Interventional neuroradiology
Endovascular Surgical Neuroradiology (ESN), also known as Neurointerventional Surgery (NIS), Interventional Neuroradiology (INR), and Endovascular Neurosurgery, is a medical subspecialty of Neurology, Neurosurgery, and radiology specializing in minimally invasive image-based technologies and procedures used in diagnosis and treatment of diseases of the head, neck, and spine.[1]
History
Diagnostic angiography
Cerebral angiography was developed by Portuguese neurologist Egas Moniz at the University of Lisbon, in order to identify central nervous system diseases such as tumors or arteriovenous malformations. He performed the first brain angiography in Lisbon in 1927[3] by injecting an iodinated contrast medium into the carotid artery and using the X-rays discovered 30 years earlier by Roentgen in order to visualize the cerebral vessels. In pre-CT and pre-MRI, it was the only tool to observe the structures within the skull and was also used to diagnose extravascular pathologies.
Subsequently, European radiologists further developed the angiographic technique by replacing the traumatic direct puncture with catheterization: in 1953, Swedish physician Sven Seldinger introduced the technique of arterial and venous catheterization still in practice. In 1964, the Norwegian radiologist Per Amudsen was the first to perform a complete brain angiography with a transfemoral approach, as it is performed today; he then moved to San Francisco to teach the technique to American neuroradiologists. These two stages, at the basis of modern invasive vascular diagnostics, prepared the way for later therapeutic developments.
The first treatments: balloon occlusion
The first to carry out a true endovascular procedure was Charles Dotter, the father of angioplasty and considered by many as the father of all interventional radiology, as well as the first doctor to have performed endovascular treatment. On January 16, 1964, he performed a therapeutic angioplasty of a superficial femoral artery in an 82-year-old woman with an ischemic leg refusing amputation.[4] The artery remained open for the next 2 and a half years, after which the woman died of pneumonia.
The concept of using balloons to treat cerebrovascular lesions was inspired by a 1959 May Day celebration in Moscow’s Red Square. While watching children use tether lines to manipulate helium balloons, Fedor Serbinenko, a Russian neurosurgeon, began to envision small balloons moving through tortuous arteries.[5] In the 1970s Fedor Serbinenko developed a technique for closing aneurysms with balloons that were released into the internal carotid artery by occluding the lumen. The first treatment was performed in 1970 in Moscow, with the occlusion of an internal carotid to treat a carotid-cavernous fistula. He can be considered, therefore, the first interventional neuroradiologist. This technique was subsequently refined by neuroradiologists all over the world and mainly in France, where interventional neuroradiology developed and flourished.
Parallel to the development of catheters, in the radiology and neuroradiology units, image technology dramatically improved: Charles Mistretta in 1979 invented digital subtraction angiography (DSA), the technique currently in use. It consists of performing skull radiography under basic conditions which are then "subtracted" to the image after contrast media injection, to provide an image where only brain vessels are displayed, with great improvement in the diagnostic potential.
Coils replace balloon occlusion
Between the end of the '80s and the beginning of the '90s, INR was suddenly revolutionized after the work of two Italian physicians: Cesare Gianturco and Guido Guglielmi. The first combined a deep knowledge of diagnostic radiology with a great ability to solve technical and manual problems. He invented Gianturco's coils, which he used to make the first attempts to embolize arteries and aneurysms. Gianturco also patented the first endovascular stent approved by the American FDA; a device with a great legacy. In the second half of the 1980s, Hilal was the first in Columbia University to use coils to treat brain aneurysms; but this technique was inaccurate and dangerous because the coils were released with little control with great risk of occluding the vessel from which the aneurysm originated (parent vessel). The coil embolization was revolutionized by the work of Guido Guglielmi in UCLA, who realized that electricity could function as a controlled release mechanism for coils; in 1991 he published two works dealing with the embolization of brain aneurysms by means of detachable platinum coils (Guglielmi's coils). The treatment of aneurysms was thus made more accessible and safe.
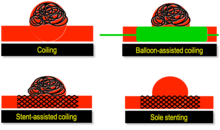
New techniques: Sole stenting and flow diversion stents
From the early 2000s, intracranial stents were used to prevent the coils inside the aneurysmal sac from protruding into the lumen. Flow diversion devices were later developed, with the function of reconstructing the vessel's normal anatomy without directly closing the aneurysm neck and therefore preserving side branches (in the brain the placement of stents covered is highly unlikely for the risk of closing small side branches and cause ischemia). The sole stenting [6] procedure involves the insertion of a stent only (without any coils) into the vessel that has an aneurysm.[7]
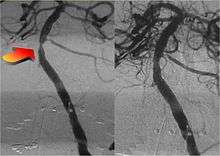
Not just hemorrhages: the treatment of ischemic stroke
Between January and June 2015, 5 major randomized trials were published in the New England Journal of Medicine with the collaboration of interventional neuroradiologists and stroke neurologists (in the Netherlands, Canada, Australia, USA and Spain) regarding the role of mechanical thrombectomy in the treatment of ischemic stroke, demonstrating that if it is performed in centers with proven experience, intra-arterial mechanical thrombectomy is more effective than traditional treatment (intravenous thrombolytic injection).
Thrombectomy is currently recommended by the guidelines written by the main American (AHA/ASA) [8] and European (ESO-ESNR-ESMINT) [9] societies of stroke neurologists and interventional neuroradiologists.
Diseases and conditions

The following is a list of diseases and conditions typically treated by neurointerventionalists.
- Cerebral aneurysm
- Brain arteriovenous malformation (AVM)
- Carotid-cavernous fistula (CCF)
- Dural arteriovenous fistula
- Extracranial (brachiocephalic) atherosclerosis
- Extracranial (head and neck) and paraspinal vascular malformations
- Head and neck tumors
- Intracranial atherosclerosis
- Juvenile nasopharyngeal tumor
- Meningiomas
- Nosebleeds
- Paragangliomas
- Stroke
- Spinal vascular malformations
- Traumatic vascular lesions
- Vasospasm
- Vertebral body tumors
- Vertebral body compression fractures
References
- https://n.neurology.org/content/70/6/e21
- Zenteno, M (March 2012). "Endovascular approach in the management of intracranial aneurysms. Part 1: basic concepts and devices". Gac Med Mex. 148 (2): 169–79. PMID 22622317.
- Artico, M (2017). "Egas Moniz: 90 Years (1927-2017) from Cerebral Angiography". Front Neuroanat. 11: 81. doi:10.3389/fnana.2017.00081. PMC 5610728. PMID 28974927.
- Busch, U (Mar 2014). "50 years ago: Charles Dotter and the first percutaneous transluminal angioplasty". Rofo (in German). 186 (3): 294–5. doi:10.1055/s-0034-1368886. PMID 24557558.
- Alaraj, A (Feb 2014). "Balloons in endovascular neurosurgery: history and current applications". Neurosurgery. 74 Suppl 1: S163-90. doi:10.1227/NEU.0000000000000220. PMID 24402485.
- Zenteno, M (Feb 2010). "Ten-year follow-up of giant basilar aneurysm treated by sole stenting technique: a case report". J Med Case Rep. 4: 64. doi:10.1186/1752-1947-4-64. PMC 2843709. PMID 20175900.
- Zenteno, MA (Jul 2005). "Sole stenting bypass for the treatment of vertebral artery aneurysms: technical case report". Neurosurgery. 57(1 Suppl) (1 Suppl): E208. doi:10.1227/01.neu.0000163683.64511.24. PMID 15987592.
- American Heart Association, Stroke Council (Mar 2018). "2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association". Stroke. 49 (3): e46–e110. doi:10.1161/str.0000000000000158. PMID 29367334.
- Sacks, D (Apr 2018). "Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke". J Vasc Interv Radiol. 29 (4): 441–453. doi:10.1016/j.jvir.2017.11.026. PMID 29478797.