Emergency tourniquet

Emergency tourniquets are cuff-like devices designed to stop severe traumatic bleeding before or during transport to a care facility. They are wrapped around the limb, proximal to the site of trauma, and tightened until all blood vessels underneath are occluded. The design and construction of emergency tourniquets allows quick application by first aid responders or the injured persons themselves.[1] Correct use of tourniquet devices have been shown to save lives under austere conditions with comparatively low risk of injury. In field trials, prompt application of emergency tourniquets before the patient goes into shock are associated with higher survival rates than any other scenario where tourniquets were used later or not at all.[2][3]
Tourniquet design

Existing guidelines call for the use of improvised "rope-and-stick" tourniquets as a last resort to stop severe bleeding. However, purpose-made tourniquet devices that are well designed can provide greatly increased safety and efficacy.[2][4] Variability in performance has been shown to exist between various designs and application methods.[5][6]
Mechanical advantage
Mechanisms that confer sufficient mechanical advantage are essential for applying adequate pressure to stop bleeding, particularly on the lower extremities. Pressures that occlude venous but not arterial flow can exacerbate hemorrhage and cause damage to healthy tissue.[1]
Mechanical characteristics of emergency tourniquet devices
| Tourniquet | Strap Width (cm) [1] | Mechanism [1] | Note [1] |
|---|---|---|---|
| Combat Application Tourniquet (CAT) | 3.8 | Windlass | Stick and strap inside outer sleeve |
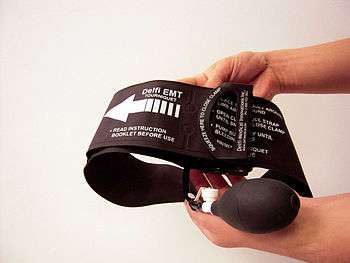
| Emergency & Military Tourniquet (EMT) | 9.1 | Pneumatic | Hand pump and inflatable bladder |
| K2 Tactical Tourniquet (K2) | 3.8 | Clamp | Modified wood clamp |
| Smart Tactical Application Tourniquet (S.T.A.T.) | 2.5 | Ratchet | Strap with ratcheting mechanism |
| Last Resort Tourniquet (LRT) | 5.1 | Ratchet | Strap with ratcheting mechanism |
| London Bridge Tourniquet (LBT) | 2.4 | Ratchet | Strap with ratcheting mechanism |
| Mechanical Advantage Tourniquet (MAT) | 3.8 | Block and tackle | Pulleys on outer frame |
| One-Handed Tourniquet (OHT) | 2.8 | Elastic | Parallel bungee cords and clamp |
| Self-Applied Tourniquet System (SATS) | 3.8 | Cam | Cantilever system |
| Special Operations Forces Tactical Tourniquet (SOFTT) | 3.7 | Windlass | Stick and strap |
Results from laboratory and field testing suggest that windlass and pneumatic mechanisms are effective where other systems fail due to excessive pain, slipping, inadequate force, or mechanical failure.[1][2]
Pressure gradients
Pressure underneath a tourniquet cuff is not evenly distributed, with the highest pressures localized around the cuff centerline and decreasing to zero near the cuff edges.[7] A high rate of change of pressure across the cuff width, or a high cuff pressure gradient, is a leading cause of nerve and muscle injury from tourniquet use.[7] Tourniquets with wider straps or cuffs, especially those with pneumatic actuation in contrast to mechanical force, distribute pressure more evenly and produce lower pressure gradients.[7] They are therefore more likely to stop bleeding and less likely to cause damage to underlying tissue, in addition to being significantly less painful than tourniquets with narrow straps and bands.[4][8] Overpressure protection in certain emergency tourniquets also help to prevent excessive force from damaging the limb.[1]
Risks

Possible risks of complications—morbidity—related to emergency tourniquet use include
|
Emergency care services implementing routine tourniquet use, especially in the civilian setting, should exercise caution and ensure that training is adequate for optimal results.[3] However, given proper precautions, the occurrence of complications due to tourniquet use is quite rare.[9] Designed tourniquet devices are routinely tightened over healthy limbs during training with no ill effects, and recent evidence from combat hospitals in Iraq suggests that morbidity rates are low when users adhere to standard best practices. Since no better alternatives exist for users to self-apply with only basic training, the benefit of tourniquet use far outweighs the risks.[2][3][9]
Safe tourniquet practice involves:
|
1. Careful placement of tourniquet proximal to all sites of hemorrhage. 2. Limiting tourniquet time to less than two hours, if possible. 3. Minimizing excessive applied pressure beyond the point of complete blood flow cessation.[2][9] |
Current developments

Field experience
Latest field trials suggest that wider straps are more effective and less painful than tourniquets with thinner straps. The concept of limb occlusion pressure is also gaining prominence over the misconception that greater applied force results in greater effectiveness. In addition, studies of failed cases indicate that the correct devices should be coupled with training that facilitates realistic expectations and correct user actions.[4]
Emerging needs
Despite the success of widespread tourniquet deployment to limit combat casualties, many preventable deaths from hemorrhage occur where conventional tourniquet use is inappropriate. The need exists for controlling junctional bleeding, especially in the pelvic area.[10] In 2012, the Combat Ready Clamp (CRoC) was selected by the U.S. Army Institute of Surgical Research (USAISR) for that purpose.[11] Another emerging need is more refined training regimes and doctrine based on scientific evidence, which can ensure that future tourniquet practice and policies are in line with the most current body of knowledge.[10]
Junctional hemorrhage, bleeding from the areas at the junction of the trunk and its appendages, is a difficult problem in trauma. These areas are not amenable to extremity tourniquets because the area that is bleeding will not allow placement that can create circumferential pressure around the extremity and above the wound. Junctional arterial injuries can rapidly lead to death by exsanguination prior to care in the hospital so out-of-hospital control of junctional bleeding can be lifesaving.[12]
For the study interval between October 2001 and June 2011, 4,596 battlefield fatalities were reviewed and analyzed. The stratification of mortality demonstrated that 87.3% of all injury mortality occurred pre-Military Treatment Facility (MTF). Of the pre-MTF deaths, 75.7% (n = 3,040) were classified as non-survivable, and 24.3% (n = 976) were deemed potentially survivable (PS). In this study the injury/physiologic focus of PS mortal wounding was largely associated with hemorrhage (90.9%) and the primary site of lethal hemorrhage was truncal (67.3%), followed by junctional (19.2%), and then peripheral-extremity (13.5%) hemorrhage.[13]
From the statistics cited above we can deduce that there were 976 PS patients, with 91% of those involving hemorrhage. This results in a total of 888 PS patients that died as a result of hemorrhage. From these hemorrhagic cases we find that 19.2% involved junctional hemorrhage resulting in a potentially survivable subgroup of 171 patients from this study. Therefore, if a device that can control junctional hemorrhage had been available, 171 persons with life-threatening hemorrhage from junctional regions could have been treated near the point of injury most probably resulting in reduced mortality in this subgroup. And if that junctional device were multi-site capable so it could also be used to control extremity hemorrhage if needed then perhaps more in the peripheral-extremity sub-group could have survived. Additionally it is unclear to what extent that the authors of this study categorized inter-pelvic bleeding, a common component of both amputations from blast and from blunt trauma like motor vehicle accidents, as truncal hemorrhage. However it is very clear that if a device were capable of controlling not only junctional hemorrhage but was also clearly indicated and effective for controlling inter-pelvic hemorrhage, it could potentially change which injuries are viewed as “potentially survivable” in this study and thereby further expand survivability.[14]
See also
References
- 1 2 3 4 5 6 7 Walters, Thomas J.; Wenke, Joseph C.; Kauvar, David S. (2005). "Effectiveness of Self-Applied Tourniquets in Human Volunteers". Prehospital Emergency Care. Informa Healthcare. 9 (4): 416–22. doi:10.1080/10903120500255123.
- 1 2 3 4 5 6 Kragh, John F.; Walters, Thomas J.; Baer, David G. (2008). "Practical Use of Emergency Tourniquets to Stop Bleeding in Major Limb Trauma". The Journal of Trauma. Lippincott Williams & Wilkins. 64 (2): S38–S50. doi:10.1097/TA.0b013e31816086b1. PMID 18376170.
- 1 2 3 Kragh, John F.; Walters, Thomas J.; Baer, David G. (2009). "Survival With Emergency Tourniquet Use to Stop Bleeding in Major Limb Trauma". Annals of Surgery. Lippincott Williams & Wilkins. 249 (1): 1–7. doi:10.1097/SLA.0b013e31818842ba.
- 1 2 3 Kragh, John F.; O'Neill, Michelle L.; Walters, Thomas J. (2011). "The Military Emergency Tourniquet Program's Lessons Learned With Devices and Designs". Military Medicine. Association of Military Surgeons of the U.S. 176 (10): 1144–52. doi:10.7205/milmed-d-11-00114.
- ↑ Ruterbusch, VL; Swiergosz, MJ; Montgomery, LD; Hopper, KW; Gerth, WA (2005). "ONR/MARCORSYSCOM Evaluation of Self-Applied Tourniquets for Combat Applications". United States Navy Experimental Diving Unit Technical Report. NEDU-TR-05-15. Retrieved 2008-07-22.
- ↑ Hill, JP; Montgomery, LD; Hopper, KW; Roy, LA (2007). "Evaluation of Self-Applied Tourniquets for Combat Applications, Second Phase". US Navy Experimental Diving Unit Technical Report. NEDU-TR-07-07. Retrieved 2008-07-22.
- 1 2 3 Noordin, Shahryar; McEwen, James A.; Kragh, John F. (2009). "Current Concepts Review: Surgical Tourniquets in Orthopaedics". Journal of Bone and Joint Surgery. JBJS. 91 (12): 2958–67. doi:10.2106/JBJS.I.00634. ISSN 0021-9355.
- ↑ Taylor, David M.; Vater, Gill M.; Parker, Paul J. (2011). "An Evaluation of Two Tourniquet Systems for the Control of Prehospital Lower Limb Hemorrhage". The Journal of Trauma. Lippincott Williams & Wilkins. 71 (3): 591–5. doi:10.1097/TA.0b013e31820e0e41.
- 1 2 3 Kragh, John F.; Littrel, Michelle L.; Walters, Thomas J. (2009). "Battle Casualty Survival with Emergency Tourniquet Use to Stop Limb Bleeding". The Journal of Emergency Medicine. Lippincott Williams & Wilkins. XX (2): S38–S50. doi:10.1016/j.jemermed.2009.07.022.
- 1 2 Murphy, Chris; Kragh, John F.; Dubick, Michael A. (2011). "New Tourniquet Device Concepts for Battlefield Hemorrhage Control". U.S. Army Medical Department Journal: 38–48. ISSN 1524-0436.
- ↑ "New truncal tourniquet ready for battle use".
- ↑ Croushorn, J; Thomas, G; McCord, SR (2013). "Abdominal aortic tourniquet controls junctional hemorrhage from a gunshot wound of the axilla". Journal of Special Operations Medicine. 13 (3): 1–4. PMID 24048982.
- ↑ Eastridge, Brian J.; Mabry, Robert L.; Seguin, Peter; Cantrell, Joyce; Tops, Terrill; Uribe, Paul; Mallett, Olga; Zubko, Tamara; Oetjen-Gerdes, Lynne; Rasmussen, Todd E.; Butler, Frank K.; Kotwal, Russell S.; Holcomb, John B.; Wade, Charles; Champion, Howard; Lawnick, Mimi; Moores, Leon; Blackbourne, Lorne H. (December 2012). "Death on the battlefield (2001–2011)" (PDF). Journal of Trauma and Acute Care Surgery. 73 (6): S431–S437. doi:10.1097/TA.0b013e3182755dcc. PMID 23192066. Archived from the original (PDF) on 2014-06-16.
- ↑ Pastore, Rose (2012-06-11). "2012 Invention Awards: An Inflatable Abdominal Tourniquet". Popsci.com. Popular science.