Plasmid-mediated resistance
Plasmid-mediated resistance is the transfer of antibiotic resistance genes which are carried on plasmids. The plasmids can be transferred between bacteria within the same species or between different species via conjugation. Plasmids often carry multiple antibiotic resistance genes, contributing to the spread of multidrug-resistance (MDR). Antibiotic resistance mediated by MDR plasmids severely limits the treatment options for the infections caused by Gram-negative bacteria, especially family Enterobacteriaceae.[1] The global spread of MDR plasmids has been enhanced by selective pressure from antibiotic usage in human and veterinary medicine.[2]
Properties of resistance plasmids
Resistance plasmids by definition carry one or more antibiotic resistance genes. They are frequently accompanied by the genes encoding virulence determinants, specific enzymes or resistance to toxic heavy metals. Multiple resistance genes are commonly arranged in the resistance cassettes. The antibiotic resistance genes found on the plasmids confer resistance to most of the antibiotic classes used nowadays, for example, beta-lactams, fluoroquinolones and aminoglycosides.[1][3]
It is very common for the resistance genes or entire resistance cassettes to be re-arranged on the same plasmid or be moved to a different plasmid or chromosome by means of recombination systems. Examples of such systems include integrons and transposons.[3]
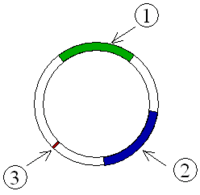
Most of the resistance plasmids are conjugative, meaning that they encode all the needed components for the transfer of the plasmid to other bacterium. Other smaller plasmids (usually < 10 kb in size) can be mobilized by a conjugative plasmid (usually > 30 kb) in order to be transferred.[3]
Enterobacteriaceae

Members of family Enterobacteriaceae, for example, Escherichia coli or Klebsiella pneumoniae pose the biggest threat regarding plasmid-mediated resistance in hospital- and community-acquired infections.[1]
Beta-lactam resistance
Both narrow spectrum beta-lactamases (e.g. penicillinases) and extended spectrum beta-lactamases (ESBL) are common for resistance plasmids in Enterobacteriaceae. Often multiple beta-lactamase genes are found on the same plasmid hydrolyzing a wide spectrum of beta-lactam antibiotics.[1]
Extended spectrum beta-lactamases (ESBL)
ESBL enzymes can hydrolyze all beta-lactam antibiotics, including cephalosporins, except for the carpabepenems. The first clinically observed ESBL enzymes were mutated versions of the narrow spectrum beta-lactamases, like TEM and SHV. Other ESBL enzymes originate outside of family Enterobacteriaceae, but have been spreading as well.[1]
In addition, since the plasmids that carry ESBL genes also commonly encode resistance determinants for many other antibiotics, ESBL strains are often resistant to many non-beta-lactam antibiotics as well,[4] leaving very few options for the treatment.
Carbapenemases
Carbapenemases represent type of ESBL which are able to hydrolyze carbapenem antibiotics that are considered as the last-resort treatment for ESBL-producing bacteria. KPC, NDM-1, VIM and OXA-48 carbapenemases have been increasingly reported worldwide as causes of hospital-acquired infections.[1]
Quinolone resistance
Quinolone resistance genes are frequently located on the same plasmid as the ESBL genes. Examples of resistance mechanisms include different Qnr proteins, aminoglycose acetyltransferase aac(6')-Ib-cr that is able to hydrolyze ciprofloxacin and norfloxacin, as well as efflux transporters OqxAB and QepA.[1]
Aminoglycoside resistance
Aminoglycoside resistance genes are also commonly found together with ESBL genes. Resistance to aminoglycosides is conferred via numerous aminoglycoside-modifying enzymes and 16S rRNA methyltransferases.[1]
small RNAs
Study investigating physiological effect of pHK01 plasmid in host E.coli J53 found that the plasmid reduced bacterial motility and conferred resistance to beta-lactams. The pHK01 produced plasmid-encoded small RNAs and mediated expression of host sRNAs. These sRNAs were antisense to genes involved in replication, conjugate transfer and plasmid stabilisation : AS-repA3 (CopA), AS-traI, AS-finO, AS-traG, AS-pc02 . The over-expression of one of the plasmid-encoded antisense sRNAs: AS-traI shortened t lalog phase of host growth.[5]
References
- Schultsz C, Geerlings S (January 2012). "Plasmid-mediated resistance in Enterobacteriaceae: changing landscape and implications for therapy". Drugs. 72 (1): 1–16. doi:10.2165/11597960-000000000-00000. PMID 22191792.
- Carattoli A (October 2003). "Plasmid-mediated antimicrobial resistance in Salmonella enterica" (PDF). Current Issues in Molecular Biology. 5 (4): 113–22. PMID 12921226.
- Bennett PM (March 2008). "Plasmid encoded antibiotic resistance: acquisition and transfer of antibiotic resistance genes in bacteria". British Journal of Pharmacology. 153 Suppl 1 (S1): S347–57. doi:10.1038/sj.bjp.0707607. PMC 2268074. PMID 18193080.
- Broad spectrum antibiotics and resistance in non-target bacteria: an example from tetracycline, Journal of Pure and Applied Microbiology, (2014); 8(4): 2667-2671.
- Jiang X, Liu X, Law CO, Wang Y, Lo WU, Weng X, Chan TF, Ho PL, Lau TC (July 2017). "The CTX-M-14 plasmid pHK01 encodes novel small RNAs and influences host growth and motility". FEMS Microbiology Ecology. 93 (7). doi:10.1093/femsec/fix090. PMID 28854680.
Further reading
- Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A (October 2009). "Plasmid-mediated quinolone resistance: a multifaceted threat". Clinical Microbiology Reviews. 22 (4): 664–89. doi:10.1128/CMR.00016-09. PMC 2772364. PMID 19822894.
- Nordmann P, Poirel L (September 2005). "Emergence of plasmid-mediated resistance to quinolones in Enterobacteriaceae". The Journal of Antimicrobial Chemotherapy. 56 (3): 463–9. doi:10.1093/jac/dki245. PMID 16020539.
- Oktem IM, Gulay Z, Bicmen M, Gur D (January 2008). "qnrA prevalence in extended-spectrum beta-lactamase-positive Enterobacteriaceae isolates from Turkey". Japanese Journal of Infectious Diseases. 61 (1): 13–7. PMID 18219128. Archived from the original on 6 June 2010.
- Chen LP, Cai XW, Wang XR, Zhou XL, Wu DF, Xu XJ, Chen HC (October 2010). "Characterization of plasmid-mediated lincosamide resistance in a field isolate of Haemophilus parasuis". The Journal of Antimicrobial Chemotherapy. 65 (10): 2256–8. doi:10.1093/jac/dkq304. PMID 20699244.