Reserpine
Reserpine is a drug that is used for the treatment of high blood pressure, usually in combination with a thiazide diuretic or vasodilator.[1] Large clinical trials have shown that combined treatment with reserpine plus a thiazide diuretic reduces mortality of people with hypertension. Although the use of reserpine as a solo drug has declined since it was first approved by the FDA in 1955,[2] a review recommends use of reserpine and a thiazide diuretic or vasodilator in patients who do not achieve adequate lowering of blood pressure with first-line drug treatment alone.[3] The reserpine-hydrochlorothiazide combo pill was the 17th most commonly prescribed of the 43 combination antihypertensive pills available In 2012.[4]
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Consumer Drug Information |
| MedlinePlus | a601107 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 50% |
| Metabolism | gut/liver |
| Elimination half-life | phase 1 = 4.5h, phase 2 = 271h, average = 33h |
| Excretion | 62% feces / 8% urine |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.044 |
| Chemical and physical data | |
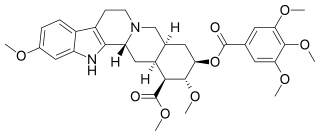
| Formula | C33H40N2O9 |
| Molar mass | 608.68 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
InChI
| |
| (verify) | |
The antihypertensive actions of reserpine are largely due to its antinoradrenergic effects, which are a result of its ability to deplete catecholamines (among other monoamine neurotransmitters) from peripheral sympathetic nerve endings. These substances are normally involved in controlling heart rate, force of cardiac contraction and peripheral vascular resistance.[5]
At doses of 0.05 to 0.2 mg per day, reserpine is well tolerated;[6] the most common adverse effect being nasal stuffiness.
Reserpine has also been used for relief of psychotic symptoms.[7] A review found that in persons with schizophrenia, reserpine and chlorpromazine had similar rates of adverse effects, but that reserpine was less effective than chlorpromazine for improving a person's global state.[8]
Mechanism of action
Reserpine irreversibly blocks the H+-coupled vesicular monoamine transporters, VMAT1 and VMAT2. VMAT1 is mostly expressed in neuroendocrine cells. VMAT2 is mostly expressed in neurons. Thus, it is the blockade of neuronal VMAT2 by reserpine that inhibits uptake and reduces stores of the monoamine neurotransmitters norepinephrine, dopamine, serotonin and histamine in the synaptic vesicles of neurons.[9] VMAT2 normally transports free intracellular norepinephrine, serotonin, and dopamine in the presynaptic nerve terminal into presynaptic vesicles for subsequent release into the synaptic cleft ("exocytosis"). Unprotected neurotransmitters are metabolized by MAO (as well as by COMT), attached to the outer membrane of the mitochondria in the cytosol of the axon terminals, and consequently never excite the post-synaptic cell. Thus, reserpine increases removal of monoamine neurotransmitters from neurons, decreasing the size of the neurotransmitter pools, and thereby decreasing the amplitude of neurotransmitter release.[10]
It may take the body days to weeks to replenish the depleted VMATs, so reserpine's effects are long-lasting.
Biosynthetic pathway
Reserpine is one of dozens of indole alkaloids isolated from the plant Rauvolfia serpentina.[11] In the Rauvolfia plant, tryptophan is the starting material in the biosynthetic pathway of reserpine, and is converted to tryptamine by tryptophan decarboxylase enzyme. Tryptamine is combined with secologanin in the presence of strictosidine synthetase enzyme and yields strictosidine. Various enzymatic conversion reactions lead to the synthesis of reserpine from strictosidine.[12]
History
Reserpine was isolated in 1952 from the dried root of Rauvolfia serpentina (Indian snakeroot),[13] which had been known as Sarpagandha and had been used for centuries in India for the treatment of insanity, as well as fever and snakebites[14] — Mahatma Gandhi used it as a tranquilizer.[15] It was first used in the United States by Robert Wallace Wilkins in 1950. Its molecular structure was elucidated in 1953 and natural configuration published in 1955.[16] It was introduced in 1954, two years after chlorpromazine.[17] The first total synthesis was accomplished by R. B. Woodward in 1958.[16]
Reserpine was also highly influential in promoting the thought of a biogenic amine hypothesis of depression.[18] Reserpine-mediated depletion of monoamine neurotransmitters in the synapses is often cited as evidence to the theory that depletion of the monoamine neurotransmitters causes subsequent depression in humans (c.f. monoamine hypothesis). However, this claim is not without controversy. The reserpine-induced depression is considered by some researchers to be a myth, while others claim that teas made out of the plant roots containing reserpine have a calming, sedative action that can actually be considered antidepressant.[19] Notably, reserpine was the first compound shown to be an effective antidepressant in a randomized placebo-controlled trial.[20]
Uses today
Medical Usage
Reserpine is recommended as an alternative drug for treating hypertension by the JNC 8.[21] A 2016 Cochrane review found reserpine to be as effective as other first-line antihypertensive drugs for lowering of blood pressure.[22] The reserpine - thiazide diuretic combination is one of the few drug treatments shown to reduce mortality in randomized controlled trials: The Hypertension Detection and Follow-up Program,[23] the Veterans Administration Cooperative Study Group in Anti-hypertensive Agents,[24] and the Systolic Hypertension in the Elderly Program.[25] Moreover, reserpine was included as a secondary antihypertensive option for patients who did not achieve blood pressure lowering targets in the ALLHAT study.[26]
It was previously used to treat symptoms of dyskinesia in patients suffering from Huntington's disease,[27] but alternative medications are preferred today.[28]
The daily dose of reserpine in antihypertensive treatment is as low as 0.05 to 0.25 mg. The use of reserpine as an antipsychotic drug had been nearly completely abandoned, but more recently it made a comeback as adjunctive treatment, in combination with other antipsychotics, so that more refractory patients get dopamine blockade from the other antipsychotic, and dopamine depletion from reserpine. Doses for this kind of adjunctive goal can be kept low, resulting in better tolerability. Originally, doses of 0.5 mg to 40 mg daily were used to treat psychotic diseases.
Doses in excess of 3 mg daily often required use of an anticholinergic drug to combat excessive cholinergic activity in many parts of the body as well as parkinsonism. For adjunctive treatment, doses are typically kept at or below 0.25 mg twice a day.
Veterinary
Reserpine is used as a long-acting tranquilizer to subdue excitable or difficult horses and has been used illicitly for the sedation of show horses, for-sale horses, and in other circumstances where a "quieter" horse might be desired.[29]
Antibacterial Effects
Reserpine inhibits formation of biofilms by Staphylococcus aureus and inhibits the metabolic activity of bacteria present in biofilms.[30]
Adverse effects
At doses of less than 0.2 mg/day, reserpine has few adverse effects, the most common of which is nasal congestion.[31]
Reserpine can cause: nasal congestion, nausea, vomiting, weight gain, gastric intolerance, gastric ulceration (due to increased cholinergic activity in gastric tissue and impaired mucosal quality), stomach cramps and diarrhea are noted. The drug causes hypotension and bradycardia and may worsen asthma. Congested nose and erectile dysfunction are other consequences of alpha-blockade.[32]
Central nervous system effects at higher doses (0.5 mg or higher) include drowsiness, dizziness, nightmares, Parkinsonism, general weakness and fatigue. [33]
High dose studies in rodents found reserpine to cause fibroadenoma of the breast and malignant tumors of the seminal vesicles among others. Early suggestions that reserpine causes breast cancer in women (risk approximately doubled) were not confirmed. It may also cause hyperprolactinemia.[32]
Reserpine passes into breast milk and is harmful to breast-fed infants, and should therefore be avoided during breastfeeding if possible.[34]
It may produce an excessive decline in blood pressure at doses needed for treatment of anxiety, depression, or psychosis.[35]
References
- Tsioufis C, Thomopoulos C (November 2017). "Combination drug treatment in hypertension". Pharmacol. Res. 125 (Pt B): 266–271. doi:10.1016/j.phrs.2017.09.011. PMID 28939201.
- http://drugcentral.org/drugcard/2370
- Barzilay J, Grimm R, Cushman W, Bertoni AG, Basile J (August 2007). "Getting to goal blood pressure: why reserpine deserves a second look". J Clin Hypertens (Greenwich). 9 (8): 591–4. doi:10.1111/j.1524-6175.2007.07229.x. PMID 17673879.
- Wang B, Choudhry NK, Gagne JJ, Landon J, Kesselheim AS (March 2015). "Availability and utilization of cardiovascular fixed-dose combination drugs in the United States". Am. Heart J. 169 (3): 379–386.e1. doi:10.1016/j.ahj.2014.12.014. PMID 25728728.
- Forney, Barbara. Reserpine for Veterinary Use Wedgewood Pharmacy. 2001-2002.
- Morley JE (May 2014). "Treatment of hypertension in older persons: what is the evidence?". Drugs Aging. 31 (5): 331–7. doi:10.1007/s40266-014-0171-7. PMID 24668034.
- Hoenders HJ, Bartels-Velthuis AA, Vollbehr NK, Bruggeman R, Knegtering H, de Jong JT (February 2018). "Natural Medicines for Psychotic Disorders: A Systematic Review". J. Nerv. Ment. Dis. 206 (2): 81–101. doi:10.1097/NMD.0000000000000782. PMC 5794244. PMID 29373456.
- Nur S, Adams CE (April 2016). "Chlorpromazine versus reserpine for schizophrenia". Cochrane Database Syst Rev. 4: CD012122. doi:10.1002/14651858.CD012122.pub2. PMID 27124109.
- Yaffe D, Forrest LR, Schuldiner S (May 2018). "The ins and outs of vesicular monoamine transporters". J. Gen. Physiol. 150 (5): 671–682. doi:10.1085/jgp.201711980. PMC 5940252. PMID 29666153.
- Eiden, LE; Weihe, E (2011). "VMAT2: a dynamic regulator of brain monoaminergic neuronal function interacting with drugs of abuse". Ann. N. Y. Acad. Sci. 1216: 86–98. doi:10.1111/j.1749-6632.2010.05906.x. PMC 4183197. PMID 21272013.
- "Indole Alkaloids" Major Types Of Chemical Compounds In Plants & Animals Part II: Phenolic Compounds, Glycosides & Alkaloids. Wayne's Word: An On-Line Textbook of Natural History. 2005.
- Ramawat et al, 1999.Ramawat KG; Rachnana Sharma; Suri SS (2007-01-01). Ramawat, KG.; Merillon, JM. (eds.). Medicinal Plants in Biotechnology- Secondary metabolites 2nd edition 2007. Oxford and IBH, India. pp. 66–367. ISBN 978-1-57808-428-9.
- Rauwolfia Dorlands Medical Dictionary. Merck Source. 2002.
- The Columbia Encyclopedia, Sixth Edition. Copyright © 2001-05 Columbia University Press.
- Pills for Mental Illness?, TIME Magazine, November 8, 1954
- Nicolaou, K. C.; E. J. Sorensen (1996). Classics in Total Synthesis. Weinheim, Germany: VCH. p. 55. ISBN 978-3-527-29284-4.
- López-Muñoz F, Bhatara VS, Alamo C, Cuenca E (2004). "[Historical approach to reserpine discovery and its introduction in psychiatry]". Actas Esp Psiquiatr. 32 (6): 387–95. PMID 15529229.
- Everett GM, Toman JEP (1959) Mode of action of Rauwolfia alkaloids and motor activity. Biol Psychiat 2:75–81
- Baumeister, A. A.; Hawkins, M. F.; Uzelac, S. M. (2003). "The Myth of Reserpine-Induced Depression: Role in the Historical Development of the Monoamine Hypothesis". Journal of the History of the Neurosciences. 12 (2): 207–220. doi:10.1076/jhin.12.2.207.15535. PMID 12953623.
- Davies D. L.; Shepherd M. (1955). "Reserpine in the Treatment of Anxious and Depressed Patients". The Lancet. 269 (6881): 117–20. doi:10.1016/s0140-6736(55)92118-8.
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Narva AS, Ortiz E (February 2014). "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- Shamon SD, Perez MI (December 2016). "Blood pressure-lowering efficacy of reserpine for primary hypertension". Cochrane Database Syst Rev. 12: CD007655. doi:10.1002/14651858.CD007655.pub3. PMC 6464022. PMID 27997978.
- "Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. Hypertension Detection and Follow-up Program Cooperative Group". JAMA. 242 (23): 2562–71. 1979. doi:10.1001/jama.242.23.2562. PMID 490882. full text at OVID
- "Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg". JAMA. 202 (11): 1028–34. 1967. doi:10.1001/jama.202.11.1028. PMID 4862069.
- "Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group". JAMA. 265 (24): 3255–64. 1991. doi:10.1001/jama.265.24.3255. PMID 2046107.
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group (December 18, 2002). "Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)". JAMA. 288 (23): 2981–97. doi:10.1001/jama.288.23.2981. PMID 12479763. Archived from the original on November 26, 2009.
- Shen, Howard (2008). Illustrated Pharmacology Memory Cards: PharMnemonics. Minireview. p. 11. ISBN 978-1-59541-101-3.
- Bhomraj Thanvi, Nelson Lo, and Tom Robinson: Levodopa‐induced dyskinesia in Parkinson's disease: clinical features, pathogenesis, prevention and treatment.Postgrad Med J. 2007 Jun; 83(980): 384–388. PMC 2600052.
- Forney B. Reserpine for veterinary use. Available at http://www.wedgewoodpetrx.com/learning-center/professional-monographs/reserpine-for-veterinary-use.html.
- Parai D, Banerjee M, Dey P, Mukherjee SK (October 2019). "Reserpine attenuates biofilm formation and virulence of Staphylococcus aureus". Microb. Pathog. 138: 103790. doi:10.1016/j.micpath.2019.103790. PMID 31605761.
- Curb JD, Schneider K, Taylor JO, Maxwell M, Shulman N (1988). "Antihypertensive drug side effects in the Hypertension Detection and Follow-up Program". Hypertension. 11 (3 Pt 2): II51–5. doi:10.1161/01.hyp.11.3_pt_2.ii51. PMID 3350594.
- AJ Giannini, HR Black. Psychiatric, Psychogenic, and Somatopsychic Disorders Handbook. Garden City, NY. Medical Examination Publishing, 1978. Pg. 233. ISBN 0-87488-596-5.
- Barcelos, R. C. S.; Benvegnú, D. M.; Boufleur, N.; Pase, C.; Teixeira, A. L. M.; Reckziegel, P. C.; Emanuelli, T.; Da Rocha, J. O. B. T.; Bürger, M. E. (2010). "Short Term Dietary Fish Oil Supplementation Improves Motor Deficiencies Related to Reserpine-Induced Parkinsonism in Rats". Lipids. 46 (2): 143–149. doi:10.1007/s11745-010-3514-0. PMID 21161603.
- kidsgrowth.org --> Drugs and Other Substances in Breast Milk Archived 2007-06-23 at Archive.today Retrieved on June 19, 2009
- Pinel, John P.J. (2011). Biopsychology (8th ed.). Boston: Allyn & Bacon. p. 469. ISBN 978-0205832569.
External links
- NLM Hazardous Substances Databank – Reserpine
- PubChem Substance Summary: Reserpine National Center for Biotechnology Information.
- The Stork Synthesis of (−)-Reserpine