McKenzie method
The McKenzie method (also Mechanical Diagnosis and Therapy) is a technique primarily used in physical therapy. It was developed in the late 1950s by New Zealand physical therapist Robin McKenzie, OBE (1931–2013).[1][2][3] In 1981 he launched the concept which he called Mechanical Diagnosis and Therapy (MDT) – a system encompassing assessment, diagnosis and treatment for the spine and extremities. MDT categorises patients' complaints not on an anatomical basis,[4][5][6] but subgroups them by the clinical presentation of patients.[7]
| McKenzie method | |
|---|---|
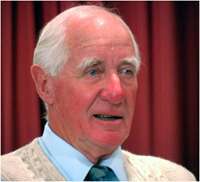 Robin Anthony McKenzie | |
| Other names | Mechanical Diagnosis and Therapy |
There is weak evidence for the effectiveness of the Method's use for treating lower back pain.[8]
Effectiveness
The McKenzie method has been widely used and as of 2019 is recommended in the United Kingdom by National Institute for Health and Care Excellence. However, in general, research into the effectiveness of the McKenzie Method has been of poor quality.[9]
Compared to other treatments, the McKenzie Method is of little benefit for treating acute pain and disability for people with lower back pain. Evidence suggests it may be better than some other approaches for chronic lower back pain, but this evidence is insufficient to inform clinical decision making.[8]
Terminology
The McKenzie method consists of two components used to treat musculoskeletal conditions: assessment and intervention. The assessment component of the McKenzie method uses repeated movements and sustained postures in a single direction to elicit centralisation. In spinal patients centralisation refers to a pattern of pain level response which is characterised by decreased or abolished pain symptoms, experienced sequentially, first to the left and right of the spine (distal symptoms), and ultimately abolished pain symptoms in the spine altogether.[10]
The assessment portion attempts to discover “directional preference”, which identifies the pattern of lumbosacral movement in a single direction that effectively results in centralisation and subsequent abolishment of pain symptoms in the spine and the return of proper range of motion.[11]
The intervention component of the McKenzie method is the corresponding repeated and sustained flexion and extension movements as prescribed by the assessment component.[10]
History
The McKenzie method has its roots in an event in 1956 that led to increased experimentation of certain movement in order to elicit what is now known as the centralisation phenomenon. A patient who was experiencing pain on the right side of his lower back buttock, laid down on McKenzie's treatment table. The patient ended up lying in significant lumbar extension for around five minutes, meaning his back was bending backward because the head of the table had been raised for a previous patient. After ceasing this sustained position in lumbar extension the patient noted the pain on the right side of his body had experienced surprising and significant improvement.[12]
This led McKenzie to continuously experiment with specific movement and movement patterns to treat chronic lower back pain and bring about centralisation of pain symptoms. Over the years of experimentation in McKenzie’s career, he noted patterns of symptom relief in response to prescribed spinal movements and positions and developed a classification system to categorise spinal pain problems. McKenzie went on to write and publish books so people could manage and treat their own back pain, such as “Treat Your Own Back” first published in 1980, with the latest edition being published in 2011.[13]
Description
The McKenzie Method also referred to as Mechanical Diagnosis and Therapy is a method of assessing and treating spinal back pain and related extremity pain most commonly through the use of specific repeated movements and appropriate prevention measures. The method puts an emphasis on self-care after initial clinical visits. There are four major steps when it comes to proper McKenzie method therapy: assessment, classification, treatment, and prevention.[14]
The assessment or evaluation procedure determines the type of movements that result in centralisation and reduction in pain.
MDT uses primarily self-treatment strategies, and minimises manual therapy procedures, with the McKenzie-trained therapist supporting the patient with passive procedures only if an individual self-treatment program is not fully effective.
McKenzie states that self treatment is the best way to achieve a lasting improvement of back pain and neck pain.[15][16][17]
Centralisation
Centralisation occurs when Pain symptoms off-centered from the mid-line of the spine, often diagnosed as sciatica, migrate towards the centre of the mid-line of the spine. This migration of pain symptoms to the centre of the lower back is a sign of progress in the McKenzie method. A patient has found their directional preference once they discover which repeated end-range exercise movements elicit centralisation of pain symptoms. The most common directional preference that result in centralisation is extension of the back. In many cases extension exercises are commonly referred to as McKenzie exercises for this very reason.[12]
According to the McKenzie method, movements and exercises that produce centralisation are very beneficial whereas movements that create pain that wander from the spinal mid-line are extremely detrimental to a patient's specific condition. A 2012 systematic review found that lumbar centralisation was associated with a better recovery prognosis in terms of pain, short- and long-term disability, and the likelihood of undergoing surgery in the following year[18]
Assessment
The first step is understanding a patient's symptoms and how they behave—such as where the patient feels pain and when, how often in a day, to what degree, and in what specific movements or positions does pain intensify or express itself. The patient will be tested and asked by a clinician to perform specific single direction movement, both sustained and repeated. A large differentiator from other physical therapy methods of assessment is the use of repeated movements. A range of single direction movements are used in this phase of the McKenzie method, depending on how pain symptoms behave and change will allow the clinician to categorise the problem to effectively prescribe the proper movements to achieve centralisation and elimination of spinal and sciatic pain.[19]
Classification
There are three primary classifications that result from the assessment portion of the McKenzie method's comprehensive approach; Postural syndrome, dysfunction syndrome, and derangements syndrome with a minority of patients falling into an 'other category. Each classification represents the likely underlying reason of experienced pain symptoms and symptom behaviour. The classification process is very important because it determines if the McKenzie method is an appropriate approach for specific patients and also determines which movement and protocols will most likely lead to centralisation and a cessation or reduction of pain symptoms. Each syndrome corresponds to specific mechanical procedures.[20]
Treatment
Depending on the classification and the nature of the underlying cause of disablement, certain treatment protocols are used. Depending on classification type and directional preference, patients perform specific exercises to end-range. There will be limited mobility and the position will likely cause discomfort, but the patient repeats the exercises one after the other until centralisation occurs, pain symptoms subside, and mobility to end-range increases.[21]
Derangement Syndrome
New evidence suggests that centralization and peripheralization of pain can only occur in the derangement syndrome. It is the most commonly encountered classification.[22] Defined by pain that is experienced due to a disturbance in the joint area resulting in diminished movement in certain directions. Depending on a patient's specific directional preference as discovered in the assessment stage of the McKenzie method, patients are prescribed to use repeated movements in a single direction that cause a gradual reduction in pain and centralisation of pain symptoms. That is, symptoms of pain from the left and right of the middle-lower back become centralised to the centre of the lower back and over time result in lasting reduction of pain symptom intensity.[23]
Dysfunction Syndrome
This type of pain is categorised by mechanical impairments and deformities of impaired tissue within the body such as scar tissue or shortened tissues. To treat this treatment classification the goal is to remodel the impaired tissue by mobilisation exercise
Postural Syndrome
This type of pain is the result of postural deformation. Static holds of improper end-range positions, such as slouching are the cause of postural syndrome. Treatment is more geared towards education and proper posture training rather than repeated exercises as the other syndrome classifications prescribe.[21]
Technique
McKenzie exercises is synonymous with spinal extension exercises, as opposed to William Flexion Exercises which is synonymous to lumbar flexion exercises. Physical Therapist usually prescribe McKenzie exercises for patients with centralization phenomenon with directional preference towards spinal extension.
Spinal extension exercises include, but are not limited to:
- Prone position lying flat (patient lies flat on their stomach)
- Prone position propped on elbows (patient lies flat on their stomach and props themselves onto their elbows with the spine in extension)
- Prone position propped on hands (patient lies flat on their stomach and props themselves onto their hands with elbows in full extension, with the spine in extension)
- Standing lumbar extension (patient stands upright with feet shoulder-width apart, and puts hands on the lower back while extending the spine)
Spinal flexion, rotation, or lateral bending can also perform such exercises.[22]
Prevention
The last portion of treatment is designed to educate patients to ensure proper continuation of appropriate exercises and correct structural positioning day-to-day. Self-care and proper exercise is stressed and encouraged as prevention methods.[21]
Prevalence of use
The McKenzie method was commonly used worldwide in the late 2000s in diagnosis[24] and treatment of low back pain,[25][26][27][28] and peripheral joint complaints.[29][30]
See also
References
- "Robin Anthony McKenzie". Archived from the original on 16 May 2013. Retrieved 15 May 2013.
- McKenzie, Robin; May, Stephen (2006). Cervical and Thoracic Spine: Mechanical Diagnosis and Therapy. Orthopedic Physical Therapy Products. ISBN 978-0-9583647-7-5.
- McKenzie, Robin A.; May, Stephen (2003). The lumbar spine mechanical diagnosis & therapy. Waikanae: Spinal Publications New Zealand. ISBN 978-0-9583647-5-1.
- Young, S; April, C; Laslett, M (2003). "Correlation of clinical examination characteristics with three sources of chronic low back pain". The Spine Journal. 3 (6): 460–5. doi:10.1016/S1529-9430(03)00151-7. PMID 14609690.
- Hancock, M. J.; Maher, C. G.; Latimer, J.; Spindler, M. F.; McAuley, J. H.; Laslett, M.; Bogduk, N. (2007). "Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain". European Spine Journal. 16 (10): 1539–1550. doi:10.1007/s00586-007-0391-1. PMC 2078309. PMID 17566796.
- Kolber, Morey J.; Hanney, William J. (2009). "The dynamic disc model: a systematic review of the literature". Physical Therapy Reviews. 14 (3): 181–19. doi:10.1179/174328809X452827.
- Werneke, Mark W.; Hart, Dennis L. (2004). "Categorizing patients with occupational low back pain by use of the Quebec Task Force Classification system versus pain pattern classification procedures: discriminant and predictive validity". Physical Therapy. 84 (3): 243–54. PMID 14984296. Archived from the original on 10 September 2012.
- Lam OT, Strenger DM, Chan-Fee M, Pham PT, Preuss RA, Robbins SM (June 2018). "Effectiveness of the McKenzie Method of Mechanical Diagnosis and Therapy for Treating Low Back Pain: Literature Review With Meta-analysis". J Orthop Sports Phys Ther. 48 (6): 476–490. doi:10.2519/jospt.2018.7562. PMID 29602304.
- Namnaqani FI, Mashabi AS, Yaseen KM, Alshehri MA (December 2019). "The effectiveness of McKenzie method compared to manual therapy for treating chronic low back pain: a systematic review". J Musculoskelet Neuronal Interact (Systematic review). 19 (4): 492–499. PMC 6944795. PMID 31789300.
- May, Stephen; Donelson, Ronald (2008). "Evidence-informed management of chronic low back pain with the McKenzie method". The Spine Journal. 8 (1): 134–141. doi:10.1016/j.spinee.2007.10.017. PMID 18164461 – via Elsevior.
- Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine 2002;27:E207–14
- McKenzie, Robin (2011). Treat Your Own Back. Spinal Publications New Zealand Ltd. pp. x–xi. ISBN 978-0-9876504-0-5.
- McKenzie RA. The lumbar spine: mechanical diagnosis and therapy. Waikanae, NZ: Spinal Publications New Zealand Ltd., 1981.
- "For Patients - The McKenzie Institute, USA". www.mckenzieinstituteusa.org. Retrieved 2 April 2017.
- Udermann, B; Spratt, KF; Donelson, RG; Mayer, J; Graves, JE; Tillotson, J (2004). "Can a patient educational book change behavior and reduce pain in chronic low back pain patients?". The Spine Journal. 4 (4): 425–35. doi:10.1016/j.spinee.2004.01.016. PMID 15246305.
- May, S; Donelson, R (2008). "Evidence-informed management of chronic low back pain with the McKenzie method". The Spine Journal. 8 (1): 134–41. doi:10.1016/j.spinee.2007.10.017. PMID 18164461.
- May, S; Gardiner, E; Young, S; Klaber-Moffett, J (2008). "Predictor Variables for a Positive Long-Term Outcome in Patients with Acute and Chronic Neck and Back Pain Treated with a McKenzie Approach: A Secondary Analysis". The Journal of Manual & Manipulative Therapy. 16 (3): 155–60. doi:10.1179/jmt.2008.16.3.155. PMC 2582422. PMID 19119405.
- May, S; Aina, A (2012). "Centralization and directional preference: A systematic review". Manual Therapy. 17 (6): 497–506. doi:10.1016/j.math.2012.05.003. PMID 22695365.
- "What does it involve?". The McKenzie Institute International®. Retrieved 2 April 2017.
- "The McKenzie Method". The McKenzie Institute International®. Retrieved 2 April 2017.
- "Mckenzie Method - Physiopedia, universal access to physiotherapy knowledge". www.physio-pedia.com. Retrieved 3 April 2017.
- Mann, Steven J.; Singh, Paramvir (2019), "McKenzie Back Exercises", StatPearls, StatPearls Publishing, PMID 30969542, retrieved 9 December 2019

- "The McKenzie Method". The McKenzie Institute International®. Retrieved 2 April 2017.
- Horton, S; Franz, A (2007). "Mechanical Diagnosis and Therapy approach to assessment and treatment of derangement of the sacro-iliac joint". Manual Therapy. 12 (2): 126–32. doi:10.1016/j.math.2006.06.001. PMID 16891145.
- Spoto, Marcia Miller; Collins, Jennifer (2008). "Physiotherapy diagnosis in clinical practice: a survey of orthopaedic certified specialists in the USA". Physiotherapy Research International. 13 (1): 31–41. doi:10.1002/pri.390. PMID 18189334.
- Miller, Eric R.; Schenk, Ronald J.; Karnes, James L.; Rousselle, John G. (2005). "A Comparison of the McKenzie Approach to a Specific Spine Stabilization Program for Chronic Low Back Pain". Journal of Manual & Manipulative Therapy. 13 (2): 103–12. doi:10.1179/106698105790824996.
- Tulder, Maurits; Becker, Annette; Bekkering, Trudy; Breen, Alan; Gil Del Real, Maria Teresa; Hutchinson, Allen; Koes, Bart; Laerum, Even; et al. (2006). "Chapter 3 European guidelines for the management of acute nonspecific low back pain in primary care". European Spine Journal. 15: S169–91. doi:10.1007/s00586-006-1071-2. PMC 3454540. PMID 16550447.
- Schrupp, Robert J. (June 2004). "Honoring Our 'Giants'". Advance for Physical Therapy & Rehab Medicine. 15 (14): 61. Archived from the original on 7 July 2011. Retrieved 7 December 2010.
- May, Stephen; Ross, Jenny (2009). "The McKenzie Classification System in the Extremities: A Reliability Study Using Mckenzie Assessment Forms and Experienced Clinicians". Journal of Manipulative and Physiological Therapeutics. 32 (7): 556–63. doi:10.1016/j.jmpt.2009.08.007. PMID 19748407.
- McKenzie, Robin (2000). Human Extremities: Mechanical Diagnosis and Therapy. Orthopedic Physical Therapy Products. ISBN 978-0-9583647-0-6.