Synthetic lethality
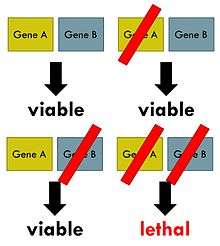
Synthetic lethality arises when a combination of deficiencies in the expression of two or more genes leads to cell death, whereas a deficiency in only one of these genes does not. The deficiencies can arise through mutations, epigenetic alterations or inhibitors of one of the genes. In a synthetic lethal genetic screen, it is necessary to begin with a mutation that does not kill the cell, although may confer a phenotype (for example, slow growth), and then systematically test other mutations at additional loci to determine which confer lethality. Synthetic lethality has utility for purposes of molecular targeted cancer therapy, with the first example of a molecular targeted therapeutic exploiting a synthetic lethal exposed by an inactivated tumor suppressor gene (BRCA1 and 2) receiving FDA approval in 2016 (PARP inhibitor).[1] A sub-case of synthetic lethality, where vulnerabilities are exposed by the deletion of passenger genes rather than tumor suppressor is the so-called "collateral lethality".[2]
Background
The phenomenon of synthetic lethality was first described by Calvin Bridges in 1922, who noticed that some combinations of mutations in the model organism Drosophila melanogaster confer lethality.[3] Theodore Dobzhansky coined the term "synthetic lethality" in 1946 to describe the same type of genetic interaction in wildtype populations of Drosophila.[4] If the combination of genetic events results in a non-lethal reduction in fitness, the interaction is called synthetic sickness. Although in classical genetics the term synthetic lethality refers to the interaction between two genetic perturbations, synthetic lethality can also apply to cases in which the combination of a mutation and the action of a chemical compound causes lethality, whereas the mutation or compound alone are non-lethal.[5]
Synthetic lethality is a consequence of the tendency of organisms to maintain buffering schemes that allow phenotypic stability despite genetic variation, environmental changes and random events such as mutations. This genetic robustness is the result of parallel redundant pathways and "capacitor" proteins that camouflage the effects of mutations so that important cellular processes do not depend on any individual component.[6] Synthetic lethality can help identify these buffering relationships, and what type of disease or malfunction that may occur when these relationships break down, through the identification of gene interactions that function in either the same biochemical process or pathways that appear to be unrelated.[7]
High-throughput screens
High-throughput synthetic lethal screens may help illuminate questions about how cellular processes work without previous knowledge of gene function or interaction. Screening strategy must take into account the organism used for screening, the mode of genetic perturbation, and whether the screen is forward or reverse. Many of the first synthetic lethal screens were performed in S. cerevisiae. Budding yeast has many experimental advantages in screens, including a small genome, fast doubling time, both haploid and diploid states, and ease of genetic manipulation.[8] Gene ablation can be performed using a PCR-based strategy and complete libraries of knockout collections for all annotated yeast genes are publicly available. Synthetic genetic array (SGA), synthetic lethality by microarray (SLAM), and genetic interaction mapping (GIM) are three high-throughput methods for analyzing synthetic lethality in yeast. A genome scale genetic interaction map was created by SGA analysis in S. cerevisiae that comprises about 75% of all yeast genes.[9]
Collateral lethality
Collateral lethality is a sub-case of synthetic lethality in personalized cancer therapy, where vulnerabilities are exposed by the deletion of passenger genes rather than tumor suppressor genes, which are deleted by virtue of chromosomal proximity to major deleted tumor suppressor loci.[2]
DDR deficiencies
DNA mismatch repair deficiency
Mutations in genes employed in DNA mismatch repair (MMR) cause a high mutation rate.[10][11] In tumors, such frequent subsequent mutations often generate "non-self" immunogenic antigens. A human Phase II clinical trial, with 41 patients, evaluated one synthetic lethal approach for tumors with or without MMR defects.[12] In the case of sporadic tumors evaluated, the majority would be deficient in MMR due to epigenetic repression of an MMR gene (see DNA mismatch repair). The product of gene PD-1 ordinarily represses cytotoxic immune responses. Inhibition of this gene allows a greater immune response. In this Phase II clinical trial with 47 patients, when cancer patients with a defect in MMR in their tumors were exposed to an inhibitor of PD-1, 67% - 78% of patients experienced immune-related progression-free survival. In contrast, for patients without defective MMR, addition of PD-1 inhibitor generated only 11% of patients with immune-related progression-free survival. Thus inhibition of PD-1 is primarily synthetically lethal with MMR defects.
Werner syndrome gene deficiency
The analysis of 630 human primary tumors in 11 tissues shows that WRN promoter hypermethylation (with loss of expression of WRN protein) is a common event in tumorigenesis.[13] The WRN gene promoter is hypermethylated in about 38% of colorectal cancers and non-small-cell lung carcinomas and in about 20% or so of stomach cancers, prostate cancers, breast cancers, non-Hodgkin lymphomas and chondrosarcomas, plus at significant levels in the other cancers evaluated. The WRN helicase protein is important in homologous recombinational DNA repair and also has roles in non-homologous end joining DNA repair and base excision DNA repair.[14]
Topoisomerase inhibitors are frequently used as chemotherapy for different cancers, though they cause bone marrow suppression, are cardiotoxic and have variable effectiveness.[15] A 2006 retrospective study, with long clinical follow-up, was made of colon cancer patients treated with the topoisomerase inhibitor irinotecan. In this study, 45 patients had hypermethylated WRN gene promoters and 43 patients had unmethylated WRN gene promoters.[13] Irinitecan was more strongly beneficial for patients with hypermethylated WRN promoters (39.4 months survival) than for those with unmethylated WRN promoters (20.7 months survival). Thus, a topoisomerase inhibitor appeared to be synthetically lethal with deficient expression of WRN. Further evaluations have also indicated synthetic lethality of deficient expression of WRN and topoisomerase inhibitors.[16][17][18][19][20]
Clinical and preclinical PARP1 inhibitor synthetic lethality
As reviewed by Murata et al.,[21] five different PARP1 inhibitors are now undergoing Phase I, II and III clinical trials, to determine if particular PARP1 inhibitors are synthetically lethal in a large variety of cancers, including those in the prostate, pancreas, non-small-cell lung tumors, lymphoma, multiple myeloma, and Ewing sarcoma. In addition, in preclinical studies using cells in culture or within mice, PARP1 inhibitors are being tested for synthetic lethality against epigenetic and mutational deficiencies in about 20 DNA repair defects beyond BRCA1/2 deficiencies. These include deficiencies in PALB2, FANCD2, RAD51, ATM, MRE11, p53, XRCC1 and LSD1.
Preclinical ARID1A synthetic lethality
ARID1A, a chromatin modifier, is required for non-homologous end joining, a major pathway that repairs double-strand breaks in DNA,[22] and also has transcription regulatory roles.[23] ARID1A mutations are one of the 12 most common carcinogenic mutations.[24] Mutation or epigenetically decreased expression[25] of ARID1A has been found in 17 types of cancer.[26] Pre-clinical studies in cells and in mice show that synthetic lethality for deficient ARID1A expression occurs by either inhibition of the methyltransferase activity of EZH2,[27][28] by inhibition of the DNA repair kinase ATR,[29] or by exposure to the kinase inhibitor dasatinib.[30]
Preclinical RAD52 synthetic lethality
There are two pathways for homologous recombinational repair of double-strand breaks. The major pathway depends on BRCA1, PALB2 and BRCA2 while an alternative pathway depends on RAD52.[31] Pre-clinical studies, involving epigenetically reduced or mutated BRCA-deficient cells (in culture or injected into mice), show that inhibition of RAD52 is synthetically lethal with BRCA-deficiency.[32]
Side effects
Although treatments using synthetic lethality can stop or slow progression of cancers and prolong survival, each of the synthetic lethal treatments has some adverse side effects. For example, more than 20% of patients treated with an inhibitor of PD-1 encounter fatigue, rash, pruritus, cough, diarrhea, decreased appetite, constipation or arthralgia.[33] Thus, it is important to determine which DDR deficiency is present, so that only an effective synthetic lethal treatment can be applied, and not unnecessarily subject patients to adverse side effects without a direct benefit.
See also
References
- Lord, Christopher J.; Ashworth, Alan (17 March 2017). "PARP inhibitors: Synthetic lethality in the clinic". Science. 355 (6330): 1152–1158. Bibcode:2017Sci...355.1152L. doi:10.1126/science.aam7344. ISSN 1095-9203. PMC 6175050. PMID 28302823.
- Muller, Florian (August 16, 2012). "Passenger deletions generate therapeutic vulnerabilities in cancer". Nature. 488 (7411): 337–342. Bibcode:2012Natur.488..337M. doi:10.1038/nature11331. PMC 3712624. PMID 22895339.
- Nijman, Sebastian (Jan 3, 2011). "Synthetic Lethality: General principles, utility and detection using genetic screens in human cells". FEBS Lett. 585 (1): 1–6. doi:10.1016/j.febslet.2010.11.024. PMC 3018572. PMID 21094158.
- Ferrari, Elisa; Lucca, Chiara; Foiani, Marco (Nov 2010). "A lethal combination for cancer cells: synthetic lethality screenings for drug discovery". Eur J Cancer. 46 (16): 2889–95. doi:10.1016/j.ejca.2010.07.031. PMID 20724143.
- Hartwell, LH (Nov 7, 1997). "Integrating genetic approaches into the discovery of anticancer drugs". Science. 278 (5340): 1064–1068. Bibcode:1997Sci...278.1064H. doi:10.1126/science.278.5340.1064. PMID 9353181.
- Baugh, LR (2005). "Synthetic lethal analysis of Caenorhabditis elegans posterior embryonic patterning genes identifies conserved genetic interactions". Genome Biol. 6 (5): R45. doi:10.1186/gb-2005-6-5-r45. PMC 1175957. PMID 15892873.
- Hartman; Garvik, B; Hartwell, L (Feb 2001). "Principles for the buffering of genetic variation". Science. 291 (5506): 1001–4. Bibcode:2001Sci...291.1001H. doi:10.1126/science.291.5506.1001. PMID 11232561.
- Matuo, Renata; Sousa, Fabricio; Soares, Daniele; Bonatto, Diego; Saffi, Jenifer; Escargueil, Alexandre; Larsen, Annette; Henriques, Joao (Oct 2012). "Saccharomyces cerevisiae as a model system to study the response to anticancer agents". Cancer Chemother Pharmacol. 70 (4): 491–502. doi:10.1007/s00280-012-1937-4. PMID 22851206.
- Costanzo, Michael (Jan 2010). "The Genetic Landscape of a Cell". Science. 327 (5964): 425–431. Bibcode:2010Sci...327..425C. doi:10.1126/science.1180823. PMC 5600254. PMID 20093466.
- Narayanan, L.; Fritzell, J. A.; Baker, S. M.; Liskay, R. M.; Glazer, P. M. (1997). "Elevated levels of mutation in multiple tissues of mice deficient in the DNA mismatch repair gene Pms2". Proceedings of the National Academy of Sciences. 94 (7): 3122–3127. Bibcode:1997PNAS...94.3122N. doi:10.1073/pnas.94.7.3122. PMC 20332. PMID 9096356.
- Hegan, D. C.; Narayanan, L.; Jirik, F. R.; Edelmann, W.; Liskay, R.M.; Glazer, P. M. (2006). "Differing patterns of genetic instability in mice deficient in the mismatch repair genes Pms2, Mlh1, Msh2, Msh3 and Msh6". Carcinogenesis. 27 (12): 2402–2408. doi:10.1093/carcin/bgl079. PMC 2612936. PMID 16728433.
- Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, Biedrzycki B, Donehower RC, Zaheer A, Fisher GA, Crocenzi TS, Lee JJ, Duffy SM, Goldberg RM, de la Chapelle A, Koshiji M, Bhaijee F, Huebner T, Hruban RH, Wood LD, Cuka N, Pardoll DM, Papadopoulos N, Kinzler KW, Zhou S, Cornish TC, Taube JM, Anders RA, Eshleman JR, Vogelstein B, Diaz LA (2015). "PD-1 Blockade in Tumors with Mismatch-Repair Deficiency". N. Engl. J. Med. 372 (26): 2509–20. doi:10.1056/NEJMoa1500596. PMC 4481136. PMID 26028255.
- Agrelo R, Cheng WH, Setien F, Ropero S, Espada J, Fraga MF, Herranz M, Paz MF, Sanchez-Cespedes M, Artiga MJ, Guerrero D, Castells A, von Kobbe C, Bohr VA, Esteller M (2006). "Epigenetic inactivation of the premature aging Werner syndrome gene in human cancer". Proc. Natl. Acad. Sci. U.S.A. 103 (23): 8822–7. Bibcode:2006PNAS..103.8822A. doi:10.1073/pnas.0600645103. PMC 1466544. PMID 16723399.
- Monnat RJ (2010). "Human RECQ helicases: roles in DNA metabolism, mutagenesis and cancer biology". Semin. Cancer Biol. 20 (5): 329–39. doi:10.1016/j.semcancer.2010.10.002. PMC 3040982. PMID 20934517.
- Pommier Y (2013). "Drugging topoisomerases: lessons and challenges". ACS Chem. Biol. 8 (1): 82–95. doi:10.1021/cb300648v. PMC 3549721. PMID 23259582.
- Wang L, Xie L, Wang J, Shen J, Liu B (2013). "Correlation between the methylation of SULF2 and WRN promoter and the irinotecan chemosensitivity in gastric cancer". BMC Gastroenterol. 13: 173. doi:10.1186/1471-230X-13-173. PMC 3877991. PMID 24359226.
- Bird JL, Jennert-Burston KC, Bachler MA, Mason PA, Lowe JE, Heo SJ, Campisi J, Faragher RG, Cox LS (2012). "Recapitulation of Werner syndrome sensitivity to camptothecin by limited knockdown of the WRN helicase/exonuclease". Biogerontology. 13 (1): 49–62. doi:10.1007/s10522-011-9341-8. PMID 21786128.
- Masuda K, Banno K, Yanokura M, Tsuji K, Kobayashi Y, Kisu I, Ueki A, Yamagami W, Nomura H, Tominaga E, Susumu N, Aoki D (2012). "Association of epigenetic inactivation of the WRN gene with anticancer drug sensitivity in cervical cancer cells". Oncol. Rep. 28 (4): 1146–52. doi:10.3892/or.2012.1912. PMC 3583574. PMID 22797812.
- Futami K, Takagi M, Shimamoto A, Sugimoto M, Furuichi Y (2007). "Increased chemotherapeutic activity of camptothecin in cancer cells by siRNA-induced silencing of WRN helicase". Biol. Pharm. Bull. 30 (10): 1958–61. doi:10.1248/bpb.30.1958. PMID 17917271.
- Futami K, Ishikawa Y, Goto M, Furuichi Y, Sugimoto M (2008). "Role of Werner syndrome gene product helicase in carcinogenesis and in resistance to genotoxins by cancer cells". Cancer Sci. 99 (5): 843–8. doi:10.1111/j.1349-7006.2008.00778.x. PMID 18312465.
- Murata S, Zhang C, Finch N, Zhang K, Campo L, Breuer EK (2016). "Predictors and Modulators of Synthetic Lethality: An Update on PARP Inhibitors and Personalized Medicine". Biomed Res Int. 2016: 1–12. doi:10.1155/2016/2346585. PMC 5013223. PMID 27642590.
- Watanabe R, Ui A, Kanno S, Ogiwara H, Nagase T, Kohno T, Yasui A (2014). "SWI/SNF factors required for cellular resistance to DNA damage include ARID1A and ARID1B and show interdependent protein stability". Cancer Res. 74 (9): 2465–75. doi:10.1158/0008-5472.CAN-13-3608. PMID 24788099.
- Raab JR, Resnick S, Magnuson T (2015). "Genome-Wide Transcriptional Regulation Mediated by Biochemically Distinct SWI/SNF Complexes". PLoS Genet. 11 (12): e1005748. doi:10.1371/journal.pgen.1005748. PMC 4699898. PMID 26716708.
- Lawrence MS, Stojanov P, Mermel CH, Robinson JT, Garraway LA, Golub TR, Meyerson M, Gabriel SB, Lander ES, Getz G (2014). "Discovery and saturation analysis of cancer genes across 21 tumour types". Nature. 505 (7484): 495–501. Bibcode:2014Natur.505..495L. doi:10.1038/nature12912. PMC 4048962. PMID 24390350.
- Zhang X, Sun Q, Shan M, Niu M, Liu T, Xia B, Liang X, Wei W, Sun S, Zhang Y, Liu XS, Song Q, Yang Y, Ma Y, Liu Y, Yang L, Ren Y, Zhang G, Pang D (2013). "Promoter hypermethylation of ARID1A gene is responsible for its low mRNA expression in many invasive breast cancers". PLoS ONE. 8 (1): e53931. Bibcode:2013PLoSO...853931Z. doi:10.1371/journal.pone.0053931. PMC 3549982. PMID 23349767.
- Wu JN, Roberts CW (2013). "ARID1A mutations in cancer: another epigenetic tumor suppressor?". Cancer Discov. 3 (1): 35–43. doi:10.1158/2159-8290.CD-12-0361. PMC 3546152. PMID 23208470.
- Bitler BG, Aird KM, Garipov A, Li H, Amatangelo M, Kossenkov AV, Schultz DC, Liu Q, Shih IeM, Conejo-Garcia JR, Speicher DW, Zhang R (2015). "Synthetic lethality by targeting EZH2 methyltransferase activity in ARID1A-mutated cancers". Nat. Med. 21 (3): 231–8. doi:10.1038/nm.3799. PMC 4352133. PMID 25686104.
- Kim KH, Kim W, Howard TP, Vazquez F, Tsherniak A, Wu JN, Wang W, Haswell JR, Walensky LD, Hahn WC, Orkin SH, Roberts CW (2015). "SWI/SNF-mutant cancers depend on catalytic and non-catalytic activity of EZH2". Nat. Med. 21 (12): 1491–6. doi:10.1038/nm.3968. PMC 4886303. PMID 26552009.
- Williamson, Chris T.; Miller, Rowan; Pemberton, Helen N.; Jones, Samuel E.; Campbell, James; Konde, Asha; Badham, Nicholas; Rafiq, Rumana; Brough, Rachel (13 December 2016). "ATR inhibitors as a synthetic lethal therapy for tumours deficient in ARID1A". Nature Communications. 7: 13837. Bibcode:2016NatCo...713837W. doi:10.1038/ncomms13837. ISSN 2041-1723. PMC 5159945. PMID 27958275.
- Miller RE, Brough R, Bajrami I, Williamson CT, McDade S, Campbell J, Kigozi A, Rafiq R, Pemberton H, Natrajan R, Joel J, Astley H, Mahoney C, Moore JD, Torrance C, Gordan JD, Webber JT, Levin RS, Shokat KM, Bandyopadhyay S, Lord CJ, Ashworth A (2016). "Synthetic Lethal Targeting of ARID1A-Mutant Ovarian Clear Cell Tumors with Dasatinib". Mol. Cancer Ther. 15 (7): 1472–84. doi:10.1158/1535-7163.MCT-15-0554. PMID 27364904.
- Lok BH, Carley AC, Tchang B, Powell SN (2013). "RAD52 inactivation is synthetically lethal with deficiencies in BRCA1 and PALB2 in addition to BRCA2 through RAD51-mediated homologous recombination". Oncogene. 32 (30): 3552–8. doi:10.1038/onc.2012.391. PMC 5730454. PMID 22964643.
- Cramer-Morales K, Nieborowska-Skorska M, Scheibner K, Padget M, Irvine DA, Sliwinski T, Haas K, Lee J, Geng H, Roy D, Slupianek A, Rassool FV, Wasik MA, Childers W, Copland M, Müschen M, Civin CI, Skorski T (2013). "Personalized synthetic lethality induced by targeting RAD52 in leukemias identified by gene mutation and expression profile". Blood. 122 (7): 1293–304. doi:10.1182/blood-2013-05-501072. PMC 3744994. PMID 23836560.
- Villadolid J, Amin A (2015). "Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities". Transl Lung Cancer Res. 4 (5): 560–75. doi:10.3978/j.issn.2218-6751.2015.06.06. PMC 4630514. PMID 26629425.
External links
- Data Repository of Yeast Genetic INteractions
- Saccharomyces Genome Deletion Project
- Syn-Lethality Database
| Look up synthetic lethality in Wiktionary, the free dictionary. |