Idiopathic CD4+ lymphocytopenia
| Idiopathic CD4+ lymphocytopenia | |
|---|---|
| Synonyms | IMMUNODEFICIENCY 13 |
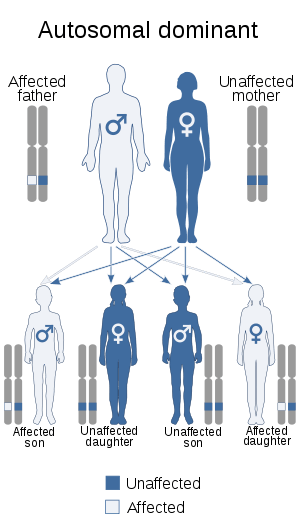 | |
| Idiopathic CD4+ lymphocytopenia is inherited via autosomal dominant manner[1] | |
| Classification and external resources | |
| Specialty | immunology |
Idiopathic CD4+ lymphocytopenia (ICL) is a rare medical syndrome in which the body has too few CD4+ T lymphocytes, which are a kind of white blood cell.[2] ICL is sometimes characterized as "HIV-negative AIDS" by AIDS denialists, though in fact its clinical presentation differs from that seen with HIV/AIDS.[3] People with ICL have a weakened immune system and are susceptible to opportunistic infections, although the rate of infections is lower than in people with AIDS.[4]
Cause
The cause of ICL, like all idiopathic conditions, is unknown. It does not appear to be caused by a transmissible agent, such as a virus.[5] It is widely believed that there is more than one cause.[6]
Pathophyisology
The loss of CD4+ T cells appears to be through apoptosis.[4][7] The accelerated deaths of the T cells is likely driven by crosslinking T cell receptors.[7]
Diagnosis
The mandatory criteria for diagnosis of idiopathic CD4+ lymphocytopenia include:[8]
- Low numbers of CD4+ cells, on two or more measurements over at least six weeks:
- CD4 cell count less than 300 cells per microliter, or
- Less than 20% of T lymphocytes are CD4+
- Lack of laboratory evidence of HIV infection
- Absence of any alternative explanation for the CD4 lymphocytopenia
A one-time finding of low CD4+ cells is usually associated with a recent infection and resolves on its own.[7] Alternative explanations for the low CD4 counts include conditions such as blood cancers (aleukemia), treatment with chemotherapy, immunosuppressive medications, or other medications that suppress or kill T cells, infections, and problems with blood production.[2][9]
All criteria must be fulfilled for a diagnosis of ICL. In addition, if these findings are present but combined with other significant findings, such as anemia or thrombocytopenia, then other diagnoses must be considered.
Prognosis
In contrast to the CD4+ cell depletion caused by HIV, in general, patients with idiopathic CD4 lymphocytopenia have a good prognosis.[6][10][11][12] The decline in CD4+ T-cells in patients with ICL is generally slower than that seen in HIV-infected patients.[3] The major risk to people with ICL is unexpected infections, including cryptococcus, atypical mycobacterial and Pneumocystis jiroveci pneumonia (PCP). The condition may also resolve on its own.[13]
ICL sometimes precedes and may be the first signal of several blood cancers. ICL patients have developed primary effusion lymphoma,[14][15] primary leptomeningeal lymphoma,[9] diffuse large cell lymphoma,[16] MALT lymphoma,[17] and Burkitt's lymphoma,[18] among others.
ICL may indirectly trigger autoimmune diseases. It has been associated with several cases of autoimmune disease Sjogren's syndrome.[4][19]
Because all of the reported autoimmune diseases and lymphomas involve B cells, one hypothesis proposes that ICL's narrow T cell repertoire predisposes the immune system to B cell disorders.[4]
Treatment
Fludarabine-based hematopoietic stem cell transplantation (HSCT) has shown to be a feasible treatment for ICL.[20]
Epidemiology
ICL is a very rare disease.[2] In 1993, a total of 47 confirmed cases were reported in a survey sponsored by the Centers for Disease Control.[21]
References
- ↑ "OMIM Entry - # 615518 - IMMUNODEFICIENCY 13; IMD13". omim.org. Retrieved 21 July 2017.
- 1 2 3 Walker UA, Warnatz K (July 2006). "Idiopathic CD4 lymphocytopenia". Curr Opin Rheumatol. 18 (4): 389–95. doi:10.1097/01.bor.0000231908.57913.2f. PMID 16763460.
- 1 2 Luo L, Li T (December 2008). "Idiopathic CD4 lymphocytopenia and opportunistic infection--an update". FEMS Immunol. Med. Microbiol. 54 (3): 283–9. doi:10.1111/j.1574-695X.2008.00490.x. PMID 19049641.
- 1 2 3 4 Wladis EJ, Kapila R, Chu DS (July 2005). "Idiopathic CD4+ lymphocytopenia and Sjogren syndrome" (PDF). Arch. Ophthalmol. 123 (7): 1012. doi:10.1001/archopht.123.7.1012-a. PMID 16009850. Archived from the original (PDF) on 2011-05-25.
- ↑ Online Medical Dictionary entry on T-lymphocytopenia Archived 2011-07-19 at the Wayback Machine.
- 1 2 Duncan RA, von Reyn CF, Alliegro GM, Toossi Z, Sugar AM, Levitz SM (February 1993). "Idiopathic CD4+ T-lymphocytopenia--four patients with opportunistic infections and no evidence of HIV infection". N. Engl. J. Med. 328 (6): 393–8. doi:10.1056/NEJM199302113280604. PMID 8093636.
- 1 2 3 Laurence J, Mitra D, Steiner M, Lynch DH, Siegal FP, Staiano-Coico L (February 1996). "Apoptotic depletion of CD4+ T cells in idiopathic CD4+ T lymphocytopenia". J. Clin. Invest. 97 (3): 672–80. doi:10.1172/JCI118464. PMC 507103. PMID 8609222.
- ↑ UpToDate article on "Techniques and interpretation of measurement of the CD4 cell count in HIV-infected patients", by John G. Bartlett. Accessed 30 Oct 2006.
- 1 2 Busse PJ, Cunningham-Rundles C (March 2002). "Primary leptomeningeal lymphoma in a patient with concomitant CD4+ lymphocytopenia". Ann. Allergy Asthma Immunol. 88 (3): 339–42. doi:10.1016/S1081-1206(10)62019-4. PMID 11926631.
- ↑ Laurence J, Siegal F, Schattner E, Gelman I, Morse S (1992). "Acquired immunodeficiency without evidence of infection with human immunodeficiency virus types 1 and 2". Lancet. 340 (8814): 273–4. doi:10.1016/0140-6736(92)92359-N. PMID 1353194.
- ↑ Ho D, Cao Y, Zhu T, Farthing C, Wang N, Gu G, Schooley R, Daar E (1993). "Idiopathic CD4+ T-lymphocytopenia--immunodeficiency without evidence of HIV infection". N Engl J Med. 328 (6): 380–5. doi:10.1056/NEJM199302113280602. PMID 8093634.
- ↑ Spira T, Jones B, Nicholson J, Lal R, Rowe T, Mawle A, Lauter C, Shulman J, Monson R (1993). "Idiopathic CD4+ T-lymphocytopenia--an analysis of five patients with unexplained opportunistic infections". N Engl J Med. 328 (6): 386–92. doi:10.1056/NEJM199302113280603. PMID 8093635.
- ↑ Zonios DI, Falloon J, Bennett JE, et al. (July 2008). "Idiopathic CD4+ lymphocytopenia: natural history and prognostic factors". Blood. 112 (2): 287–294. doi:10.1182/blood-2007-12-127878. PMC 2442741. PMID 18456875.
- ↑ Niino D, Tsukasaki K, Torii K, et al. (January 2008). "Human herpes virus 8-negative primary effusion lymphoma with BCL6 rearrangement in a patient with idiopathic CD4 positive T-lymphocytopenia". Haematologica. 93 (1): e21–3. doi:10.3324/haematol.12085. PMID 18166773.
- ↑ Richetta A, Amoruso GF, Ascoli V, et al. (2007). "PEL, Kaposi's sarcoma HHV8+ and idiopathic T-lymphocitopenia CD4+". Clin Ter. 158 (2): 151–5. PMID 17566517.
- ↑ Campbell JK, Prince HM, Juneja SK, Seymour JF, Slavin M (April 2001). "Diffuse large cell lymphoma and t(8;22) (q24;q11) in a patient with idiopathic CD4+ T-lymphopenia". Leuk. Lymphoma. 41 (3–4): 421–3. doi:10.3109/10428190109057998. PMID 11378556.
- ↑ Longo F, Hébuterne X, Michiels JF, Maniere A, Caroli-Bosc FX, Rampal P (January 1999). "[Multifocal MALT lymphoma and acute cytomegalovirus gastritis revealing CD4 lymphopenia without HIV infection]". Gastroenterol. Clin. Biol. (in French). 23 (1): 132–6. PMID 10219614.
- ↑ Shimano S, Murata N, Tsuchiya J (July 1997). "[Idiopathic CD4+ T-lymphocytopenia terminating in Burkitt's lymphoma]". Rinsho Ketsueki (in Japanese). 38 (7): 599–603. PMID 9267164.
- ↑ Mandl T, Bredberg A, Jacobsson LT, Manthorpe R, Henriksson G (April 2004). "CD4+ T-lymphocytopenia--a frequent finding in anti-SSA antibody seropositive patients with primary Sjögren's syndrome". J. Rheumatol. 31 (4): 726–8. PMID 15088298.
- ↑ Hamidieh, A. A.; Pourpak, Z.; Hamdi, A.; Nabavi, M.; Ghavamzadeh, A. (2013). "Successful fludarabine-based hematopoietic stem cell transplantation in a pediatric patient with idiopathic CD4+ lymphocytopenia". Pediatric Transplantation. 17 (4): E109–11. doi:10.1111/petr.12086. PMID 23581828.
- ↑ Smith D, Neal J, Holmberg S (1993). "Unexplained opportunistic infections and CD4+ T-lymphocytopenia without HIV infection. An investigation of cases in the United States. The Centers for Disease Control Idiopathic CD4+ T-lymphocytopenia Task Force". N Engl J Med. 328 (6): 373–9. doi:10.1056/NEJM199302113280601. PMID 8093633.
External links
| Classification | |
|---|---|
| External resources |