Cold agglutinin disease
| Cold agglutinin disease | |
|---|---|
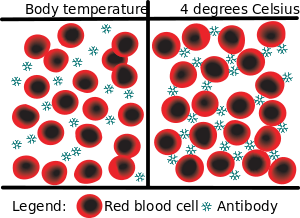 | |
| Cold agglutination - at body temperature, the antibodies do not attach to the red blood cells. At lower temperatures, however, the antibodies react to Ii antigens, bringing the red blood cells together, a process known as agglutination | |
| Specialty |
Hematology |
Cold agglutinin disease is an autoimmune disease characterized by the presence of high concentrations of circulating antibodies, usually IgM, directed against red blood cells, causing them to agglutinate and undergo lysis.[1] It is a form of autoimmune hemolytic anemia, specifically one in which antibodies bind red blood cells only at low body temperatures, typically 28–31 °C.
Cause
Cold agglutinin disease can be either primary (arising spontaneously) or secondary (a result of another pathology). The primary form is caused by excessive cell proliferation[4] of B lymphocytes.[5] Secondary cold agglutinin disease is a result of an underlying condition. In adults, this is typically due to a lymphoproliferative disease such as lymphoma and chronic lymphoid leukemia, or infection. Waldenström's macroglobulinemia may also be positive for cold agglutinins. In children, cold agglutinin disease is often secondary to an infection, such as Mycoplasma pneumonia, mononucleosis, and HIV.
Pathophysiology
All individuals have circulating antibodies directed against red blood cells, but their concentrations are often too low to trigger disease (titers under 64 at 4 °C). In individuals with cold agglutinin disease, these antibodies are in much higher concentrations (titers over 1000 at 4 °C).
At body temperatures of 28–31 °C, such as those encountered during winter months, and occasionally at body temperatures of 37 °C, antibodies (generally IgM) bind to the polysaccharide region of glycoproteins on the surface of red blood cells (typically the I antigen, i antigen, and Pr antigens). Binding of antibodies to red blood cells activates the classical pathway of the complement system. If the complement response is sufficient, red blood cells are damaged by the membrane attack complex, an effector of the complement cascade. In the formation of the membrane attack complex, several complement proteins are inserted into the red blood cell membrane, forming pores that lead to membrane instability and intravascular hemolysis (destruction of the red blood cell within the blood vessels).
If the complement response is insufficient to form membrane attack complexes, then extravascular lysis will be favored over intravascular red blood cell lysis. In lieu of the membrane attack complex, complement proteins (particularly C3b and C4b) are deposited on red blood cells. This opsonization enhances the clearance of red blood cell by phagocytes in the liver, spleen, and lungs, a process termed extravascular hemolysis.
Individuals with cold agglutinin disease present with signs and symptoms of hemolytic anemia. Those with secondary agglutinin disease may also present with an underlying disease, often autoimmune.
Diagnosis
Detection of antibodies (cold or warm) and /or complement system on RBC from the patient is a direct Coombs antiglobulin test. Detection of antibodies in serum of the patient (still circulating in the blood, that have not yet formed any complexes with RBC) is an indirect Coombs antiglobulin test.
Treatment
- Avoid cold weather.
- Treat the underlying lymphoma.
- No cold drinks; all drinks should be at room temperature (or above).
- Requires heater to maintain temperature in cold places.
See also
References
- ↑ Cold Agglutinin Disease at eMedicine
- ↑ Gertz, Moric A (2006). "Cold agglutinin disease". Haematologica. 91 (4): 439–41. PMID 16585009.
- ↑ Dacie, J. V.; Crookston, J. H.; Christenson, W. N. (1957). "'Incomplete' Cold Antibodies: Role of Complement in Sensitization to Antiglobulin Serum by Potentially Haemolytic Antibodies". British Journal of Haematology. 3 (1): 77–87. doi:10.1111/j.1365-2141.1957.tb05773.x. PMID 13413095.
- ↑ Berentsen, Sigbjørn; Tjønnfjord, Geir E. (2012). "Diagnosis and treatment of cold agglutinin mediated autoimmune hemolytic anemia". Blood Reviews. 26 (3): 107–15. doi:10.1016/j.blre.2012.01.002. PMID 22330255.
- ↑ Berentsen, Sigbjørn; Randen, Ulla; Tjønnfjord, Geir E. (2015). "Cold Agglutinin-Mediated Autoimmune Hemolytic Anemia". Hematology/Oncology Clinics of North America. 29 (3): 455–71. doi:10.1016/j.hoc.2015.01.002. PMID 26043385.
- ↑ Berentsen, Sigbjørn; Ulvestad, Elling; Gjertsen, Bjørn Tore; Hjorth-Hansen, Henrik; Langholm, Ruth; Knutsen, Håvar; Ghanima, Waleed; Shammas, Fuad Victor; Tjønnfjord, Geir E. (2004). "Rituximab for primary chronic cold agglutinin disease: a prospective study of 37 courses of therapy in 27 patients". Blood. 103 (8): 2925–8. doi:10.1182/blood-2003-10-3597. PMID 15070665.
External links
| Classification | |
|---|---|
| External resources |