Epidural hematoma
| Epidural hematoma | |
|---|---|
| Synonyms | Extradural hematoma, epidural hemorrhage, epidural haematoma, epidural bleeding |
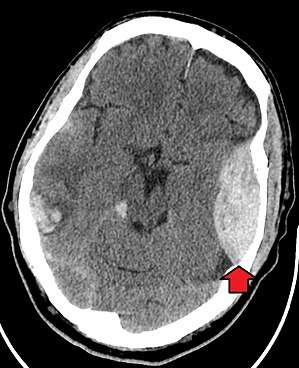 | |
| Epidural hematoma as seen on CT scan with overlying skull fracture. Note the biconvex shape hemorrhage. Also some brain contusion with bleeding on the opposite side of the brain. | |
| Specialty | Neurosurgery, emergency medicine |
| Symptoms | Headache, confusion, paralysis[1] |
| Usual onset | Rapid[2] |
| Causes | Head injury, bleeding disorder, blood vessel malformation[1] |
| Diagnostic method | Medical imaging (CT scan)[1] |
| Differential diagnosis | Subdural hematoma, subarachnoid hemorrhage, traumatic brain injury[1] |
| Treatment | Surgery (craniotomy, burr hole)[1] |
Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain (dura mater), and the skull.[3] Often there is loss of consciousness following a head injury, a brief regaining of consciousness, and then loss of consciousness again.[2] Other symptoms may include headache, confusion, vomiting, and an inability to move parts of the body.[1] Complications may include seizures.[1]
The cause is typically head injury that results in a break of the temporal bone and bleeding from the middle meningeal artery.[3] Occasionally it can occur as a result of a bleeding disorder or blood vessel malformation.[1] Diagnosis is typically by a CT scan or MRI.[1] When this condition occurs in the spine it is known as a spinal epidural hematoma.[3]
Treatment is generally by urgent surgery in the form of a craniotomy or burr hole.[1] Without treatment death typically results.[4] The condition occurs in one to four percent of head injuries.[1] Typically it occurs in young adults.[1] Males are more often affected than females.[1]
Signs and symptoms
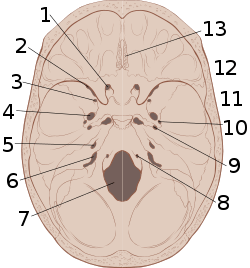
Epidural, subdural, and subarachnoid hemorrhages are extra-axial bleeds, occurring outside of the brain tissue, while intra-axial hemorrhages, including intraparenchymal and intraventricular hemorrhages, occur within it.
Epidural hematomas may present with a lucid period immediately following the trauma and a delay before symptoms become evident. After the epidural hematoma begins collecting, it starts to compress intracranial structures which may impinge on the CN III.[5] This can be seen in the physical exam as a fixed and dilated pupil on the side of the injury.[5] The eye will be positioned down and out, due to unopposed CN IV and CN VI innervation.
Other manifestations will include weakness of the extremities on the opposite side as the lesion (except in rare cases), due to compression of the crossed pyramid pathways, and a loss of visual field opposite to the side of the lesion, due to compression of the posterior cerebral artery on the side of the lesion.
The most feared event that takes place is tonsillar herniation which could result in respiratory arrest since the medullary structures are compromised. The trigeminal nerve (CN V) may be involved late in the process as the pons becomes compressed, but this is not a significant clinical presentation, since by that time the patient may already be dead.[6] In the case of epidural hematoma in the posterior cranial fossa, the herniation is tonsillar and causes the Cushing's triad: hypertension, bradycardia, and irregular respiration.
Epidural bleeding is rapid because it is usually from arteries, which are high pressure. Epidural bleeds from arteries can grow until they reach their peak size at six to eight hours post injury, spilling from 25 to 75 cubic centimeters of blood into the intracranial space.[7] As the hematoma expands, it strips the dura from the inside of the skull, causing an intense headache. Epidural bleeds can become large and raise intracranial pressure, causing the brain to shift, lose blood supply, or be crushed against the skull. Larger hematomas cause more damage. Epidural bleeds can quickly expand and compress the brainstem, causing unconsciousness, abnormal posturing, and abnormal pupil responses to light.[8]
Cause
The most common cause of intracranial epidural hematoma is traumatic, although spontaneous hemorrhage is known to occur. Hemorrhages commonly result from acceleration-deceleration trauma and transverse forces.[7][9] The majority of bleeds originate from meningeal arteries, particularly in the temporal region. 10% of epidural bleeds may be venous,[10] due to shearing injury from rotational forces. Epidural hematoma commonly results from a blow to the side of the head. The pterion region which overlies the middle meningeal artery is relatively weak and prone to injury.[10] Thus only 20 to 30% of epidural hematomas occur outside the region of the temporal bone.[11] The brain may be injured by prominences on the inside of the skull as it scrapes past them. Epidural hematoma is usually found on the same side of the brain that was impacted by the blow, but on very rare occasions it can be due to a contrecoup injury.[12]
Diagnosis
On images produced by CT scans and MRIs, epidural hematomas usually appear convex in shape because their expansion stops at the skull's sutures, where the dura mater is tightly attached to the skull. Thus they expand inward toward the brain rather than along the inside of the skull, as occurs in subdural hematoma. The lens-like shape of the hematoma causes the appearance of these bleeds to be "lentiform".
Epidural hematomas may occur in combination with subdural hematomas, or either may occur alone.[10] CT scans reveal subdural or epidural hematomas in 20% of unconscious patients.[13] In the hallmark of epidural hematoma, patients may regain consciousness and appear completely normal during what is called a lucid interval, only to descend suddenly and rapidly into unconsciousness later. The lucid interval, which depends on the extent of the injury, is a key to diagnosing epidural hemorrhage. If the patient is not treated with prompt surgical intervention, death is likely to follow.[14]
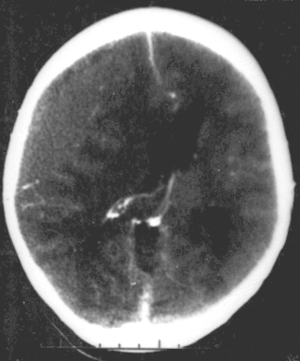 Nontraumatic epidural hematoma in a young woman. The grey area in the top left is organizing hematoma, causing midline shift and compression of the ventricle.
Nontraumatic epidural hematoma in a young woman. The grey area in the top left is organizing hematoma, causing midline shift and compression of the ventricle. Non-contrast CT Scan of a traumatic acute hematoma in the left fronto-temporal area
Non-contrast CT Scan of a traumatic acute hematoma in the left fronto-temporal area
Treatment
As with other types of intracranial hematomas, the blood may be removed surgically to remove the mass and reduce the pressure it puts on the brain.[9] The hematoma is evacuated through a burr hole or craniotomy. If transfer to a facility with neurosurgery is prolonged trephination may be performed in the emergency department.[15]
Prognosis
In TBI patients with epidural hematomas, prognosis is better if there was a lucid interval (a period of consciousness before coma returns) than if the patient was comatose from the time of injury.[16] Unlike most forms of TBI, people with epidural hematoma and a Glasgow Coma Score of 15 (the highest score, indicating the best prognosis) are expected to make a good outcome if they can receive surgery quickly.[16]
Notable cases
Michel de Montaigne, in his essay "That to Philosophise is to Learn to Die," written in the 1580s, gives the case of his brother, Captain Saint-Martin, aged 23 years. He was playing real, or court, tennis "when he was struck by a ball a little above the right ear. There being no sign of a wound or contusion, he did not sit down to rest, but five or six hours later he died of an apoplexy caused by this blow." [from the translation by E. J. Trechmann]
On November 18, 1982, 23 year old boxer Kim Duk-koo fought Ray Mancini in a US sanctioned fight. In the 14th round Mancini hit Kim with a hard right and bounced Kim off the ropes. Kim went down hitting his head on the canvas. Referee Richard Green stopped the fight and Mancini was declared the winner by TKO. Minutes after the fight was over Kim collapsed into a coma and was taken to the Desert Springs Hospital. Emergency brain surgery was performed but Kim died four days later.[17]
On February 20, 1998, 38-year-old Indian cricketer Raman Lamba was hit on the head by a cricket ball while fielding without a helmet. Although Lamba walked off the field and the injury did not appear to be serious at the time, he slipped into a coma on the day of the injury and then succumbed to internal hemorrhage three days later.[18]
On April 17, 2003, at age 72, Dr. Robert Atkins, creator of the Atkins diet, slipped on the ice while walking to work, hitting his head and causing bleeding around his brain. He lost consciousness on the way to the hospital, where he spent two weeks in intensive care. His death certificate states that the cause of death was "blunt impact injury of head with epidural hematoma".[19]
On March 18, 2009, actress Natasha Richardson died as a result of an epidural hematoma sustained two days earlier while skiing in Mont-Tremblant, Québec, Canada.[20] Like many patients, she had a lucid interval where she did not exhibit any symptoms until approximately an hour after her fall when she complained of a headache.[21] By the time she reached medical care, the hematoma had already caused significant damage.[22][23]
On May 26, 2010, actor Gary Coleman was admitted to Utah Valley Regional Medical Center in Provo, Utah, after falling and hitting his head and suffering an epidural hematoma at his home in Santaquin, Utah. He was announced to be in critical condition. By mid-afternoon on May 27, 2010, Coleman was unconscious and on life support. He died at 12:05 p.m. MDT (18:05 UTC) on May 28, 2010.
On September 5, 2012, Major League Baseball Pitcher Brandon McCarthy was hit by a line drive to the head from Erick Aybar. He was immediately rushed to the hospital where he underwent a 2-hour surgery to relieve pressure on his brain. Although he never lost consciousness and walked off the field, McCarthy suffered an epidural hemorrhage, brain contusion and skull fracture in the accident.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Ferri, Fred F. (2016). Ferri's Clinical Advisor 2017 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 441. ISBN 9780323448383.
- 1 2 Pooler, Charlotte (2009). Porth Pathophysiology: Concepts of Altered Health States. Lippincott Williams & Wilkins. p. 1256. ISBN 9781605477817.
- 1 2 3 Pryse-Phillips, William (6 May 2009). Companion to Clinical Neurology. Oxford University Press. p. 335. ISBN 9780199710041. Retrieved 8 October 2014.
Epidural hemorrhage (epidural hematoma, extradural hemorrhage, or hematoma) Bleeding outside the outermost layer of the dural mater, which is thus stripped away from the inner table of the skull or spinal canal.
- ↑ Rubin, Raphael; Strayer, David S.; Rubin, Emanuel; (M.D.), Jay M. McDonald (2008). Rubin's Pathology: Clinicopathologic Foundations of Medicine. Lippincott Williams & Wilkins. p. 1183. ISBN 9780781795166.
- 1 2 Epidural Hematoma in Emergency Medicine at Medscape. Author: Daniel D Price. Updated: Nov 3, 2010
- ↑ Wagner AL. 2006. "Subdural Hematoma." Emedicine.com. Retrieved on February 6, 2007.
- 1 2 University of Vermont College of Medicine. "Neuropathology: Trauma to the CNS." Retrieved on February 6, 2007.
- ↑ Singh J and Stock A. 2006. "Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
- 1 2 McCaffrey P. 2001. "The Neuroscience on the Web Series: CMSD 336 Neuropathologies of Language and Cognition." California State University, Chico. Retrieved on February 6, 2007.
- 1 2 3 Shepherd S. 2004. "Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
- ↑ Graham DI and Gennareli TA. Chapter 5, "Pathology of Brain Damage After Head Injury" Cooper P and Golfinos G. 2000. Head Injury, 4th Ed. Morgan Hill, New York.
- ↑ Mishra A, Mohanty S (2001). "Contre-coup extradural haematoma: A short report". Neurology India. 49 (94): 94–5. PMID 11303253. Retrieved 2008-01-24.
- ↑ Downie A. 2001. "Tutorial: CT in Head Trauma" Archived November 6, 2005, at the Wayback Machine.. Retrieved on February 6, 2007.
- ↑ Caroline NL. 1991. Emergency Medical Treatment. Little Brown & Company.
- ↑ Smith SW, Clark M, Nelson J, Heegaard W, Lufkin KC, Ruiz E (2010). "Emergency department skull trephination for epidural hematoma in patients who are awake but deteriorate rapidly". J Emerg Med. 39 (3): 377–83. doi:10.1016/j.jemermed.2009.04.062. PMID 19535215.
- 1 2 Zink BJ (2001). "Traumatic brain injury outcome: Concepts for emergency care". Ann Emerg Med. 37 (3): 318–32. doi:10.1067/mem.2001.113505. PMID 11223769.
- ↑ Kriegel, Mark (September 16, 2012), "A Step Back", The New York Times
- ↑ "Cricketer killed by ball". BBC. February 23, 1998. Retrieved January 3, 2010.
- ↑ "Copy of Robert Atkins' Death Certificate". The Smoking Gun. Retrieved 2008-10-14.
- ↑ "Family hold wake for Richardson". BBC News. March 21, 2009. Retrieved May 2, 2010.
- ↑ "Natasha Richardson dies aged 45". BBC News. March 19, 2009. Retrieved May 2, 2010.
- ↑ Autopsy: Natasha Richardson died from hitting head, Associated Press, March 19, 2009
- ↑ Brain injury victims can seem OK, symptoms delayed, Associated Press, March 19, 2009
External links
| Classification | |
|---|---|
| External resources |