured urovaginal infection in a comparison of menstrual cup and tampon use, and found no difference.[11]
No differences in the growth of Staphylococcus aureus, or health harms were identified among school girls provided with menstrual cups compared to those using sanitary pads, or continuing their usual practice in rural western Kenya.[13][23]
Toxic shock syndrome
Toxic shock syndrome (TSS) is a potentially fatal bacterial illness. Scientists have recognized an association between TSS and tampon use, although the exact connection remains unclear.[24] TSS caused by menstrual cup use appears to be very rare to virtually nonexistent.[11][25] The probable reason for this is that menstrual cups are not absorbent, do not irritate the vaginal mucosal tissue, and so do not change the vaginal flora in any measurable amount.[26] Conversely, vaginal dryness and abrasions may occur if the tampon used is more absorbent than needed for the menstrual flow, and normal liquid that should line the vaginal wall is also absorbed.[24] Research has shown that the cup has no impact on the vaginal flora, which means there is no effect on the presence of S. aureus, the bacterium that can cause TSS.[26] The risk of TSS associated with cervical caps used for contraception in the female barrier method is also very low.[27] Cervical caps and menstrual cups both use mostly medical grade silicone or latex.
However, recent research has shown that in vitro, One case report noted a confirmed case of toxic shock syndrome (TSS) associated with the use of the DivaCup menstrual cup.[28] The case was a woman who had a history of Hashimoto’s thyroiditis and chronic menorrhagia. This report is the first and only report to detail the association between a menstrual cup and menstrual TSS, making it very rare.
Types
Menstrual cups are generally bell-shaped, with a few exceptions. Most brands use medical grade silicone as the material for the menstrual cup, although latex and thermoplastic elastomer are also options. Menstrual cups made from silicone are generally designed to last for 1–5 years.
The majority of menstrual cup brands on the market are selling reusable cups, rather than disposable cups, which is therefore the focus of this article.
Sizing and selection
Most menstrual cup brands sell a smaller and a larger size. The smaller size is recommended for women under 30 who have not given birth vaginally. The larger size is recommended for women who are over 30, have given birth vaginally, or have a heavy flow. Cups with an even smaller size are recommended for teenagers, as well as women and girls who are more physically fit, as those with stronger pelvic floor muscles may find a larger cup uncomfortable. Length also needs to be considered: if a female's cervix sits particularly low, she may want to use a shorter cup. Capacity is important to women who have a heavier flow. The average menstrual cup holds around 20 ml. Some cups are designed to be larger and hold 37–42 ml. However, all cups currently available have a larger capacity than a regular tampon, which is 10–12 ml.[29]
A final consideration in selecting a menstrual cup is firmness or flexibility. Some companies offer a range of firmness levels in their cups. A firmer cup pops open more easily after insertion and may hold a more consistent seal against the vaginal wall (preventing leaks), but many women find softer cups more comfortable.[30]
Color
The silicone of which most brands of cups are produced is naturally colorless and translucent. Several brands offer colored cups as well as, or instead of the colorless ones. Translucent cups lose their initial appearance faster than colored – they tend to get yellowish stains with use. The shade of a colored cup may change over time, though stains are often not as obvious on colored cups. Stains on any color of cup can often be removed or at least lightened by soaking the cup in diluted hydrogen peroxide and/or leaving it out in the sun for a few hours.
Most cups produced do not have any other additives to them, except for the colored cups. The coloring used is reported to be safe and approved by the FDA for medical use and food coloring.
Disposable

A disposable cup (also called menstrual disc) is usually disc-shaped, like a diaphragm, with a flexible outer ring and a soft, collapsible center. It is designed to be disposed of after use. These tend to be made of a medical-grade polymer blend. It is placed at the base of the cervix in the vaginal fornix, and covers the cervix, like a diaphragm. Because of its placement, it can be worn during sexual intercourse, but it is not a contraceptive nor does it protect against sexually transmitted infections.[32]
Disposable cups are designed to fit most women, but may not be suitable for teenagers as the diameter of the rim may be uncomfortable. The disposable cup is pinched in half and inserted into the vaginal canal. Once inserted, a finger is used to push it back and down toward the cervix. The top rim of the disc rests behind the pubic bone. If correctly inserted, it should not be felt and should not leak.[31]
After about 12 hours of use (depending on flow volume), a disposable cup should be removed and disposed of. This is done by inserting a finger into the vagina, feeling for the top of the rim, hooking the finger beneath the rim and pulling straight out. Sitting down is recommended, to keep the disc parallel to the floor while removing. Removing a disc cleanly takes practice, and may be done while seated on the toilet to avoid spillage. During peak flow, most women use two disposable cups per day.[32]
Cost
Reusable menstrual products (including menstrual cups, but not disposable menstrual cups) are more economical than disposable products. Money will be saved using a menstrual cup, compared with other options such as tampons.[11] A woman in a developed country spends an average of US$60 per year on pads and tampons. If a woman menstruates for 40 years, the lifetime expense for pads and tampons is US$2,400. If the average silicon menstrual cup lasts between one and five years, eight would be needed in 40 years. If a menstrual cup costs US$30 (costs vary by manufacturer), the lifetime cost for a menstrual cup would be approximately US$240.[33]
The up-front cost of a menstrual cup may be expensive for women from low-income households, especially in developing countries. Buying pads or using rags monthly may seem more affordable than purchasing a menstrual cup, though the lifetime spend is higher.[15]
History
An early version of a bullet-shaped menstrual cup was patented in 1932, by the midwifery group of McGlasson and Perkins.[34] Leona Chalmers patented the first usable commercial cup in 1937.[35] Later menstrual cups were patented in 1935, 1937, and 1950.[36][37][38] The Tassaway brand of menstrual cups was introduced in the 1960s, but it was not a commercial success.[39] Early menstrual cups were made of rubber.[7]
In 1987, another latex rubber menstrual cup, The Keeper, was manufactured in the United States. This proved to be the first commercially viable menstrual cup and it is still available today. The first silicone menstrual cup was the UK-manufactured Mooncup in 2001. Most menstrual cups are now manufactured from medical grade silicone because of its durability and hypoallergenic properties, though there are also brands made of TPE (thermoplastic elastomer). Menstrual cups are becoming more popular worldwide, with many different brands, shapes and sizes on the market.[10] Most are reusable, though there is at least one brand of disposable menstrual cups currently manufactured.[10]
Some non-governmental organizations (NGOs) and companies have begun to propose menstrual cups to females in developing countries since about 2010, for example in Kenya and South Africa.[40] Menstrual cups are regarded as a low-cost and environmentally friendly alternative to sanitary cloth, expensive disposable pads or "nothing" – the reality for many females in developing countries.[16]
While numerous companies all over the world offer this product it was still not well known in around 2010. It may be difficult for companies to make profit from this product as one single menstrual cup can last a girl or woman five years or longer. Most women hear of menstrual cups through the internet or word of mouth, rather than through conventional advertizing on TV for example. As of 2018, menstrual cups are mentioned more and more often alongside tampons and pads in publications about menstrual hygiene management.
Society and culture
Developing countries
.jpg)
Menstrual cups can be useful as a means of menstrual hygiene management for women in developing countries, such as Kenya, Uganda and India, where access to affordable sanitary products may be limited.[14][41] A lack of affordable hygiene products means inadequate, unhygienic alternatives are often used, which can present a serious health risk.[42][43] Menstrual cups offer a long-term solution compared to some other feminine hygiene products because they do not need to be replaced monthly.
Cultural aspects
Feminine hygiene products that need to be inserted into the vagina can be unacceptable for cultural reasons. There are myths that they interfere with female reproductive organs and that females lose their virginity.[15] Use of a menstrual cup could stretch or break the hymen. Since some cultures value preservation of the hymen as evidence of virginity, this can discourage young women from using cups.
Environmental impact
Since they are reusable, menstrual cups help to reduce solid waste.[44] Some disposable sanitary napkins and plastic tampon applicators can take 25 years to break down in the ocean and can cause a significant environmental impact.[45] Biodegradable sanitary options are also available,[46] and these decompose in a short period of time, but they must be composted, and not disposed of in a landfill.
Each year, an estimated 20 billion pads and tampons are discarded in North America. They typically end up in landfills or are incinerated, which can have a great impact on the environment. Most of the pads and tampons are made of cotton and plastic. Plastic takes about 50 or more years and cotton starts degrading after 90 days if it's composted.[47]
Given that the menstrual cup is reusable, its use greatly decreases the amount of waste generated from menstrual cycles, as there is no daily waste and the amount of discarded packaging decreases as well. After their life span is over, the silicone cups are put in landfills or incinerated.
Menstrual cups may be emptied into a small hole in the soil or in compost piles, since menstrual fluid is a valuable fertilizer for plants and any pathogens of sexually transmitted diseases will quickly be destroyed by soil microbes.[48] The water used to rinse the cups can be disposed of in the same way. This reduces the amount of wastewater that needs to be treated.
In developing countries, solid waste management is often lacking. Here, menstrual cups have an advantage over disposable pads or tampons as they do not contribute to the solid waste issues in the communities or generate embarrassing refuse that others may see.
See also
| Wikimedia Commons has media related to Menstrual cup. |
References
- ↑ "What is a menstrual cup, review and use". louloucup. Retrieved 2018-07-06.
- ↑ "Care and cleaning". Divacup.com. 27 May 2018. Retrieved 27 May 2018.
- ↑ Elizabeth Gunther Stewart, Paula Spencer: The V Book: A Doctor's Guide to Complete Vulvovaginal Health, Bantam Books, 2002, Seiten 96 und 97, ISBN 0-553-38114-8.
- ↑ "Menstruationstasse für deine Tage". Archived from the original on November 19, 2016. Retrieved November 20, 2016.
- ↑ Leslie Garrett, Peter Greenberg: The Virtuous Consumer: Your Essential Shopping Guide for a Better, Kinder and Healthier World, New World Library, 2007, Seiten 17 bis 19, ISBN 1-930722-74-5.
- ↑ "What's a Menstrual Cup?". WebMD. Retrieved 2018-09-02.
- 1 2 3 Pruthi, Sandhya (January 30, 2008). "Menstrual cup: What is it?". Mayoclinic.com.
- 1 2 "Vagina Anatomy - Learn Your Parts". Lunette UK. Retrieved 2018-08-31.
- ↑ "How to Use a Menstrual Cup". wikiHow. March 2, 2015. Retrieved 2018-08-31.
- 1 2 3 "Alternative Menstrual Products". Center for Young Women's Health. Boston Children's Hospital. 28 March 2013. Retrieved 30 March 2013.
- 1 2 3 4 Howard C, Rose CL, Trouton K, Stamm H, Marentette D, Kirkpatrick N, Karalic S, Fernandez R, Paget J (June 2011). "FLOW (finding lasting options for women): Multicentre randomized controlled trial comparing tampons with menstrual cups". Canadian Family Physician. 57 (6): e208–15. PMC 3114692. PMID 21673197.
- ↑ Cheng M, Kung R, Hannah M, Wilansky D, Shime J (September 1995). "Menses cup evaluation study". Fertility and Sterility. 64 (3): 661–3. PMID 7641929.
- 1 2 3 Phillips-Howard, Penelope A.; Nyothach, Elizabeth; Ter Kuile, Feiko O.; Omoto, Jackton; Wang, Duolao; Zeh, Clement; Onyango, Clayton; Mason, Linda; Alexander, Kelly T. (2016). "Menstrual cups and sanitary pads to reduce school attrition, and sexually transmitted and reproductive tract infections: a cluster randomised controlled feasibility study in rural Western Kenya". BMJ open. 6 (11): e013229. doi:10.1136/bmjopen-2016-013229. ISSN 2044-6055. PMC 5168542. PMID 27881530.
- 1 2 3 Mason, Linda; Laserson, Kayla; Oruko, Kelvin; Nyothach, Elizabeth; Alexander, Kelly; Odhiambo, Frank; Eleveld, Alie; Isiye, Emily; Ngere, Isaac; Omoto, Jackton; Mohammed, Aisha; Vulule, John; Phillips-Howard, Penelope (2015). "Adolescent schoolgirls' experiences of menstrual cups and pads in rural western Kenya: a qualitative study". Waterlines. 34 (1): 15–30. doi:10.3362/1756-3488.2015.003. ISSN 0262-8104.
- 1 2 3 Crofts, T. (2012). Menstruation hygiene management for schoolgirls in low-income countries. Loughborough: Water, Engineering and Development Center (WEDC), Loughborough University.
- 1 2 APHRC (2010). Attitudes towards, and acceptability of, menstrual cups as a method for managing menstruation: Experiences of women and schoolgirls in Nairobi, Kenya - Policy Brief No. 21. The African Population and Health Research Center (APHRC), Nairobi, Kenya
- ↑ WECF (2006). Ecological sanitation and hygienic considerations for women - Fact Sheet. Women in Europe for a Common Future, Netherlands and Germany
- ↑ Stewart, Elizabeth B. (2002). The V Book: A Doctor's Guide to Complete Vulvovaginal Health. Bantam. p. 96. ISBN 0-553-38114-8.
- 1 2 Lione, Armand; Guidone, Heather C. "The ERC online questionnaire of women who used menstrual cups: summary statement of results and a call for additional research". assocpharmtox.org. Endometriosis Research Centre, Associated Pharmacologists & Toxicologists (APT).
- ↑ North, Barbara B.; Oldham, Michael J. (February 2011). "Preclinical, clinical, and over-the-counter postmarketing experience with a new vaginal cup: menstrual collection". Journal of Women's Health. Mary Ann Liebert, Inc. 20 (2): 303–311. doi:10.1089/jwh.2009.1929. PMC 3036176. PMID 21194348.
- ↑ Spechler S, Nieman LK, Premkumar A, Stratton P (2003). "The Keeper, a menstrual collection device, as a potential cause of endometriosis and adenomyosis". Gynecologic and Obstetric Investigation. 56 (1): 35–7. doi:10.1159/000072329. PMID 12867766.
- ↑ Lione, Armand. "Citizen Petition on Menstrual Cups & Endometriosis" (PDF). Retrieved 19 December 2010.
- ↑ Juma, Jane; Nyothach, Elizabeth; Laserson, Kayla F.; Oduor, Clifford; Arita, Lilian; Ouma, Caroline; Oruko, Kelvin; Omoto, Jackton; Mason, Linda (2017-05-04). "Examining the safety of menstrual cups among rural primary school girls in western Kenya: observational studies nested in a randomised controlled feasibility study". BMJ open. 7 (4): e015429. doi:10.1136/bmjopen-2016-015429. ISSN 2044-6055. PMC 5566618. PMID 28473520.
- 1 2 "Tampons and Asbestos, Dioxin, & Toxic Shock Syndrome". FDA U.S. Food and Drug Administration, U.S. Department of Health and Human Services. 13 May 2015. Retrieved 8 September 2015.
- ↑ MA Mitchell; S Bisch; S Arntfield; SM Hosseini-Moghaddam (August 2015). "A confirmed case of toxic shock syndrome associated with the use of a menstrual cup". Canadian Journal of Infectious Diseases & Medical Microbiology. 26 (4): 218–220.
- 1 2 North B. B., Oldham M. J. (2011). "Preclinical, Clinical, and Over-the-Counter Postmarketing Experience with a New Vaginal Cup: Menstrual Collection". Journal of Women's Health. 20 (2): 303–311. doi:10.1089/jwh.2009.1929. PMC 3036176. PMID 21194348.
- ↑ Faculty of Family Planning & Reproductive Health Care (2007). Female Barrier Methods. Archived 2015-11-26 at the Wayback Machine. London: p.3
- ↑ Mitchell MA, Bisch S, Arntfeld S, Hosseini-Moghaddam SM (2015). "A confirmed case of toxic shock syndrome associated with the use of a menstrual cup". Canadian Journal of Infectious Diseases & Medical Microbiology. 26: 218–20. doi:10.1155/2015/560959. PMC 4556184. PMID 26361491.
- ↑ "Assorted Size Charts". Menstrual Cup Support. 18 August 2008. Archived from the original on 17 July 2010. Retrieved 8 November 2009.
- ↑ Melissa L. "Menstrual Cup Info: Measurement Chart". Word Press Blog. Retrieved 21 May 2014.
- 1 2 How to use an Instead Softcup, Wikihow
- 1 2 "FAQs | learn more about FLEX & how to use it | The Flex Company". The Flex Company. Retrieved 2017-06-10.
- ↑ Caitlyn Shaye Weir, BSc Combined Honours, Environmental Science and Gender and Women Studies, Dalhousie University (2015) April 3rd, 2015
- ↑ Goddard, L.J. US Patent #1,891,761 (issued December 1932).
- ↑ North, Barbara B.; Oldham, Michael J. (Feb 2011). "Preclinical, Clinical, and Over-the-Counter Postmarketing Experience with a New Vaginal Cup: Menstrual Collection". J Womens Health (Larchmt). 20: 303–11. doi:10.1089/jwh.2009.1929. PMC 3036176. PMID 21194348.
- ↑ Hagedora, Arthur F. US Patent #1,996,242 (issued April 1935).
- ↑ Chalmers, Leona. US Patent #2,089,113 (issued August 1937).
- ↑ Chalmers, Ileona W. US Patent #2,534,900 (issued December 1950).
- ↑ Wysocki, Susan. "New Options in Menstrual Protection" Archived 2009-05-24 at the Wayback Machine.. Advance for Nurse Practitioners (November 1997).
- ↑ African Population and Health Research Center (APHRC). Use of Menstrual Cup by Adolescent Girls and Women: Potential Benefits and Key Challenges. In: Policy Brief No. 22. Nairobi: APHRC, 2010.
- ↑ Tellier M, Hyttel M, Gad M. Assessing acceptability and hygienic safety of menstrual cups as a menstrual management method for vulnerable young women in Uganda Red Cross Society’s Life Planning Skills Project, Kampala: WoMena, 2012.
- ↑ African Population and Health Research Center (APHRC). Experiences and Problems with Menstruation Among Poor Women and Schoolgirls in Nairobi. In: Policy Brief No. 20. Nairobi, Kenya: APHRC, 2010.
- ↑ Obiria M. Kenyan students could solve sanitary problem with banana-fibre pad. The Guardian. https://www.theguardian.com/global-development/2014/sep/26/kenyan-girls-sanitary-problem-banana-fibre-pad. 26 Sep 2014.
- ↑ Bharadwaj S, Patkar A. Menstrual hygiene and management in developing countries: Taking stock; Junction Social 2004.
- ↑ "The Environmental Impact of Everyday Things". The Chic Ecologist. Retrieved 22 August 2014.
- ↑ van Schagen, Sarah (8 November 2008). "A review of eco-minded feminine products". Grist. Retrieved 22 August 2014.
- ↑ Lili Li; Margaret Frey; Kristie J Browning (2010). "Biodegradability Study on Cotton and Polyester Fabrics" (PDF). Journal of Engineered Fibers and Fabrics. 5.
- ↑ CalRecycle. "Composting Reduces Growers' Concerns About Pathogens". Retrieved May 15, 2017.