Spondylolisthesis
| Spondylolisthesis | |
|---|---|
| Synonyms | Olisthesis |
 | |
| X-ray of the lateral lumbar spine with a grade III anterolisthesis at the L5-S1 level. | |
| Pronunciation |
|
| Specialty | Orthopedics |
Spondylolisthesis is the slippage or displacement of one vertebra compared to another. Spondylolisthesis is often defined in medical textbooks as displacement in any direction.[1][2] Yet, medical dictionaries usually define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it (or the sacrum).[3][4]
Types
Olisthesis is a term that more explicitly denotes displacement in any direction.[5] Forward or anterior displacement can specifically be called anterolisthesis.[1][2] Anterolisthesis commonly involves the fifth lumbar vertebra.[6] Backward displacement is called retrolisthesis. Lateral displacement is called lateral listhesis[1] or laterolisthesis.[2]
A hangman's fracture is a specific type of spondylolisthesis where the second cervical vertebra (C2) is displaced anteriorly relative to the C3 vertebra due to fractures of the C2 vertebra's pedicles.
Anterolisthesis
Signs and symptoms
Symptoms of anterolisthesis include:
- A general stiffening of the back and a tightening of the hamstrings, with a resulting change in both posture and gait.
- A leaning-forward or semi-kyphotic posture may be seen, due to compensatory changes.
- A "waddle" may be seen in more advanced causes, due to compensatory pelvic rotation due to decreased lumbar spine rotation.
- A result of the change in gait is often a noticeable atrophy in the gluteal muscles due to lack of use.
- Generalized lower-back pain may also be seen, with intermittent shooting pain from the buttocks to the posterior thigh, and/or lower leg via the sciatic nerve.
Other symptoms may include tingling and numbness. Coughing and sneezing can intensify the pain. An individual may also note a "slipping sensation" when moving into an upright position. Sitting and trying to stand up may be painful and difficult.[7][8]
Classification
Anterolisthesis can be categorized by cause, location and severity.
By causes
- Degenerative anterolisthesis (a.k.a. type 3) is a disease of the older adult that develops as a result of facet arthritis and joint remodeling. Joint arthritis, and ligamentum flavum weakness, may result in slippage of a vertebra. Degenerative forms are more likely to occur in women, persons older than fifty, and African Americans.[9]
- Traumatic anterolisthesis is rare and results from acute fractures in the neural arch, other than the pars.[10]
- Dysplastic anterolisthesis (a.k.a. type 1) results from congenital abnormalities of the upper sacral facets or inferior facets of the fifth lumbar vertebra, and accounts for 14% to 21% of all anterolisthesis.[11]
- Isthmic anterolisthesis (a.k.a. type 2) is caused by a defect in the pars interarticularis but it can also be seen with an elongated pars.
- Pathologic anterolisthesis (a.k.a. type 5) is caused by either infection or a malignancy.
- Post-surgical/iatrogenic anterolisthesis (a.k.a. type 6) is caused by complications after surgery.
By location
Anterolisthesis location includes which vertebrae are involved, and may also specify which parts of the vertebrae are affected.
Isthmic anterolisthesis is where there is a defect in the pars interarticularis.[12] It is the most common form of spondylolisthesis; also called spondylolytic spondylolisthesis, it occurs with a reported prevalence of 5–7 percent in the US population. A slip or fracture of the intravertebral joint is usually acquired between the ages of 6 and 16 years, but remains unnoticed until adulthood. Roughly 90 percent of these isthmic slips are low-grade (less than 50 percent slip) and 10 percent are high-grade (greater than 50 percent slip).[9] It is divided into three subtypes:[13]
- A: pars fatigue fracture
- B: pars elongation due to multiple healed stress effects
- C: pars acute fracture
Severity
Classification by degree of the slippage, as measured as percentage of the width of the vertebral body:[14]
- Grade I: 0-25%
- Grade II: 25- 50%
- Grade III: 50-75%
- Grade IV: 75-100%
- Grade V: greater than 100%
 X-ray picture of a grade 1 isthmic anterolisthesis at L4-5
X-ray picture of a grade 1 isthmic anterolisthesis at L4-5 MRI of L5-S1 anterolisthesis
MRI of L5-S1 anterolisthesis- X-ray of a grade 4 anterolisthesis at L5-S1 with spinal misalignment indicated
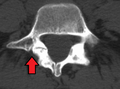 Anterolisthesis L5/S1
Anterolisthesis L5/S1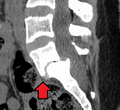 Anterolisthesis L5/S1
Anterolisthesis L5/S1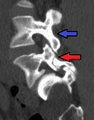 Anterolisthesis L5/S1. Blue arrow normal pars interarticularis. Red arrow is a break in pars interarticularis
Anterolisthesis L5/S1. Blue arrow normal pars interarticularis. Red arrow is a break in pars interarticularis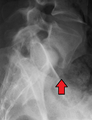 Anterolisthesis L5/S1
Anterolisthesis L5/S1
Treatment
Conservative
Patients with symptomatic isthmic anterolisthesis are initially offered conservative treatment consisting of activity modification, pharmacological intervention, and a physical therapy consultation.
- Physical therapy can evaluate and address postural and compensatory movement abnormalities.[15]
- Anti-inflammatory medications (NSAIDS) in combination with paracetamol (Tylenol) can be tried initially. If a severe radicular component is present, a short course of oral steroids such as Prednisone or Methylprednisolone can be considered. Epidural steroid injections, either interlaminal or transforaminal, performed under fluoroscopic guidance can help with severe radicular (leg) pain. Lumbosacral orthoses may be of benefit for some patients but should be used on a temporary basis to prevent spinal muscle atrophy and loss of proprioception.
Surgical
Degenerative anterolisthesis with spinal stenosis is one of the most common indications for spine surgery (typically a laminectomy) among older adults.[16] Both minimally invasive and open surgical techniques are used to treat anterolisthesis.[17]
Retrolisthesis
A retrolisthesis is a posterior displacement of one vertebral body with respect to the subjacent vertebra to a degree less than a luxation (dislocation). Retrolistheses are most easily diagnosed on lateral x-ray views of the spine. Views, where care has been taken to expose for a true lateral view without any rotation, offer the best diagnostic quality.
Retrolistheses are found most prominently in the cervical spine and lumbar region but can also be seen in the thoracic area.
History
Spondylolisthesis was first described in 1782 by Belgian obstetrician Herbinaux.[18] He reported a bony prominence anterior to the sacrum that obstructed the vagina of a small number of patients.[19] The term “spondylolisthesis” was coined in 1854 from the Greek σπονδυλος, "spondylos" = "vertebra" and ὀλισθός "olisthos" = "slipperiness," "a slip."[20]
See also
References
- 1 2 3 Introduction to chapter 17 in: Thomas J. Errico, Baron S. Lonner, Andrew W. Moulton (2009). Surgical Management of Spinal Deformities. Elsevier Health Sciences. ISBN 9781416033721.
- 1 2 3 Page 250 in: Walter R. Frontera, Julie K. Silver, Thomas D. Rizzo (2014). Essentials of Physical Medicine and Rehabilitation (3 ed.). Elsevier Health Sciences. ISBN 9780323222723.
- ↑ "spondylolisthesisplay". Merriam-Webster medical dictionary. Retrieved 2017-09-07.
- ↑ "spondylolisthesis". Farlex medical dictionary. Retrieved 2017-09-07.
, in turn citing:
- Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. Copyright date 2003
- Dorland's Medical Dictionary for Health Consumers. Copyright date 2007
- The American Heritage Medical Dictionary. Copyright date 2007
- Mosby's Medical Dictionary, 9th edition
- McGraw-Hill Concise Dictionary of Modern Medicine. Copyright date 2002
- Collins Dictionary of Medicine. Copyright date 2005
- ↑ Frank Gaillard. Radiopaedia https://radiopaedia.org/articles/olisthesis. Retrieved 2018-02-21. Missing or empty
|title=(help) - ↑ Foreman P, Griessenauer CJ, Watanabe K, Conklin M, Shoja MM, Rozzelle CJ, Loukas M, Tubbs RS (2013). "L5 spondylolysis/spondylolisthesis: a comprehensive review with an anatomic focus". Child's Nervous System. 29 (2): 209–16. doi:10.1007/s00381-012-1942-2. PMID 23089935.
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=A00588%5Bfull+citation+needed%5D
- ↑ http://www.webmd.com/back-pain/tc/spondylolisthesis-topic-overview%5Bfull+citation+needed%5D
- 1 2 "Adult Spondylolisthesis in the Low Back". American Academy of Orthopaedic Surgeons. Retrieved 9 June 2013.
- ↑ Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD (2010). "Spondylolysis: a review and reappraisal". Hippokratia. 14 (1): 17–21. PMC 2843565. PMID 20411054.
- ↑ Leone LD, Lamont DW (1999). "Diagnosis and treatment of severe dysplastic spondylolisthesis". The Journal of the American Osteopathic Association. 99 (6): 326–8. doi:10.7556/jaoa.1999.99.6.326. PMID 10405520.
- ↑ Aruna Ganju (2002). "Isthmic Spondylolisthesis". Neurosurg Focus. 13 (1).
- ↑ http://www.orthobullets.com/spine/2038/adult-isthmic-spondylolisthesis%5Bfull+citation+needed%5D
- ↑ "Spondylolysis and Spondylolisthesis of the Lumbar Spine". Massachusetts General Hospital. Retrieved 2016-12-14.
- ↑ Treatment Options for Spondylolisthesis; OrthoConsult
- ↑ Grabias S (1980). "Current concepts review. The treatment of spinal stenosis". The Journal of Bone and Joint Surgery. American Volume. 62 (2): 308–13. PMID 6987238.
- ↑ Lu VM, Kerezoudis P, Gilder HE, McCutcheon BA, Phan K, Bydon M (2017). "Minimally Invasive Surgery Versus Open Surgery Spinal Fusion for Spondylolisthesis: A Systematic Review and Meta-analysis". Spine (Phila Pa 1976). 42 (3): E177–E185. doi:10.1097/BRS.0000000000001731. PMID 27285899.
- ↑ Newman PH (1955). "Spondylolisthesis, its cause and effect". Annals of the Royal College of Surgeons of England. 16 (5): 305–23. PMC 2377893. PMID 14377314.
- ↑ Garrigues, Henry Jacques (1902). "Spondylolisthesic pelvis". A textbook of the science and art of obstetrics. pp. 490–93. OCLC 654149619.
- ↑ "Isthmic Spondylolisthesis and Spondylolysis".
External links
| Classification | |
|---|---|
| External resources |