Severe acute respiratory syndrome
Severe acute respiratory syndrome (SARS) is a viral respiratory disease of zoonotic origin that surfaced in the early 2000s caused by severe acute respiratory syndrome coronavirus (SARS-CoV or SARS-CoV-1), the first-identified strain of the SARS coronavirus species severe acute respiratory syndrome-related coronavirus (SARSr-CoV). The syndrome caused the 2002–2004 SARS outbreak. In late 2017, Chinese scientists traced the virus through the intermediary of civets to cave-dwelling horseshoe bats in Yunnan province.[2] No cases of the first SARS-CoV have been reported worldwide since 2004.[3]
| Severe acute respiratory syndrome (SARS) | |
|---|---|
 | |
| Electron micrograph of SARS coronavirus virion | |
| Pronunciation |
|
| Specialty | Infectious disease |
| Symptoms | Fever, dry cough, headache, muscle aches and difficulty breathing |
| Complications | Acute Respiratory Distress Syndrome (ARDS) with other comorbidities that eventually leads to death |
| Prevention | Hand washing, cough etiquette, avoiding close contact with affected people, avoiding travel to affected areas[1] |
| Prognosis | 9.5% chance of death (all countries) |
| Frequency | 8,098 cases |
| Deaths | 774 |
In 2019, a related virus strain, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was discovered. This new strain causes COVID-19, a disease which brought about the 2019–20 coronavirus pandemic.[4]
Signs and symptoms
Symptoms are flu-like symptoms and may include fever, muscle pain, lethargy, cough, sore throat, and other nonspecific symptoms. The only symptom common to all patients appears to be a fever above 38 °C (100 °F). SARS may eventually lead to shortness of breath and pneumonia; either direct viral pneumonia or secondary bacterial pneumonia.
The average incubation period for SARS is 4–6 days, although rarely it could be as short as 1 day or as long as 14 days.[5]
Transmission
The primary route of transmission for SARS-CoV is contact of the mucous membranes with respiratory droplets or fomites. While diarrhea is common in people with SARS, the fecal–oral route does not appear to be a common mode of transmission.[5] The basic reproduction number of SARS-CoV, R0, ranges from 2 to 4 depending on different analyses. Control measures introduced in April 2003 reduced the R to 0.4.[5]
Diagnosis
SARS-CoV may be suspected in a patient who has:
- Any of the symptoms, including a fever of 38 °C (100 °F) or higher, and
- Either a history of:
- Contact (sexual or casual) with someone with a diagnosis of SARS within the last 10 days or
- Travel to any of the regions identified by the World Health Organization (WHO) as areas with recent local transmission of SARS.
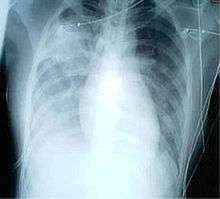
For a case to be considered probable, a chest X-ray must be positive for atypical pneumonia or respiratory distress syndrome.
The WHO has added the category of "laboratory confirmed SARS" for patients who would otherwise be considered "probable" but who have not yet had a positive chest X-ray changes, but have tested positive for SARS based on one of the approved tests (ELISA, immunofluorescence or PCR).[6]
The appearance of SARS-CoV in chest X-rays is not always uniform but generally appears as an abnormality with patchy infiltrates.[7]
Prevention
There is no vaccine for SARS, although doctor Anthony Fauci mentioned that the CDC developed one and placed it in the US national stockpile.[8] Clinical isolation and quarantine remain the most effective means to prevent the spread of SARS. Other preventive measures include:
- Hand-washing with soap and water, or use of alcohol-based hand sanitizer[9]
- Disinfection of surfaces of fomites to remove viruses
- Avoiding contact with bodily fluids
- Washing the personal items of someone with SARS in hot, soapy water (eating utensils, dishes, bedding, etc.)[10]
- Keeping children with symptoms home from school
- Simple hygiene measures
- Isolating oneself as much as possible to minimize the chances of transmission of the virus
Many public health interventions were made to try to control the spread of the disease, which is mainly spread through respiratory droplets in the air. These interventions included earlier detection of the disease; isolation of people who are infected; droplet and contact precautions; and the use of personal protective equipment (PPE), including masks and isolation gowns.[11] Studies done during the outbreak found that for medical professionals, wearing any type of mask compared to none could reduce the chances of getting sick by about 80%. A screening process was also put in place at airports to monitor air travel to and from affected countries.[12]
SARS-CoV is most infectious in severely ill patients, which usually occurs during the second week of illness. This delayed infectious period meant that quarantine was highly effective; people who were isolated before day five of their illness rarely transmitted the disease to others.[5]
Although no cases have been identified since 2004, the CDC was still working to make federal and local rapid response guidelines and recommendations in the event of a reappearance of the virus as of 2017.[13]
Treatment

As SARS is a viral disease, antibiotics do not have direct effect but may be used against bacterial secondary infection. Treatment of SARS is mainly supportive with antipyretics, supplemental oxygen and mechanical ventilation as needed. Antiviral medications are used as well as high doses of steroids to reduce swelling in the lungs.
People with SARS-CoV must be isolated, preferably in negative-pressure rooms, with complete barrier nursing precautions taken for any necessary contact with these patients, to limit the chances of medical personnel getting infected with SARS. In certain cases, natural ventilation by opening doors and windows are documented to help decreasing indoor concentration of virus particles.[14]
Some of the more serious damage caused by SARS may be due to the body's own immune system reacting in what is known as cytokine storm.[15]
As of 2020, there is no cure or protective vaccine for SARS that has been shown to be both safe and effective in humans.[16][17] According to research papers published in 2005 and 2006, the identification and development of novel vaccines and medicines to treat SARS is a priority for governments and public health agencies around the world.[18][19][20] In early 2004, an early clinical trial on volunteers was planned.[21]
Prognosis
Several consequent reports from China on some recovered SARS patients showed severe long-time sequelae. The most typical diseases include, among other things, pulmonary fibrosis, osteoporosis, and femoral necrosis, which have led in some cases to the complete loss of working ability or even self-care ability of people who have recovered from SARS. As a result of quarantine procedures, some of the post-SARS patients have been documented as suffering from post-traumatic stress disorder (PTSD) and major depressive disorder.[22][23]
Epidemiology
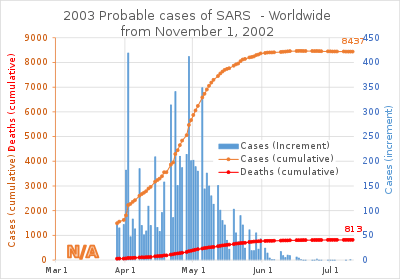
SARS was a relatively rare disease; at the end of the epidemic in June 2003, the incidence was 8,422 cases with a case fatality rate (CFR) of 11%.[11]
The case fatality rate (CFR) ranges from 0% to 50% depending on the age group of the patient.[5] Patients under 24 were least likely to die (less than 1%); those 65 and older were most likely to die (over 55%).[24]
As with MERS and COVID-19, SARS resulted in significantly more deaths of males than females.
| Country or region | Cases | Deaths | Fatality (%) | |
|---|---|---|---|---|
| 5,327 | 349 | 6.6 | ||
| 1,755 | 299 | 17.0 | ||
| 346 | 73[26][27] | 21.1 | ||
| 251 | 43 | 17.1 | ||
| 238 | 33 | 13.9 | ||
| 63 | 5 | 7.9 | ||
| 27 | 0 | 0 | ||
| 14 | 2 | 14.3 | ||
| 9 | 2 | 22.2 | ||
| 9 | 0 | 0 | ||
| 9 | 0 | 0 | ||
| 7 | 1 | 14.3 | ||
| 6 | 0 | 0 | ||
| 5 | 2 | 40.0 | ||
| 5 | 0 | 0 | ||
| 4 | 0 | 0 | ||
| 4 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 1 | 1 | 100.0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| 1 | 0 | 0 | ||
| Total excluding China[lower-alpha 1] | 2,769 | 454 | 16.4 | |
| Total (29 territories) | 8,096 | 774 | 9.6 | |
| ||||
Outbreak in South China
The viral outbreak can be genetically traced to a colony of cave-dwelling horseshoe bats in China's Yunnan province.[28]
The SARS epidemic appears to have started in Guangdong Province, China, in November 2002 where the first case was reported that same month. The patient, a farmer from Shunde, Foshan, Guangdong, was treated in the First People's Hospital of Foshan. The patient died soon after, and no definite diagnosis was made on his cause of death. Despite taking some action to control it, Chinese government officials did not inform the World Health Organization of the outbreak until February 2003. This lack of openness caused delays in efforts to control the epidemic, resulting in criticism of the People's Republic of China from the international community. China officially apologized for early slowness in dealing with the SARS epidemic.[29]
The outbreak first appeared on 27 November 2002, when Canada's Global Public Health Intelligence Network (GPHIN), an electronic warning system that is part of the World Health Organization's Global Outbreak Alert and Response Network (GOARN), picked up reports of a "flu outbreak" in China through Internet media monitoring and analysis and sent them to the WHO. While GPHIN's capability had recently been upgraded to enable Arabic, Chinese, English, French, Russian, and Spanish translation, the system was limited to English or French in presenting this information. Thus, while the first reports of an unusual outbreak were in Chinese, an English report was not generated until 21 January 2003.[30][31] The first super-spreader was admitted to the Sun Yat-sen Memorial Hospital in Guangzhou on 31 January, which soon spread the disease to nearby hospitals.[32]
Subsequent to this, the WHO requested information from Chinese authorities on 5 and 11 December. Despite the successes of the network in previous outbreaks of diseases, it did not receive intelligence until the media reports from China several months after the outbreak of SARS. Along with the second alert, WHO released the name, definition, as well as an activation of a coordinated global outbreak response network that brought sensitive attention and containment procedures.[33] By the time the WHO took action, over 500 deaths and an additional 2,000 cases had already occurred worldwide.[31]
In early April 2003, after Jiang Yanyong pushed to report the danger to China,[34][35] there appeared to be a change in official policy when SARS began to receive a much greater prominence in the official media. Some have directly attributed this to the death of American James Earl Salisbury.[36] It was around this same time that Jiang Yanyong made accusations regarding the undercounting of cases in Beijing military hospitals.[34][35] After intense pressure, Chinese officials allowed international officials to investigate the situation there. This revealed problems plaguing the aging mainland Chinese healthcare system, including increasing decentralization, red tape, and inadequate communication.
Many healthcare workers in the affected nations risked and lost their lives by treating patients, and trying to contain the infection before ways to prevent infection were known.[37]
Spread to other regions
The epidemic reached the public spotlight in February 2003, when an American businessman traveling from China, Johnny Chen, became afflicted with pneumonia-like symptoms while on a flight to Singapore. The plane stopped in Hanoi, Vietnam, where the victim died in Hanoi French Hospital. Several of the medical staff who treated him soon developed the same disease despite basic hospital procedures. Italian doctor Carlo Urbani identified the threat and communicated it to WHO and the Vietnamese government; he later succumbed to the disease.[38]
The severity of the symptoms and the infection among hospital staff alarmed global health authorities, who were fearful of another emergent pneumonia epidemic. On 12 March 2003, the WHO issued a global alert, followed by a health alert by the United States Centers for Disease Control and Prevention (CDC). Local transmission of SARS took place in Toronto, Ottawa, San Francisco, Ulaanbaatar, Manila, Singapore, Taiwan, Hanoi and Hong Kong whereas within China it spread to Guangdong, Jilin, Hebei, Hubei, Shaanxi, Jiangsu, Shanxi, Tianjin, and Inner Mongolia.
Hong Kong

The disease spread in Hong Kong from Liu Jianlun, a Guangdong doctor who was treating patients at Sun Yat-Sen Memorial Hospital.[39] He arrived in February and stayed on the ninth floor of the Metropole Hotel in Kowloon, infecting 16 of the hotel visitors. Those visitors traveled to Canada, Singapore, Taiwan, and Vietnam, spreading SARS to those locations.[40]
Another larger cluster of cases in Hong Kong centred on the Amoy Gardens housing estate. Its spread is suspected to have been facilitated by defects in its bathroom drainage system that allowed sewer gases including virus particles to vent into the room. Bathroom fans exhausted the gases and wind carried the contagion to adjacent downwind complexes. Concerned citizens in Hong Kong worried that information was not reaching people quickly enough and created a website called sosick.org, which eventually forced the Hong Kong government to provide information related to SARS in a timely manner.[41] The first cohort of affected people were discharged from hospital on 29 March 2003.[42]
Toronto
The first case of SARS in Toronto was identified on 23 February 2003.[43] Beginning with an elderly woman, Kwan Sui-Chu, returning from a trip to Hong Kong, the virus killed her on 5 March and eventually infected 257 individuals in the province of Ontario. The trajectory of this outbreak is typically divided into two phases, the first centring around her son Tse Chi Kwai, who infected other patients at the Scarborough Grace Hospital and died on 13 March. The second major wave of cases was clustered around accidental exposure among patients, visitors, and staff within the North York General Hospital. The WHO officially removed Toronto from its list of infected areas by the end of June 2003.[44]
The official response by the Ontario provincial government and Canadian federal government has been widely criticized in the years following the outbreak. Brian Schwartz, vice-chair of Ontario's SARS Scientific Advisory Committee, described public health officials' preparedness and emergency response at the time of the outbreak as "very, very basic and minimal at best".[45] Critics of the response often cite poorly outlined and enforced protocol for protecting healthcare workers and identifying infected patients as a major contributing factor to the continued spread of the virus. The atmosphere of fear and uncertainty surrounding the outbreak resulted in staffing issues in area hospitals when healthcare workers elected to resign rather than risk exposure to SARS.
Identification of virus
In late February 2003, Italian doctor Carlo Urbani was called into The French Hospital of Hanoi to look at Johnny Chen, an American businessman who had fallen ill with what doctors thought was a bad case of influenza. Urbani realized that Chen's ailment was probably a new and highly contagious disease. He immediately notified the WHO. He also persuaded the Vietnamese Health Ministry to begin isolating patients and screening travelers, thus slowing the early pace of the epidemic. He subsequently contracted the disease himself, and died in March 2003.
The CDC and Canada's National Microbiology Laboratory identified the SARS genome in April 2003.[46][47] Scientists at Erasmus University in Rotterdam, the Netherlands demonstrated that the SARS coronavirus fulfilled Koch's postulates thereby confirming it as the causative agent. In the experiments, macaques infected with the virus developed the same symptoms as human SARS victims.[48]
In late May 2003, studies were conducted using samples of wild animals sold as food in the local market in Guangdong, China. The results found that the SARS coronavirus could be isolated from masked palm civets (Paguma sp.), even if the animals did not show clinical signs of the virus. The preliminary conclusion was the SARS virus crossed the xenographic barrier from asian palm civet to humans, and more than 10,000 masked palm civets were killed in Guangdong Province. The virus was also later found in raccoon dogs (Nyctereuteus sp.), ferret badgers (Melogale spp.), and domestic cats. In 2005, two studies identified a number of SARS-like coronaviruses in Chinese bats.[49][50]
Phylogenetic analysis of these viruses indicated a high probability that SARS coronavirus originated in bats and spread to humans either directly or through animals held in Chinese markets. The bats did not show any visible signs of disease but are the likely natural reservoirs of SARS-like coronaviruses. In late 2006, scientists from the Chinese Centre for Disease Control and Prevention of Hong Kong University and the Guangzhou Centre for Disease Control and Prevention established a genetic link between the SARS coronavirus appearing in civets and humans, bearing out claims that the disease had jumped across species.[51]
In December 2017, "after years of searching across China, where the disease first emerged, researchers reported ... that they had found a remote cave in Yunnan province, which is home to horseshoe bats that carry a strain of a particular virus known as a coronavirus. This strain has all the genetic building blocks of the type that triggered the global outbreak of SARS in 2002." The research was performed by Shi Zheng-Li, Cui Jie and coworkers at the Wuhan Institute of Virology, China, and published in PLOS Pathogens. The authors are quoted as stating that "another deadly outbreak of SARS could emerge at any time. As they point out, the cave where they discovered their strain is only a kilometre from the nearest village."[2]
Date of containment
The World Health Organization declared severe acute respiratory syndrome contained on 5 July 2003. In the following years, four SARS cases were reported in China between December 2003 and January 2004. There were also three separate laboratory accidents that resulted in infection. In one of these cases, an ill lab worker spread the virus to several other people.[52][53] Study of live SARS specimens requires a biosafety level 3 (BSL-3) facility; some studies of inactivated SARS specimens can be done at biosafety level 2 facilities.[54]
Animals
A small number of cats and dogs tested positive for the virus during the outbreak. However, these animals did not transmit the virus to other animals of the same species or to humans.[55][56]
Society and culture
Fear of contracting the virus from consuming infected wild animals resulted in public bans and reduced business for meat markets in southern China and Hong Kong.[57]
See also
- Avian influenza
- Bat-borne virus
- Health crisis
- Health in China
- List of medical professionals who died during the SARS outbreak
- Middle East respiratory syndrome – a coronavirus discovered in June 2012 in Saudi Arabia
- SARS conspiracy theory
- Severe acute respiratory syndrome coronavirus 2
- Zhong Nanshan
- 2009 swine flu pandemic
References
- "SARS (severe acute respiratory syndrome) - NHS". Nhs.uk. 24 October 2019. Retrieved 22 April 2020.
- McKie, Robin (10 December 2017). "Scientists trace 2002 Sars virus to colony of cave-dwelling bats in China". The Guardian. ISSN 0029-7712. Retrieved 10 December 2017.
- "SARS (severe acute respiratory syndrome)". NHS Choices. UK National Health Service. 3 October 2014. Retrieved 8 March 2016.
Since 2004, there haven't been any known cases of SARS reported anywhere in the world.
- "Myth busters". WHO.int. World Health Organization. 2019. Retrieved 15 March 2020.
- Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). World Health Organization. 2003. hdl:10665/70863.
- Chan, Paul K. S; To, Wing-Kin; Ng, King-Cheung; Lam, Rebecca K. Y; Ng, Tak-Keung; Chan, Rickjason C. W; Wu, Alan; Yu, Wai-Cho; Lee, Nelson; Hui, David S. C; Lai, Sik-To; Hon, Ellis K. L; Li, Chi-Kong; Sung, Joseph J. Y; Tam, John S (2004). "Laboratory Diagnosis of SARS". Emerging Infectious Diseases. 10 (5): 825–31. doi:10.3201/eid1005.030682. PMC 3323215. PMID 15200815.
- Lu, P; Zhou, B; Chen, X; Yuan, M; Gong, X; Yang, G; Liu, J; Yuan, B; Zheng, G; Yang, G; Wang, H (2003). "Chest X-ray imaging of patients with SARS". Chinese Medical Journal. 116 (7): 972–5. PMID 12890364.
- "Pandemic Preparedness in the Next Administration: Keynote Address by Anthony S. Fauci". YouTube. 14 February 2017. Retrieved 22 April 2020.
- Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894 (2009). WHO-recommended handrub formulations. World Health Organization.CS1 maint: numeric names: authors list (link)
- "SARS: Prevention". MayoClinic.com. 6 January 2011. Retrieved 14 July 2013.
- Chan-Yeung, M; Xu, RH (November 2003). "SARS: epidemiology". Respirology (Carlton, Vic.). 8 Suppl: S9–14. doi:10.1046/j.1440-1843.2003.00518.x. PMID 15018127.
- "SARS (severe acute respiratory syndrome)". nhs.uk. 19 October 2017. Retrieved 1 December 2017.
- "SARS" (PDF). Retrieved 1 December 2017.
- Nakashima, Ellen (5 May 2003). "Vietnam Took Lead In Containing SARS". Washington Post.
- Perlman, Stanley; Dandekar, Ajai A (2005). "Immunopathogenesis of coronavirus infections: Implications for SARS". Nature Reviews Immunology. 5 (12): 917–27. doi:10.1038/nri1732. PMC 7097326. PMID 16322745.
- Jiang, Shibo; Lu, Lu; Du, Lanying (2013). "Development of SARS vaccines and therapeutics is still needed". Future Virology. 8 (1): 1–2. doi:10.2217/fvl.12.126. PMC 7079997. PMID 32201503.
- "SARS (severe acute respiratory syndrome)". nhs.uk. 19 October 2017. Retrieved 31 January 2020.
- Greenough, Thomas C; Babcock, Gregory J; Roberts, Anjeanette; Hernandez, Hector J; Thomas, Jr, William D; Coccia, Jennifer A; Graziano, Robert F; Srinivasan, Mohan; Lowy, Israel; Finberg, Robert W; Subbarao, Kanta; Vogel, Leatrice; Somasundaran, Mohan; Luzuriaga, Katherine; Sullivan, John L; Ambrosino, Donna M (2005). "Development and Characterization of a Severe Acute Respiratory Syndrome–Associated Coronavirus–Neutralizing Human Monoclonal Antibody That Provides Effective Immunoprophylaxis in Mice" (PDF). The Journal of Infectious Diseases. 191 (4): 507–14. doi:10.1086/427242. PMID 15655773.
- Tripp, Ralph A; Haynes, Lia M; Moore, Deborah; Anderson, Barbara; Tamin, Azaibi; Harcourt, Brian H; Jones, Les P; Yilla, Mamadi; Babcock, Gregory J; Greenough, Thomas; Ambrosino, Donna M; Alvarez, Rene; Callaway, Justin; Cavitt, Sheana; Kamrud, Kurt; Alterson, Harold; Smith, Jonathan; Harcourt, Jennifer L; Miao, Congrong; Razdan, Raj; Comer, James A; Rollin, Pierre E; Ksiazek, Thomas G; Sanchez, Anthony; Rota, Paul A; Bellini, William J; Anderson, Larry J (2005). "Monoclonal antibodies to SARS-associated coronavirus (SARS-CoV): Identification of neutralizing and antibodies reactive to S, N, M and E viral proteins". Journal of Virological Methods. 128 (1–2): 21–8. doi:10.1016/j.jviromet.2005.03.021. PMID 15885812.
- Roberts, Anjeanette; Thomas, William D; Guarner, Jeannette; Lamirande, Elaine W; Babcock, Gregory J; Greenough, Thomas C; Vogel, Leatrice; Hayes, Norman; Sullivan, John L; Zaki, Sherif; Subbarao, Kanta; Ambrosino, Donna M (2006). "Therapy with a Severe Acute Respiratory Syndrome–Associated Coronavirus–Neutralizing Human Monoclonal Antibody Reduces Disease Severity and Viral Burden in Golden Syrian Hamsters". The Journal of Infectious Diseases. 193 (5): 685–92. doi:10.1086/500143. PMID 16453264.
- Miller, John Dudley (20 January 2004). "China in SARS vaccine trial". The Scientist Magazine. Retrieved 31 January 2020.
- Hawryluck, Laura; Gold, Wayne L; Robinson, Susan; Pogorski, Stephen; Galea, Sandro; Styra, Rima (2004). "SARS Control and Psychological Effects of Quarantine, Toronto, Canada". Emerging Infectious Diseases. 10 (7): 1206–12. doi:10.3201/eid1007.030703. PMC 3323345. PMID 15324539.
- Ma Jinyu (15 July 2009). "(Silence of the Post-SARS Patients)" (in Chinese). Southern People Weekly. Retrieved 3 August 2013.
- Monaghan, Karen J. (2004). SARS: Down But Still a Threat. National Academies Press (US).
- "Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003". World Health Organization. 21 April 2004.
- "衛生署針對報載SARS死亡人數有極大差異乙事提出說明" (in Chinese). 台灣衛生福利部疾病管制署. 16 June 2003.
- "十年前SARS流行 346人感染73死亡" (in Chinese). 公視. 24 April 2013.
- McKie, Robin (10 December 2017), "Scientists trace 2002 Sars virus to colony of cave-dwelling bats in China", The Guardian
- "WHO targets SARS 'super spreaders'". CNN. 6 April 2003. Archived from the original on 7 March 2006. Retrieved 5 July 2006.
- Mawudeku, Abla; Blench, Michael (2005). "Global Public Health Intelligence Network" (PDF). Public Health Agency of Canada.
- Rodier, G (10 February 2004). "Global Surveillance, National Surveillance, and SARS". Emerging Infectious Diseases. 10 (2): 173–5. doi:10.3201/eid1002.031038. PMC 3322938. PMID 15040346.
- Abraham, Thomas (2004). Twenty-first Century Plague: The Story of SARS.
- Heymann, 2003
- Joseph Kahn (12 July 2007). "China bars U.S. trip for doctor who exposed SARS cover-up". The New York Times. Retrieved 3 August 2013.
- "The 2004 Ramon Magsaysay Awardee for Public Service". Ramon Magsaysay Foundation. 31 August 2004. Archived from the original on 14 June 2007. Retrieved 3 May 2013.
- "SARS death leads to China dispute". CNN. 10 April 2003. Archived from the original on 28 November 2007. Retrieved 3 April 2007.
- Fong, Kevin (16 August 2013). "They risked their lives to stop Sars" – via www.bbc.co.uk.
- "WHO | Dr. Carlo Urbani of the World Health Organization dies of SARS". www.who.int. Retrieved 29 November 2017.
- "Inside the hospital where Patient Zero was infected". South China Morning Post. 27 March 2003. Retrieved 23 May 2018.
- "Sr. Irene Martineau". Oxford Medical School Gazette. Archived from the original on 10 October 2008. Retrieved 10 November 2008. Cite journal requires
|journal=(help) - "Hong Kong Residents Share SARS Information Online". NPR.org. Retrieved 11 May 2016.
- "Severe Acute Respiratory Syndrome (SARS) overview". News Medical Life Sciences. AZO network. 24 April 2004.
- "Update: Severe Acute Respiratory Syndrome --- Toronto, Canada, 2003". www.cdc.gov. Retrieved 11 May 2016.
- Low, Donald (2004). Learning from SARS: Preparing for the Next Disease Outbreak: Workshop Summary.
- "Is Canada ready for MERS? 3 lessons learned from SARS". www.cbc.ca. Retrieved 11 May 2016.
- "Remembering SARS: A Deadly Puzzle and the Efforts to Solve It". Centers for Disease Control and Prevention. 11 April 2013. Retrieved 3 August 2013.
- "Coronavirus never before seen in humans is the cause of SARS". United Nations World Health Organization. 16 April 2006. Retrieved 5 July 2006.
- Fouchier, Ron A. M; Kuiken, Thijs; Schutten, Martin; Van Amerongen, Geert; Van Doornum, Gerard J. J; Van Den Hoogen, Bernadette G; Peiris, Malik; Lim, Wilina; Stöhr, Klaus; Osterhaus, Albert D. M. E (2003). "Aetiology: Koch's postulates fulfilled for SARS virus". Nature. 423 (6937): 240. Bibcode:2003Natur.423..240F. doi:10.1038/423240a. PMC 7095368. PMID 12748632.
- Li, W; Shi, Zhengli; Yu, Meng; Ren, Wuze; Smith, Craig; Epstein, Jonathan H; Wang, Hanzhong; Crameri, Gary; Hu, Zhihong; Zhang, Huajun; Zhang, Jianhong; McEachern, Jennifer; Field, Hume; Daszak, Peter; Eaton, Bryan T; Zhang, Shuyi; Wang, Lin-Fa (2005). "Bats Are Natural Reservoirs of SARS-Like Coronaviruses". Science. 310 (5748): 676–9. Bibcode:2005Sci...310..676L. doi:10.1126/science.1118391. PMID 16195424.
- Lau, S. K. P; Woo, P. C. Y; Li, K. S. M; Huang, Y; Tsoi, H.-W; Wong, B. H. L; Wong, S. S. Y; Leung, S.-Y; Chan, K.-H; Yuen, K.-Y (2005). "Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats". Proceedings of the National Academy of Sciences. 102 (39): 14040–5. Bibcode:2005PNAS..10214040L. doi:10.1073/pnas.0506735102. PMC 1236580. PMID 16169905.
- "Scientists prove SARS-civet cat link". China Daily. 23 November 2006.
- "SARS 2013: 10 Years Ago SARS Went Around the World, Where is It Now?". 11 March 2013.
- "WHO | SARS outbreak contained worldwide". www.who.int. Retrieved 16 October 2015.
- "SARS | Guidance | Lab Biosafety for Handling and Processing Specimens | CDC". www.cdc.gov. Retrieved 11 September 2017.
- "Coronavirus: Italy and Iran close schools and universities - BBC News". Bbc.co.uk. 4 March 2020. Retrieved 31 March 2020.
- "Expert reaction to reports that the (Previously reported) pet dog in Hong Kong has repeatedly tested 'weak positive' for COVID-19 virus | Science Media Centre".
- Zhan, MEI (2005). "Civet Cats, Fried Grasshoppers, and David Beckham's Pajamas: Unruly Bodies after SARS". American Anthropologist. 107 (1): 31–42. doi:10.1525/aa.2005.107.1.031. JSTOR 3567670.
Further reading
- Sihoe, Alan D.L; Wong, Randolph H.L; Lee, Alex T.H; Lau, Lee Sung; Leung, Natalie Y.Y; Law, Kin Ip; Yim, Anthony P.C (2004). "Severe Acute Respiratory Syndrome Complicated by Spontaneous Pneumothorax". Chest. 125 (6): 2345–51. doi:10.1378/chest.125.6.2345. PMC 7094543. PMID 15189961.
- Enserink, M (2013). "War Stories". Science. 339 (6125): 1264–8. doi:10.1126/science.339.6125.1264. PMID 23493690.
- Enserink, M (2013). "SARS: Chronology of the Epidemic". Science. 339 (6125): 1266–71. Bibcode:2013Sci...339.1266E. doi:10.1126/science.339.6125.1266. PMID 23493691.
- Normile, D (2013). "Understanding the Enemy". Science. 339 (6125): 1269–73. Bibcode:2013Sci...339.1269N. doi:10.1126/science.339.6125.1269. PMID 23493692.
External links
| Library resources about Severe acute respiratory syndrome |
| Wikimedia Commons has media related to SARS. |
- MedlinePlus: Severe Acute Respiratory Syndrome News, links and information from The United States National Library of Medicine
- Severe Acute Respiratory Syndrome (SARS) Symptoms and treatment guidelines, travel advisory, and daily outbreak updates, from the World Health Organization (WHO)
- Severe Acute Respiratory Syndrome (SARS): information on the international outbreak of the illness known as severe acute respiratory syndrome (SARS), provided by the US Centers for Disease Control
| Classification | |
|---|---|
| External resources |
|