Intersex
Intersex people are individuals born with any of several variations in sex characteristics including chromosomes, gonads, sex hormones or genitals that, according to the UN Office of the High Commissioner for Human Rights, "do not fit the typical definitions for male or female bodies".[1][2] This range of atypical variation may be physically obvious from birth – babies may have ambiguous reproductive organs, or at the other extreme range it is not obvious and may remain unknown to people all their lives.[3] Intersex people were previously referred to as hermaphrodites or "congenital eunuchs".[4][5] In the 19th and 20th centuries, some members of the medical literary community devised new nomenclature to attempt to classify the characteristics that they had observed. It was the first attempt at creating a taxonomic classification system of intersex conditions. Intersex people were categorized as either having true hermaphroditism, female pseudohermaphroditism, or male pseudohermaphroditism.[6] These terms are no longer used: terms including the word "hermaphrodite" are considered to be misleading, stigmatizing, and scientifically specious in reference to humans.[7] A hermaphrodite is now defined as "an animal or plant having both male and female reproductive organs".[6] In 1917, Richard Goldschmidt created the term intersexuality to refer to a variety of physical sex ambiguities.[6] In clinical settings, the term "disorders of sex development" (DSD) has been used since 2006.[8] This shift has been controversial since the label was introduced.[9][10][11]
| Intersex topics |
|---|
 |
|
Medicine and biology |
|
History and events |

Intersex people face stigmatization and discrimination from birth, or from discovery of an intersex trait, such as from puberty. This may include infanticide, abandonment and the stigmatization of families.[12][13][14] Globally, some intersex infants and children, such as those with ambiguous outer genitalia, are surgically or hormonally altered to create more socially acceptable sex characteristics. However, this is considered controversial, with no firm evidence of favorable outcomes.[15] Such treatments may involve sterilization. Adults, including elite female athletes, have also been subjects of such treatment.[16][17] Increasingly, these issues are considered human rights abuses, with statements from international[18][19] and national human rights and ethics institutions.[20][21] Intersex organizations have also issued statements about human rights violations, including the 2013 Malta declaration of the third International Intersex Forum.[22]
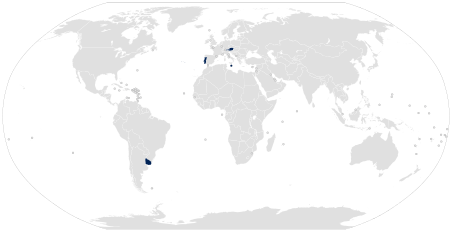
Some intersex persons may be assigned and raised as a girl or boy but then identify with another gender later in life, while most continue to identify with their assigned sex.[23][24] In 2011, Christiane Völling became the first intersex person known to have successfully sued for damages in a case brought for non-consensual surgical intervention.[25] In April 2015, Malta became the first country to outlaw non-consensual medical interventions to modify sex anatomy, including that of intersex people.[26][27]
Definitions

According to the UN Office of the High Commissioner for Human Rights:
Intersex people are born with sex characteristics (including genitals, gonads and chromosome patterns) that do not fit typical binary notions of male or female bodies. Intersex is an umbrella term used to describe a wide range of natural bodily variations. In some cases, intersex traits are visible at birth while in others, they are not apparent until puberty. Some chromosomal intersex variations may not be physically apparent at all.[2]
According to World Health Organization: Intersex is defined as a congenital anomaly of the reproductive and sexual system. An estimate about the birth prevalence of intersex is difficult to make because there are no concrete parameters to the definition of intersex.
In biological terms, sex may be determined by a number of factors present at birth, including:[28]
- the number and type of sex chromosomes,
- the type of gonads—ovaries or testicles,
- sex hormone levels,
- the internal reproductive anatomy (such as the uterus in females), and
- the external genitalia.
People whose characteristics are not either all typically male or all typically female at birth are intersex.[29]
Some intersex traits are not always visible at birth; some babies may be born with ambiguous genitals, while others may have ambiguous internal organs (testes and ovaries). Others will not become aware that they are intersex unless they receive genetic testing, because it does not manifest in their phenotype.
History
_-_02.jpg)
From early history, societies have been aware of Intersex people, some of the earliest evidence is found in mythology. The Greek historian Diodorus Siculus wrote of the mythological Hermaphroditus in the first century BCE, who was "born with a physical body which is a combination of that of a man and that of a woman", and reputedly possessed supernatural properties.[30] Ardhanarishvara, an androgynous composite form of male deity Shiva and female deity Parvati, originated in Kushan culture as far back as the first century CE.[31] A statue depicting Ardhanarishvara is included in India's Meenkashi Temple; this statue clearly shows both male and female bodily elements.[32]
Hippocrates (c. 460 – c. 370 BC Greek physician) and Galen (129 – c.200/216 AD Roman physician, surgeon and philosopher) both viewed sex as a spectrum between men and women, with "many shades in between, including hermaphrodites, a perfect balance of male and female".[33] Pliny the Elder (AD 23/24–79) the Roman naturalist described "those who are born of both sexes, whom we call hermaphrodites, at one time androgyni" (andr-, "man," and gyn-, "woman," from the Greek).[34] Augustine (354 – 28 August 430 AD) the influential catholic theologian wrote in The Literal Meaning of Genesis that humans were created in two sexes, despite "as happens in some births, in the case of what we call androgynes".[33]
In medieval and early modern European societies, Roman law, post-classical canon law, and later common law, referred to a person's sex as male, female or hermaphrodite, with legal rights as male or female depending on the characteristics that appeared most dominant.[35] The 12th-century Decretum Gratiani states that "Whether an hermaphrodite may witness a testament, depends on which sex prevails".[36][37][38] The foundation of common law, the 17th Century Institutes of the Lawes of England described how a hermaphrodite could inherit "either as male or female, according to that kind of sexe which doth prevaile."[39][40] Legal cases have been described in canon law and elsewhere over the centuries.
Some non-European societies have sex or gender systems that recognize more than the two categories of male/man and female/woman. Some of these cultures, for instance the South-Asian Hijra communities, may include intersex people in a third gender category.[41][42] Hawaiian culture in the past and today see intersex individuals as having more power "mana", both mentally and spiritually, than a single sex person. Although–according to Morgan Holmes–early Western anthropologists categorized such cultures "primitive," Holmes has argued that analyses of these cultures have been simplistic or romanticized and fail to take account of the ways that subjects of all categories are treated.[43]
During the Victorian era, medical authors introduced the terms "true hermaphrodite" for an individual who has both ovarian and testicular tissue, "male pseudo-hermaphrodite" for a person with testicular tissue, but either female or ambiguous sexual anatomy, and "female pseudo-hermaphrodite" for a person with ovarian tissue, but either male or ambiguous sexual anatomy. Some later shifts in terminology have reflected advances in genetics, while other shifts are suggested to be due to pejorative associations.[44]
The term intersexuality was coined by Richard Goldschmidt in 1917.[45] The first suggestion to replace the term 'hermaphrodite' with 'intersex' was made by Cawadias in the 1940s.[46]
Since the rise of modern medical science, some intersex people with ambiguous external genitalia have had their genitalia surgically modified to resemble either female or male genitals. Surgeons pinpointed intersex babies as a "social emergency" when born.[47] An 'optimal gender policy', initially developed by John Money, stated that early intervention helped avoid gender identity confusion, but this lacks evidence.[48] Early interventions have adverse consequences for psychological and physical health.[21] Since advances in surgery have made it possible for intersex conditions to be concealed, many people are not aware of how frequently intersex conditions arise in human beings or that they occur at all.[49]
Dialogue between what were once antagonistic groups of activists and clinicians has led to only slight changes in medical policies and how intersex patients and their families are treated in some locations.[50] In 2011, Christiane Völling became the first intersex person known to have successfully sued for damages in a case brought for non-consensual surgical intervention.[25] In April 2015, Malta became the first country to outlaw non-consensual medical interventions to modify sex anatomy, including that of intersex people.[26] Many civil society organizations and human rights institutions now call for an end to unnecessary "normalizing" interventions, including in the Malta declaration.[51][1]
Human rights and legal issues

Human rights institutions are placing increasing scrutiny on harmful practices and issues of discrimination against intersex people. These issues have been addressed by a rapidly increasing number of international institutions including, in 2015, the Council of Europe, the United Nations Office of the United Nations High Commissioner for Human Rights and the World Health Organization. These developments have been accompanied by International Intersex Forums and increased cooperation amongst civil society organizations. However, the implementation, codification, and enforcement of intersex human rights in national legal systems remains slow.
Physical integrity and bodily autonomy
Stigmatization and discrimination from birth may include infanticide, abandonment, and the stigmatization of families. As noted in the "Intersex human rights" page, the birth of an intersex child was often viewed as a curse or a sign of a witch mother, especially in parts of Africa.[12][13] Abandonments and infanticides have been reported in Uganda,[12] Kenya,[52] South Asia,[53] and China.[14]
Infants, children and adolescents also experience "normalising" interventions on intersex persons that are medically unnecessary and the pathologisation of variations in sex characteristics. In countries where the human rights of intersex people have been studied, medical interventions to modify the sex characteristics of intersex people have still taken place without the consent of the intersex person.[54][55] Interventions have been described by human rights defenders as a violation of many rights, including (but not limited to) bodily integrity, non-discrimination, privacy, and experimentation.[56] These interventions have frequently been performed with the consent of the intersex person's parents, when the person is legally too young to consent. Such interventions have been criticized by the World Health Organization, other UN bodies such as the Office of the High Commissioner for Human Rights, and an increasing number of regional and national institutions due to their adverse consequences, including trauma, impact on sexual function and sensation, and violation of rights to physical and mental integrity.[1] The UN organizations decided that infant intervention should not be allowed, in favor of waiting for the child to mature enough to be a part of the decision-making – this allows for a decision to be made with total consent.[57] In April 2015, Malta became the first country to outlaw surgical intervention without consent.[26][27] In the same year, the Council of Europe became the first institution to state that intersex people have the right not to undergo sex affirmation interventions.[26][27][58][59][60]
Anti-discrimination and equal treatment
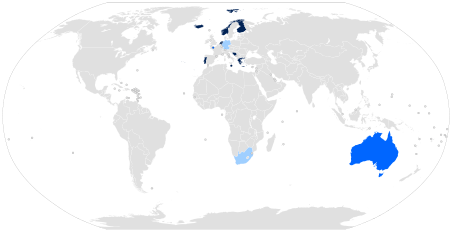
People born with intersex bodies are seen as different. Intersex infants, children, adolescents and adults "are often stigmatized and subjected to multiple human rights violations", including discrimination in education, healthcare, employment, sport, and public services.[2][1][61] Several countries have so far explicitly protected intersex people from discrimination, with landmarks including South Africa,[27][62] Australia,[63][64] and, most comprehensively, Malta.[65][66][67][68][69]
Standing to file in law and compensation claims
Standing to file in law and compensation claims was an issue in the 2011 case of Christiane Völling in Germany.[25][70] A second case was adjudicated in Chile in 2012, involving a child and his parents.[71][72] A further successful case in Germany, taken by Michaela Raab, was reported in 2015.[73] In the United States, the Minor Child (M.C. v Aaronson) lawsuit was "a medical malpractice case related to the informed consent for a surgery performed on the Crawford's adopted child (known as M.C.) at [Medical University of South Carolina] in April 2006".[74] The case was one of the first lawsuit of its kind to challenge "legal, ethical, and medical issues regarding genital-normalizing surgery" in minors, and was eventually settled out of court by the Medical University of South Carolina for $440,000 in 2017.[75]
Information and support
Access to information, medical records, peer and other counselling and support. With the rise of modern medical science in Western societies, a secrecy-based model was also adopted, in the belief that this was necessary to ensure "normal" physical and psychosocial development.[20][21][76][77][78][79]
Legal recognition
The Asia Pacific Forum of National Human Rights Institutions states that legal recognition is firstly "about intersex people who have been issued a male or a female birth certificate being able to enjoy the same legal rights as other men and women."[22] In some regions, obtaining any form of birth certification may be an issue. A Kenyan court case in 2014 established the right of an intersex boy, "Baby A", to a birth certificate.[80]
Like all individuals, some intersex individuals may be raised as a certain sex (male or female) but then identify with another later in life, while most do not.[81][23][82][83] Recognition of third sex or gender classifications occurs in several countries,[84][85][86][87] However, it is controversial when it becomes assumed or coercive, as is the case with some German infants.[88][89] Sociological research in Australia, a country with a third 'X' sex classification, shows that 19% of people born with atypical sex characteristics selected an "X" or "other" option, while 52% are women, 23% men, and 6% unsure.[24][90]
Language


Research in the late 20th century led to a growing medical consensus that diverse intersex bodies are normal, but relatively rare, forms of human biology.[23][91][92][93] Clinician and researcher Milton Diamond stresses the importance of care in the selection of language related to intersex people:
Foremost, we advocate use of the terms "typical", "usual", or "most frequent" where it is more common to use the term "normal." When possible avoid expressions like maldeveloped or undeveloped, errors of development, defective genitals, abnormal, or mistakes of nature. Emphasize that all of these conditions are biologically understandable while they are statistically uncommon.[94]
The term "intersex"
Some people with intersex traits self-identify as intersex, and some do not.[95][96] Australian sociological research published in 2016, found that 60% of respondents used the term "intersex" to self-describe their sex characteristics, including people identifying themselves as intersex, describing themselves as having an intersex variation or, in smaller numbers, having an intersex condition. A majority of 75% of survey respondents also self-described as male or female.[24] Respondents also commonly used diagnostic labels and referred to their sex chromosomes, with word choices depending on audience.[24][90] Research by the Lurie Children's Hospital, Chicago, and the AIS-DSD Support Group published in 2017 found that 80% of affected Support Group respondents "strongly liked, liked or felt neutral about intersex" as a term, while caregivers were less supportive.[97] The hospital reported that "disorders of sex development" may negatively affect care.[98]
Some intersex organizations reference "intersex people" and "intersex variations or traits"[99] while others use more medicalized language such as "people with intersex conditions",[100] or people "with intersex conditions or DSDs (differences of sex development)" and "children born with variations of sex anatomy".[101] In May 2016, Interact Advocates for Intersex Youth published a statement recognizing "increasing general understanding and acceptance of the term "intersex"".[102]
Hermaphrodite
A hermaphrodite is an organism that has both male and female reproductive organs. Until the mid-20th century, "hermaphrodite" was used synonymously with "intersex".[46] The distinctions "male pseudohermaphrodite", "female pseudohermaphrodite" and especially "true hermaphrodite"[103] are terms no longer used, which reflected histology (microscopic appearance) of the gonads.[104][105][106] Medical terminology has shifted not only due to concerns about language, but also a shift to understandings based on genetics.
Currently, hermaphroditism is not to be confused with intersex, as the former refers only to a specific phenotypical presentation of sex organs and the latter to a more complex combination of phenotypical and genotypical presentation. Using hermaphrodite to refer to intersex individuals is considered to be stigmatizing and misleading.[107] Hermaphrodite is used for animal and plant species in which the possession of both ovaries and testes is either serial or concurrent, and for living organisms without such gonads but present binary form of reproduction, which is part of the typical life history of those species; intersex has come to be used when this is not the case.
Disorders of sex development
"Disorders of sex development" (DSD) is a contested term,[9][10] defined to include congenital conditions in which development of chromosomal, gonadal, or anatomical sex is atypical. Members of the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology adopted this term in their "Consensus statement on management of intersex disorders".[8][48] While it adopted the term, to open "many more doors", the now defunct Intersex Society of North America itself remarked that intersex is not a disorder.[108] Other intersex people, activists, supporters, and academics have contested the adoption of the terminology and its implied status as a "disorder", seeing this as offensive to intersex individuals who do not feel that there is something wrong with them, regard the DSD consensus paper as reinforcing the normativity of early surgical interventions, and criticize the treatment protocols associated with the new taxonomy.[109]
Sociological research in Australia, published in 2016, found that 3% of respondents used the term "disorders of sex development" or "DSD" to define their sex characteristics, while 21% use the term when accessing medical services. In contrast, 60% used the term "intersex" in some form to self-describe their sex characteristics.[90] U.S. research by the Lurie Children's Hospital, Chicago, and the AIS-DSD Support Group published in 2017 found that "disorders of sex development" terminology may negatively affect care, give offense, and result in lower attendance at medical clinics.[98][97]
Alternatives to categorizing intersex conditions as "disorders" have been suggested, including "variations of sex development".[11] Organisation Intersex International (OII) questions a disease/disability approach, argues for deferral of intervention unless medically necessary, when fully informed consent of the individual involved is possible, and self-determination of sex/gender orientation and identity.[110] The UK Intersex Association is also highly critical of the label 'disorders' and points to the fact that there was minimal involvement of intersex representatives in the debate which led to the change in terminology.[111] In May 2016, Interact Advocates for Intersex Youth also published a statement opposing pathologizing language to describe people born with intersex traits, recognizing "increasing general understanding and acceptance of the term "intersex"".[102]
LGBT and LGBTI
Intersex can be contrasted with transgender,[112] which is the condition in which one's gender identity does not match one's assigned sex.[112][113][114] Some people are both intersex and transgender.[115] A 2012 clinical review paper found that between 8.5% and 20% of people with intersex variations experienced gender dysphoria.[82] In an analysis of the use of preimplantation genetic diagnosis to eliminate intersex traits, Behrmann and Ravitsky state: "Parental choice against intersex may ... conceal biases against same-sex attractedness and gender nonconformity."[116]
The relationship of intersex to lesbian, gay, bisexual and trans, and queer communities is complex,[117] but intersex people are often added to LGBT to create an LGBTI community. Emi Koyama describes how inclusion of intersex in LGBTI can fail to address intersex-specific human rights issues, including creating false impressions "that intersex people's rights are protected" by laws protecting LGBT people, and failing to acknowledge that many intersex people are not LGBT.[118] Organisation Intersex International Australia states that some intersex individuals are same sex attracted, and some are heterosexual, but "LGBTI activism has fought for the rights of people who fall outside of expected binary sex and gender norms."[119][120] Julius Kaggwa of SIPD Uganda has written that, while the gay community "offers us a place of relative safety, it is also oblivious to our specific needs".[121] Mauro Cabral has written that transgender people and organizations "need to stop approaching intersex issues as if they were trans issues" including use of intersex as a means of explaining being transgender; "we can collaborate a lot with the intersex movement by making it clear how wrong that approach is".[122]
In society

Fiction, literature and media
An intersex character is the narrator in Jeffrey Eugenides' Pulitzer Prize-winning novel Middlesex.
The memoir, Born Both: An Intersex Life (Hachette Books, 2017), by intersex author and activist Hida Viloria, received strong praise from The New York Times Book Review, The Washington Post, Rolling Stone, People Magazine, and Psychology Today, was one of School Library Journal's 2017 Top Ten Adult Books for Teens, and was a 2018 Lambda Literary Award nominee.
Television works about intersex and films about intersex are scarce. The Spanish-language film XXY won the Critics' Week grand prize at the 2007 Cannes Film Festival and the ACID/CCAS Support Award.[123] Faking It is notable for providing both the first intersex main character in a television show,[124] and television's first intersex character played by an intersex actor.[125]
Civil society institutions
Intersex peer support and advocacy organizations have existed since at least 1985, with the establishment of the Androgen Insensitivity Syndrome Support Group Australia in 1985.[126] The Androgen Insensitivity Syndrome Support Group (UK) established in 1988.[127] The Intersex Society of North America (ISNA) may have been one of the first intersex civil society organizations to have been open to people regardless of diagnosis; it was active from 1993 to 2008.[128]
Events
Intersex Awareness Day is an internationally observed civil awareness day designed to highlight the challenges faced by intersex people, occurring annually on 26 October. It marks the first public demonstration by intersex people, which took place in Boston on 26 October 1996, outside a venue where the American Academy of Pediatrics was holding its annual conference.[129]
Intersex Day of Remembrance, also known as Intersex Solidarity Day, is an internationally observed civil awareness day designed to highlight issues faced by intersex people, occurring annually on 8 November. It marks the birthday of Herculine Barbin, a French intersex person whose memoirs were later published by Michel Foucault in Herculine Barbin: Being the Recently Discovered Memoirs of a Nineteenth-century French Hermaphrodite.
Religion
In Hinduism, Sangam literature uses the word pedi to refer to people born with an intersex condition; it also refers to antharlinga hijras and various other hijras.[130] Warne and Raza argue that an association between intersex and hijra people is mostly unfounded but provokes parental fear.[53]
In Judaism, the Talmud contains extensive discussion concerning the status of two intersex types in Jewish law; namely the androgynous, which exhibits both male and female external sexual organs, and the tumtum which exhibits neither. In the 1970s and 1980s, the treatment of intersex babies started to be discussed in Orthodox Jewish medical halacha by prominent rabbinic leaders, for example Eliezer Waldenberg and Moshe Feinstein.[131]
Sport

Erik Schinegger, Foekje Dillema, Maria José Martínez-Patiño and Santhi Soundarajan were subject to adverse sex verification testing resulting in ineligibility to compete in organised competitive competition. Stanisława Walasiewicz was posthumously ruled ineligible to have competed.[132]
The South African middle-distance runner Caster Semenya won gold at the World Championships in the women's 800 metres and won silver in the 2012 Summer Olympics. When Semenya won gold in the World Championships, the International Association of Athletics Federations (IAAF) requested sex verification tests. The results were not released. Semenya was ruled eligible to compete.[133]
Katrina Karkazis, Rebecca Jordan-Young, Georgiann Davis and Silvia Camporesi have claimed that IAAF policies on "hyperandrogenism" in female athletes, are "significantly flawed", arguing that the policy will not protect against breaches of privacy, will require athletes to undergo unnecessary treatment in order to compete, and will intensify "gender policing". They recommend that athletes be able to compete in accordance with their legally recognised gender.[134]
In April 2014, the BMJ reported that four elite women athletes with 5-ARD (an intersex medical condition) were subjected to sterilization and "partial clitoridectomies" in order to compete in sport. The authors noted that partial clitoridectomy was "not medically indicated" and "does not relate to real or perceived athletic 'advantage'."[16] Intersex advocates regard this intervention as "a clearly coercive process".[135] In 2016, the United Nations Special Rapporteur on health, Dainius Pūras, criticized "current and historic" sex verification policies, describing how "a number of athletes have undergone gonadectomy (removal of reproductive organs) and partial clitoridectomy (a form of female genital mutilation) in the absence of symptoms or health issues warranting those procedures."[136]
Population figures

There are few firm estimates of the number of intersex people. The now-defunct Intersex Society of North America stated that:
If you ask experts at medical centers how often a child is born so noticeably atypical in terms of genitalia that a specialist in sex differentiation is called in, the number comes out to about 1 in 1500 to 1 in 2000 births [0.07–0.05%]. But a lot more people than that are born with subtler forms of sex anatomy variations, some of which won't show up until later in life.[137]
Blackless, Fausto-Sterling et al., said in two articles in 2000 that 1.7 percent of human births (1 in 60) might be intersex, including variations that may not become apparent until, for example, puberty, or until attempting to conceive.[138][139] Their publications have been widely quoted,[58][140][141] though aspects are now considered outdated, such as use of the now scientifically incorrect term hermaphrodite.[142] Eric Vilain et al. highlighted in 2007 that the term disorders of sex development (DSD) had replaced "hermaphrodite" and improper medical terms based on it.[143]
The figure of 1.7% is still maintained by Intersex Human Rights Australia "despite its flaws".[144] "This estimate relates to any 'individual who deviates from the Platonic ideal of physical dimorphism at the chromosomal, genital, gonadal, or hormonal levels' and thus it encapsulates the entire population of people who are stigmatized – or risk stigmatization – due to innate sex characteristics."
Individuals with diagnoses of disorders of sex development (DSD) may or may not experience stigma and discrimination due to their sex characteristics, including sex "normalizing" interventions. Human rights institutions have called for the de-medicalization of intersex traits, as far as possible.[20][58][145][146]
The following summarizes some prevalence figures of intersex traits (a fuller 'List of conditions' is provided below, at the end of 'Medical classifications'):
| Intersex Condition | Sex Specificity | Approximate Prevalence |
|---|---|---|
| Late onset congenital adrenal hyperplasia/nonclassic congenital adrenal hyperplasia | female, males are generally asymptomatic[147] | one in 50–1000 births (0.1–0.2% up to 1–2% depending on population)[148] |
| Hypospadias | male | one in 200–10,000 male births (0.01%–0.5%), prevalence estimates vary considerably[149] |
| Klinefelter syndrome | male | one in 500–1,000 male births (0.1–0.2%)[150] |
| 47, XXX genotype | female | one in 1,000 female births (0.10%)[151] |
| Turner syndrome | female | one in 2,500 female births (0.04%)[152] |
| Müllerian agenesis (of vagina, i.e., MRKH Syndrome) | female | one in 4,500 female births (0.022%)[153] |
| Vaginal atresia/agenesis | female | one in 5,000 female births (0.02%)[154] |
| XYY genotype | male | one in 7000 male births (0.0142%)[155] |
| Classic congenital adrenal hyperplasia | none | one in 10,000-20,000 births (0.01%–0.005%)[156] |
| XXYY genotype | male | one in 18,000–40,000 male births (0.0025%–0.0055%)[157] |
| XX genotype (male) | male | one in 20,000 male births (0.005%)[158] |
| Ovotesticular disorder of sex development | none | one in 20,000 births (0.005%)[159] |
| Complete gonadal dysgenesis | phenotypic female[160] | one in 80,000 births (0.0013%)[161] |
| Androgen insensitivity syndrome (complete and partial phenotypes) | genetic male[162] | one in 99,000 births (0.001%)[163] |
| Idiopathic (no discernable medical cause) | none | one in 110,000 births (0.0009%)[139] |
| Iatrogenic (caused by medical treatment, e.g., progestin administered to pregnant mother) | none | no estimate |
| 5-alpha-reductase deficiency | male | no estimate |
| Mixed gonadal dysgenesis | none | no estimate |
Population figures can vary due to genetic causes. In the Dominican Republic, 5-alpha-reductase deficiency is not uncommon in the town of Las Salinas, resulting in social acceptance of the intersex trait.[164] Men with the trait are called "güevedoces" (Spanish for "eggs at twelve"). 12 out of 13 families had one or more male family members that carried the gene. The overall incidence for the town was 1 in every 90 males were carriers, with other males either non-carriers or non-affected carriers.[165]
Medical classifications
Sexual differentiation
The common pathway of sexual differentiation, where a productive human female has an XX chromosome pair, and a productive male has an XY pair, is relevant to the development of intersex conditions.
During fertilization, the sperm adds either an X (female) or a Y (male) chromosome to the X in the ovum. This determines the genetic sex of the embryo.[166] During the first weeks of development, genetic male and female fetuses are "anatomically indistinguishable", with primitive gonads beginning to develop during approximately the sixth week of gestation. The gonads, in a "bipotential state", may develop into either testes (the male gonads) or ovaries (the female gonads), depending on the consequent events.[166] Through the seventh week, genetically female and genetically male fetuses appear identical.
At around eight weeks of gestation, the gonads of an XY embryo differentiate into functional testes, secreting testosterone. Ovarian differentiation, for XX embryos, does not occur until approximately week 12 of gestation. In typical female differentiation, the Müllerian duct system develops into the uterus, Fallopian tubes, and inner third of the vagina. In males, the Müllerian duct-inhibiting hormone MIH causes this duct system to regress. Next, androgens cause the development of the Wolffian duct system, which develops into the vas deferens, seminal vesicles, and ejaculatory ducts.[166] By birth, the typical fetus has been completely "sexed" male or female, meaning that the genetic sex (XY-male or XX-female) corresponds with the phenotypical sex; that is to say, genetic sex corresponds with internal and external gonads, and external appearance of the genitals.
Signs
There are a variety of symptoms that can occur. Ambiguous genitalia being the most common sign, there can be micropenis, clitoromegaly, partial labial fusion, electrolyte abnormalities, delayed or absent puberty, unexpected changes at puberty, hypospadias, labial or inguinal (groin) masses (which may turn out to be testes) in girls and undescended testes (which may turn out to be ovaries) in boys.[167]
Ambiguous genitalia
Ambiguous genitalia may appear as a large clitoris or as a small penis.
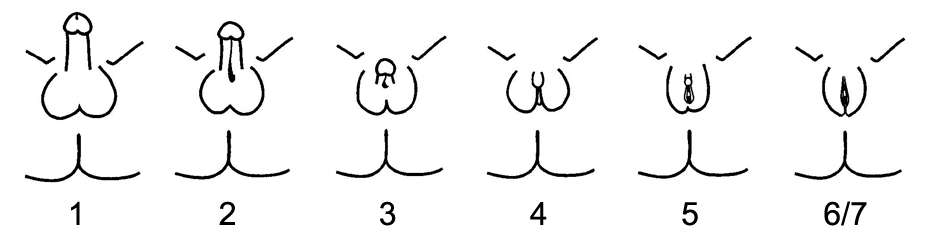
Because there is variation in all of the processes of the development of the sex organs, a child can be born with a sexual anatomy that is typically female or feminine in appearance with a larger-than-average clitoris (clitoral hypertrophy) or typically male or masculine in appearance with a smaller-than-average penis that is open along the underside. The appearance may be quite ambiguous, describable as female genitals with a very large clitoris and partially fused labia, or as male genitals with a very small penis, completely open along the midline ("hypospadic"), and empty scrotum. Fertility is variable.
Measurement systems for ambiguous genitalia
The orchidometer is a medical instrument to measure the volume of the testicles. It was developed by Swiss pediatric endocrinologist Andrea Prader. The Prader scale[168] and Quigley scale are visual rating systems that measure genital appearance. These measurement systems were satirized in the Phall-O-Meter, created by the (now defunct) Intersex Society of North America.[169][170][171]
Other signs
In order to help in classification, methods other than a genitalia inspection can be performed. For instance, a karyotype display of a tissue sample may determine which of the causes of intersex is prevalent in the case. Additionally, electrolyte tests, endoscopic exam, ultrasound and hormone stimulation tests can be done.[172]
Causes
Intersex can be divided into four categories which are: 46, XX intersex; 46, XY intersex; true gonadal intersex; and complex or undetermined intersex.
46, XX intersex
This condition used to be called "female pseudohermaphroditism". Persons with this condition have female internal genitalia and karyotype (XX) and various degree of external genitalia virilization.[173] External genitalia is masculinized congenitally when female fetus is exposed to excess androgenic environment.[167] Hence, the chromosome of the person is of a woman, the ovaries of a woman, but external genitals that appear like a male. The labia fuse, and the clitoris enlarges to appear like a penis. The causes of this can be male hormones taken during pregnancy, congenital adrenal hyperplasia, male-hormone-producing tumors in the mother and aromatase deficiency.[167]
46, XY intersex
This condition used to be called "male pseudohermaphroditism". This is defined as incomplete masculinization of the external genitalia.[174] Thus, the person has the chromosomes of a man, but the external genitals are incompletely formed, ambiguous, or clearly female.[167][175] This condition is also called 46, XY with undervirilization.[167] 46, XY intersex has many possible causes, which can be problems with the testes and testosterone formation.[167] Also, there can be problems with using testosterone. Some people lack the enzyme needed to convert testosterone to dihydrotestosterone, which is a cause of 5-alpha-reductase deficiency.[167] Androgen Insensitivity Syndrome is the most common cause of 46, XY intersex.[167]
True gonadal intersex
This condition used to be called "true hermaphroditism". This is defined as having asymmetrical gonads with ovarian and testicular differentiation on either sides separately or combined as ovotestis.[176] In most cases, the cause of this condition is unknown; however, some research has linked it to exposure to common agricultural pesticides.[176]
Complex or undetermined intersex
This is the condition of having any chromosome configurations rather than 46, XX or 46, XY intersex.[167] This condition does not result in any imbalance between internal and external genitalia.[167] However, there may be problems with sex hormone levels, overall sexual development, and altered numbers of sex chromosomes.[167]
Conditions
There are a variety of opinions on what conditions or traits are and are not intersex, dependent on the definition of intersex that is used. Current human rights based definitions stress a broad diversity of sex characteristics that differ from expectations for male or female bodies.[2] During 2015, the Council of Europe,[58] the European Union Agency for Fundamental Rights[145] and Inter-American Commission on Human Rights[146] have called for a review of medical classifications on the basis that they presently impede enjoyment of the right to health; the Council of Europe expressed concern that "the gap between the expectations of human rights organisations of intersex people and the development of medical classifications has possibly widened over the past decade".[58][145][146]
| List of conditions | ||
|---|---|---|
| Sex chromosomes | Name | Description |
| XX | Congenital adrenal hyperplasia (CAH) | The most common cause of sexual ambiguity is congenital adrenal hyperplasia (CAH), an endocrine condition in which the adrenal glands produce atypically high levels of virilizing hormones in utero. The genes that cause CAH can now be detected in the developing embryo. As Fausto-Sterling mentioned in chapter 3 of Sexing the Body, "a woman who suspects she may be pregnant with a CAH baby (if she or someone in her family carries CAH) can undergo treatment and then get tested." To prevent an XX-CAH child's genitalia from becoming masculinized, a treatment, which includes the use of the steroid dexamethasone, can begin as early as four weeks after formation. Many do not favor this process because "the safety of this experimental therapy has not been established in rigorously controlled trials", it does allow physicians to detect CAH, therefore enabling the start of treatment right after birth. Starting treatment as soon as an XX-CAH baby is born not only minimizes but also may even eliminate the chances of genital surgery from being performed.[139] However, the necessity of such surgery itself is disputed.
Meta-analysis of the studies supporting the use of dexamethasone on CAH at-risk fetuses found "less than one half of one percent of published 'studies' of this intervention were regarded as being of high enough quality to provide meaningful data for a meta-analysis. Even these four studies were of low quality" ... "in ways so slipshod as to breach professional standards of medical ethics"[177] and "there were no data on long-term follow-up of physical and metabolic outcomes in children exposed to dexamethasone".[178] In XX-females, this can range from partial masculinization that produces a large clitoris, to virilization and male appearance. The latter applies in particular to congenital adrenal hyperplasia due to 21-hydroxylase deficiency, which is the most common form of CAH. Individuals born with XX chromosomes affected by 17α-hydroxylase deficiency are born with female internal and external anatomy, but, at puberty, neither the adrenals nor the ovaries can produce sex-hormones, inhibiting breast development and the growth of pubic hair. See below for XY CAH 17α-hydroxylase deficiency. |
| XX | Progestin-induced virilisation | In this case, the excess androgen hormones are caused by the use of progestin, a drug that was used in the 1950s and 1960s to prevent miscarriage. These individuals typically have internal and external female anatomy, with functional ovaries and will therefore have menstruation. They develop, however, some male secondary sex characteristics and they frequently have unusually large clitorises. In very advanced cases, such children have initially been identified as males. |
| XX | Freemartinism | This condition occurs commonly in all species of cattle and affects most females born as a twin to a male. It is rare or unknown in other mammals, including humans. In cattle, the placentae of fraternal twins usually fuse at some time during the pregnancy, and the twins then share their blood supply. If the twins are of different sexes, male hormones produced in the body of the fetal bull find their way into the body of the fetal heifer (female), and masculinize her. Her sexual organs do not develop fully, and her ovaries may even contain testicular tissue. When adult, such a freemartin is very like a typical female in external appearance, but she is infertile, and behaves more like a castrated male (a steer). The male twin is not significantly affected, although (if he remains entire) his testes may be slightly reduced in size. The degree of masculinization of the freemartin depends on the stage of pregnancy at which the placental fusion occurs – in about ten percent of such births no fusion occurs and both calves develop typically for their chromosomal sex. |
| XY | Androgen insensitivity syndrome (AIS) | People with AIS have a Y chromosome, (typically XY), but are unable to metabolize androgens in varying degrees.
Cases with typically female appearance and genitalia are said to have complete androgen insensitivity syndrome (CAIS). People with CAIS have a vagina and no uterus, cervix, or ovaries, and are infertile. The vagina may be shorter than usual, and, in some cases, is nearly absent. Instead of female internal reproductive organs, a person with CAIS has undescended or partially descended testes, of which the person may not even be aware. In mild and partial androgen insensitivity syndrome (MAIS and PAIS), the body is partially receptive to androgens, so there is virilization to varying degrees. PAIS can result in genital ambiguity, due to limited metabolization of the androgens produced by the testes. Ambiguous genitalia may present as a large clitoris, known as clitoromegaly, or a small penis, which is called micropenis or microphallus; hypospadias and cryptorchidism may also be present, with one or both testes undescended, and hypospadias appearing just below the glans on an otherwise typical male penis, or at the base of the shaft, or at the perineum and including a bifid (or cleft) scrotum. |
| XY | 5-alpha-reductase deficiency (5-ARD) | The condition affects individuals with a Y chromosome, making their bodies unable to convert testosterone to dihydrotestosterone (DHT). DHT is necessary for the development of male genitalia in utero, and plays no role in female development, so its absence tends to result in ambiguous genitalia at birth; the effects can range from infertility with male genitalia to male underdevelopment with hypospadias to female genitalia with mild clitoromegaly. The frequency is unknown, and children are sometimes misdiagnosed as having AIS.[179] Individuals can have testes, as well as vagina and labia, and a small penis capable of ejaculation that looks like a clitoris at birth. Such individuals are usually raised as girls. The lack of DHT also limits the development of facial hair. |
| XY | Congenital adrenal hyperplasia (CAH) | In individuals with a Y chromosome (typically XY) who have Congenital adrenal hyperplasia due to 17 alpha-hydroxylase deficiency, CAH inhibits virilization, unlike cases without a Y chromosome. |
| XY | Persistent Müllerian duct syndrome (PMDS) | The child has XY chromosomes typical of a male. The child has a male body and an internal uterus and fallopian tubes because his body did not produce Müllerian inhibiting factor during fetal development. |
| XY | Anorchia | Individuals with XY chromosomes whose gonads were lost after 14 weeks of fetal development. People with anorchia have no ability to produce the hormones responsible for developing male secondary sex characteristics nor the means to produce gametes necessary for reproduction due to the lack of gonads. They may develop typically feminine secondary sex characteristics without or despite the administration of androgens to artificially initiate physical sex differentiation (typically planned around the age of puberty). Psychological and neurological gender identity may solidify before the administration of androgens, leading to gender dysphoria, as anorchic individuals are typically assigned male at birth. |
| XY | Gonadal dysgenesis | It has various causes and are not all genetic; a catch-all category. It refers to individuals (mostly XY) whose gonads don't develop properly. Clinical features are heterogeneous.[139] |
| XY | Hypospadias | It is caused by various causes, including alterations in testosterone metabolism. The urethra does not run to the tip of the penis. In mild forms, the opening is just shy of the tip; in moderate forms, it is along the shaft; and in severe forms, it may open at the base of the penis.[139] |
| Other | Unusual chromosomal sex | In addition to the most common XX and XY chromosomal sexes, there are several other possible combinations, for example Turner syndrome (XO), Triple X syndrome (XXX), Klinefelter syndrome (XXY) and variants (XXYY, XXXY, XXXXY), XYY syndrome, de la Chapelle syndrome (XX male), Swyer syndrome (XY female). |
| Other | Mosaicism and chimerism | A mix can occur, where some of the cells of the body have the common XX or XY, while some have one of the less usual chromosomal contents above. Such a mixture is caused by either mosaicism or chimerism. In mosaicism, the mixture is caused by a mutation in one of the cells of the embryo after fertilization, whereas chimerism is a fusion of two embryos.
In alternative fashion, it is simply a mixture between XX and XY, and does not have to involve any less-common genotypes in individual cells. This, too, can occur both as chimerism and as a result of one sex chromosome having mutated into the other.[180] Mosaicism and chimerism may involve chromosomes other than the sex chromosomes, and not result in intersex traits. |
| Other | Ovotesticular disorder (formerly known as true hermaphroditism) | A "true hermaphrodite" is defined as someone with both testicular and ovarian tissue. There is a spectrum of forms of ovotesticular disorder. The varieties include having two ovotestes, or one ovary and one ovotestis. Phenotype is not determinable from the ovotestes; in some cases, the appearance is "fairly typically female"; in others, it is "fairly typically male", and it may also be "fairly in-between in terms of genital development."[181] Intersex activist Cheryl Chase is an example of someone with ovotestes.[182] |
Medical interventions

Rationales
Medical interventions take place to address physical health concerns and psychosocial risks. Both types of rationale are the subject of debate, particularly as the consequences of surgical (and many hormonal) interventions are lifelong and irreversible. Questions regarding physical health include accurately assessing risk levels, necessity, and timing. Psychosocial rationales are particularly susceptible to questions of necessity as they reflect social and cultural concerns.
There remains no clinical consensus about an evidence base, surgical timing, necessity, type of surgical intervention, and degree of difference warranting intervention.[183][184][185] Such surgeries are the subject of significant contention due to consequences that include trauma, impact on sexual function and sensation, and violation of rights to physical and mental integrity.[1] This includes community activism,[44] and multiple reports by international human rights[18][58][22][186] and health[79] institutions and national ethics bodies.[21][187]
In the cases where gonads may pose a cancer risk, as in some cases of androgen insensitivity syndrome,[188] concern has been expressed that treatment rationales and decision-making regarding cancer risk may encapsulate decisions around a desire for surgical "normalization".[20]
Types
- Feminizing and masculinizing surgeries: Surgical procedures depend on diagnosis, and there is often concern as to whether surgery should be performed at all. Typically, surgery is performed shortly after birth. Defenders of the practice argue that it is necessary for individuals to be clearly identified as male or female in order for them to function socially and develop "normally". Psychosocial reasons are often stated.[8] This is criticised by many human rights institutions, and authors. Unlike other aesthetic surgical procedures performed on infants, such as corrective surgery for a cleft lip, genital surgery may lead to negative consequences for sexual functioning in later life, or feelings of freakishness and unacceptability.[189]
- Hormone treatment: There is widespread evidence of prenatal testing and hormone treatment to prevent or eliminate intersex traits,[190][191] associated also with the problematization of sexual orientation and gender non-conformity.[190][192]
- Psychosocial support: All stakeholders support psychosocial support. A joint international statement by participants at the Third International Intersex Forum in 2013 sought, amongst other demands: "Recognition that medicalization and stigmatisation of intersex people result in significant trauma and mental health concerns. In view of ensuring the bodily integrity and well-being of intersex people, autonomous non-pathologising psycho-social and peer support be available to intersex people throughout their life (as self-required), as well as to parents and/or care providers."
- Genetic selection and terminations: The ethics of preimplantation genetic diagnosis to select against intersex traits was the subject of 11 papers in the October 2013 issue of the American Journal of Bioethics.[193] There is widespread evidence of pregnancy terminations arising from prenatal testing, as well as prenatal hormone treatment to prevent intersex traits. Behrmann and Ravitsky find social concepts of sex, gender and sexual orientation to be "intertwined on many levels. Parental choice against intersex may thus conceal biases against same-sex attractedness and gender nonconformity."[116]
- Medical display. Photographs of intersex children's genitalia are circulated in medical communities for documentary purposes, and individuals with intersex traits may be subjected to repeated genital examinations and display to medical teams. Problems associated with experiences of medical photography of intersex children have been discussed[194] along with their ethics, control and usage.[195][196] "The experience of being photographed has exemplified for many people with intersex conditions the powerlessness and humiliation felt during medical investigations and interventions".[195]
- Gender dysphoria: The DSM-5 included a change from using gender identity disorder to gender dysphoria. This revised code now specifically includes intersex people who do not identify with their sex assigned at birth and experience clinically significant distress or impairment, using the language of disorders of sex development.[197]
References
Notes
- UN Committee against Torture; UN Committee on the Rights of the Child; UN Committee on the Rights of People with Disabilities; UN Subcommittee on Prevention of Torture and other Cruel, Inhuman or Degrading Treatment or Punishment; Juan Méndez; Dainius Pῡras; Dubravka Šimonoviæ; Marta Santos Pais; African Commission on Human and Peoples' Rights; Council of Europe Commissioner for Human Rights; Inter-American Commission on Human Rights (24 October 2016), "Intersex Awareness Day – Wednesday 26 October. End violence and harmful medical practices on intersex children and adults, UN and regional experts urge", Office of the High Commissioner for Human Rights, archived from the original on 21 November 2016
- "Free & Equal Campaign Fact Sheet: Intersex" (PDF). United Nations Office of the High Commissioner for Human Rights. 2015. Archived (PDF) from the original on 4 March 2016. Retrieved 28 March 2016.
- Saner, Emine (29 July 2008). "The gender trap: testing the sex of Olympians competing in Beijing". The Guardian. ISSN 0261-3077. Retrieved 11 June 2020.
- Mason H.J. (1978). "Favorinus' Disorder: Reifenstein's Syndrome in Antiquity?". Janus. 66 (1–2–3): 1–13. PMID 11610651.
- Nguyễn Khắc Thuần (1998), Việt sử giai thoại (History of Vietnam's tales), vol. 8, Vietnam Education Publishing House, p. 55
- Zucker, Kenneth J.; Bradley, Susan J.; Sullivan, Claire B. Lowry (March 1992). "Gender Identity Disorder in Children". Annual Review of Sex Research. 3 (1): 73–120. doi:10.1080/10532528.1992.10559876. ISSN 1053-2528.
- Dreger, Alice D.; Chase, Cheryl; Sousa, Aron; Gruppuso, Phillip A.; Frader, Joel (18 August 2005). "Changing the Nomenclature/Taxonomy for Intersex: A Scientific and Clinical Rationale". Journal of Pediatric Endocrinology and Metabolism. 18 (8): 729–33. doi:10.1515/JPEM.2005.18.8.729. PMID 16200837.
- Houk, C. P.; Hughes, I. A.; Ahmed, S. F.; Lee, P. A.; Writing Committee for the International Intersex Consensus Conference Participants (August 2006). "Summary of Consensus Statement on Intersex Disorders and Their Management". Pediatrics. 118 (2): 753–757. doi:10.1542/peds.2006-0737. ISSN 0031-4005. PMID 16882833.
- Davis, Georgiann (11 September 2015). Contesting Intersex: The Dubious Diagnosis. New York University Press. pp. 87–89. ISBN 978-1479887040.
- Holmes, Morgan (September 2011). "The Intersex Enchiridion: Naming and Knowledge". Somatechnics. 1 (2): 388–411. doi:10.3366/soma.2011.0026. ISSN 2044-0138.
- Diamond M, Beh HG (27 July 2006). Variations of Sex Development Instead of Disorders of Sex Development. Archived 21 August 2008 at the Wayback Machine Arch Dis Child
- Civil Society Coalition on Human Rights and Constitutional Law; Human Rights Awareness and Promotion Forum; Rainbow Health Foundation; Sexual Minorities Uganda; Support Initiative for Persons with Congenital Disorders (2014). "Uganda Report of Violations based on Sex Determination, Gender Identity, and Sexual Orientation". Archived from the original on 3 May 2015. Retrieved 15 May 2017.
- Grady, Helen; Soy, Anne (4 May 2017). "The midwife who saved intersex babies". BBC World Service, Kenya. Archived from the original on 15 May 2017.
- Beyond the Boundary – Knowing and Concerns Intersex (October 2015). "Intersex report from Hong Kong China, and for the UN Committee Against Torture: the Convention against Torture and Other Cruel Inhuman or Degrading Treatment or Punishment". Archived from the original on 26 March 2017.
- Submission 88 to the Australian Senate inquiry on the involuntary or coerced sterilisation of people with disabilities in Australia Archived 23 September 2015 at the Wayback Machine, Australasian Paediatric Endocrine Group (APEG), 27 June 2013
- Jordan-Young, R. M.; Sonksen, P. H.; Karkazis, K. (April 2014). "Sex, health, and athletes". BMJ. 348 (apr28 9): –2926–g2926. doi:10.1136/bmj.g2926. ISSN 1756-1833. PMID 24776640.
- Macur, Juliet (6 October 2014). "Fighting for the Body She Was Born With". The New York Times. Archived from the original on 12 January 2015. Retrieved 9 February 2015.
- Report of the UN Special Rapporteur on Torture Archived 24 August 2016 at the Wayback Machine, Office of the UN High Commissioner for Human Rights, February 2013.
- Eliminating forced, coercive and otherwise involuntary sterilization, An interagency statement Archived 11 July 2015 at the Wayback Machine, World Health Organization, May 2014.
- Senate of Australia; Community Affairs References Committee (2013). Involuntary or coerced sterilisation of intersex people in Australia. Australian Senate. Canberra. ISBN 978-1-74229-917-4. Archived from the original on 23 September 2015.
- Swiss National Advisory Commission on Biomedical Ethics NEK-CNE (November 2012). On the management of differences of sex development. Ethical issues relating to "intersexuality".Opinion No. 20/2012 (PDF). 2012. Berne. Archived from the original (PDF) on 23 April 2015. Retrieved 24 July 2018.
- Asia Pacific Forum of National Human Rights Institutions (June 2016). Promoting and Protecting Human Rights in relation to Sexual Orientation, Gender Identity and Sex Characteristics. ISBN 978-0-9942513-7-4. Archived from the original on 15 January 2017.
- Domurat Dreger, Alice (2001). Hermaphrodites and the Medical Invention of Sex. USA: Harvard University Press. ISBN 978-0-674-00189-3.
- "New publication "Intersex: Stories and Statistics from Australia"". Organisation Intersex International Australia. 3 February 2016. Archived from the original on 29 August 2016. Retrieved 18 August 2016.
- International Commission of Jurists. "In re Völling, Regional Court Cologne, Germany (6 February 2008)". Archived from the original on 5 January 2016. Retrieved 27 December 2015.
- Reuters (1 April 2015). "Surgery and Sterilization Scrapped in Malta's Benchmark LGBTI Law". The New York Times.
- Star Observer (2 April 2015). "Malta passes law outlawing forced surgical intervention on intersex minors". Star Observer. Archived from the original on 14 August 2015.
- Knox, David; Schacht, Caroline. (2010) Choices in Relationships: An Introduction to Marriage and the Family Archived 25 September 2015 at the Wayback Machine. 11 ed. Cengage Learning. ISBN 9781111833220. p. 64.
- "What is intersex?". Intersex Society of North America. Archived from the original on 10 November 2013. Retrieved 18 November 2013.
- Diodorus Siculus (1935). Library of History (Book IV). Loeb Classical Library Volumes 303 and 340. C H Oldfather (trans.). Cambridge, MA: Harvard University Press. Archived from the original on 27 September 2008.
- Swami., Parmeshwaranand (2004). Encyclopaedia of the Śaivism (1st ed.). New Delhi: Sarup & Sons. ISBN 978-8176254274. OCLC 54930404.
- Shankar, Gopi (March–April 2015). "The Many Genders of Old India". The Gay & Lesbian Review Worldwide. 22: 24–26 – via ProQuest.
- DeVun, Leah (June 2018). "Heavenly hermaphrodites: sexual difference at the beginning and end of time". Postmedieval. 9 (2): 132–146. doi:10.1057/s41280-018-0080-8. ISSN 2040-5960.
- Pliny, Natural History 7.34: gignuntur et utriusque sexus quos hermaphroditos vocamus, olim androgynos vocatos; Veronique Dasen, "Multiple Births in Graeco-Roman Antiquity," Oxford Journal of Archaeology 16.1 (1997), p. 61.
- Lynn E. Roller, "The Ideology of the Eunuch Priest," Gender & History 9.3 (1997), p. 558.
- Decretum Gratiani, C. 4, q. 2 et 3, c. 3
- "Decretum Gratiani (Kirchenrechtssammlung)". Bayerische StaatsBibliothek (Bavarian State Library). 5 February 2009. Archived from the original on 20 December 2016.
- Raming, Ida; Macy, Gary; Bernard J, Cook (2004). A History of Women and Ordination. Scarecrow Press. p. 113.
- E Coke, The First Part of the Institutes of the Laws of England, Institutes 8.a. (1st Am. Ed. 1812) (16th European ed. 1812).
- Greenberg, Julie (1999). "Defining Male and Female: Intersexuality and the Collision Between Law and Biology". Arizona Law Review. 41: 277–278. SSRN 896307.
- "India's Third Gender Rises Again". Sapiens. Wenner-Gren Foundation for Anthropological Research. 26 September 2019. Retrieved 26 April 2020.
- "Hijra: India's third gender claims its place in law". The Guardian. 16 April 2014. Retrieved 26 April 2020.
- Holmes, Morgan (July 2004). "Locating Third Sexes" (PDF). Transformations Journal (8). ISSN 1444-3775. Retrieved 28 December 2014.
- Intersex Issues in the International Classification of Diseases: a revision (PDF). Mauro Cabral, Morgan Carpenter (eds.). 2014. Archived (PDF) from the original on 11 August 2016.CS1 maint: others (link)
- Goldschmidt, R. (1917), "Intersexuality and the endocrine aspect of sex", Endocrinology, 1 (4): 433–456, doi:10.1210/endo-1-4-433.
- Cawadias, A. P. (1943) Hermaphoditus the Human Intersex, London, Heinemann Medical Books Ltd.
- Coran, Arnold G.; Polley, Theodore Z. (July 1991). "Surgical management of ambiguous genitalia in the infant and child". Journal of Pediatric Surgery. 26 (7): 812–820. CiteSeerX 10.1.1.628.4867. doi:10.1016/0022-3468(91)90146-K. PMID 1895191.
- Hughes, I A; Houk, C; Ahmed, S F; Lee, P A; LWPES1/ESPE2 Consensus Group (June 2005). "Consensus statement on management of intersex disorders". Archives of Disease in Childhood. 91 (7): 554–563. doi:10.1136/adc.2006.098319. ISSN 0003-9888. PMC 2082839. PMID 16624884.
- Dreger, Alice Domurat (May 1998). ""Ambiguous Sex"--or Ambivalent Medicine?". The Hastings Center Report. 28 (3): 24–35. doi:10.2307/3528648. JSTOR 3528648. PMID 9669179.
- Dreger, Alice (3 April 2015). "Malta Bans Surgery on Intersex Children". The Stranger SLOG. Archived from the original on 18 July 2015.
- Public statement by the third international intersex forum. Malta. 2 December 2013. Archived from the original on 24 November 2016.
- Odero, Joseph (23 December 2015). "Intersex in Kenya: Held captive, beaten, hacked. Dead". 76 CRIMES. Archived from the original on 25 April 2016. Retrieved 1 October 2016.
- Warne, Garry L.; Raza, Jamal (September 2008). "Disorders of sex development (DSDs), their presentation and management in different cultures". Reviews in Endocrine and Metabolic Disorders. 9 (3): 227–236. CiteSeerX 10.1.1.469.9016. doi:10.1007/s11154-008-9084-2. ISSN 1389-9155. PMID 18633712.
- Ghattas, Dan Christian; Heinrich-Böll-Stiftung (2013). Human Rights between the Sexes A preliminary study on the life situations of inter*individuals (PDF). Berlin: Heinrich-Böll-Stiftung. ISBN 978-3-86928-107-0. Archived (PDF) from the original on 23 September 2015.
- "Intersex", Radio Netherlands Archives, April 21, 2004
- Carpenter, Morgan (December 2018). "Intersex Variations, Human Rights, and the International Classification of Diseases". Health and Human Rights. 20 (2): 205–214. PMC 6293350. PMID 30568414.
- Greenberg, Julie A. (June 2017). "Legal, ethical, and human rights considerations for physicians treating children with atypical or ambiguous genitalia". Seminars in Perinatology. 41 (4): 252–255. doi:10.1053/j.semperi.2017.03.012. PMID 28478089.
- Council of Europe; Commissioner for Human Rights (April 2015), Human rights and intersex people, Issue Paper, archived from the original on 6 January 2016
- Curtis, Skyler (2010–2011). "Reproductive Organs and Differences of Sex Development: The Constitutional Issues Created by the Surgical Treatment of Intersex Children". McGeorge Law Review. 42: 863. Archived from the original on 18 December 2014. Retrieved 15 November 2012.
- "Corte Constitucional de Colombia: Sentencia T-1025/02". Archived from the original on 20 February 2013. Retrieved 2 December 2012.
- Office of the High Commissioner for Human Rights. "United Nations for Intersex Awareness". Archived from the original on 12 November 2016. Retrieved 12 November 2016.
- Government Gazette Archived 9 June 2011 at the Wayback Machine, Republic of South Africa, Vol. 487, Cape Town, 11 January 2006.
- Sex Discrimination Amendment (Sexual Orientation, Gender Identity and Intersex Status) Act 2013, No. 98, 2013 Archived 6 October 2014 at the Wayback Machine, ComLaw, C2013A00098, 2013.
- On the historic passing of the Sex Discrimination Amendment (Sexual Orientation, Gender Identity and Intersex Status) Act 2013 Archived 6 October 2014 at the Wayback Machine, Organisation Intersex International Australia, 25 June 2013.
- Malta (April 2015), Gender Identity, Gender Expression and Sex Characteristics Act: Final version
- Cabral, Mauro (8 April 2015). "Making depathologization a matter of law. A comment from GATE on the Maltese Act on Gender Identity, Gender Expression and Sex Characteristics". Global Action for Trans Equality. Archived from the original on 4 July 2015. Retrieved 3 July 2015.
- OII Europe (1 April 2015). "OII-Europe applauds Malta's Gender Identity, Gender Expression and Sex Characteristics Act. This is a landmark case for intersex rights within European law reform". Archived from the original on 22 May 2015. Retrieved 3 July 2015.
- Carpenter, Morgan (2 April 2015). "We celebrate Maltese protections for intersex people". Organisation Intersex International Australia. Archived from the original on 4 July 2015. Retrieved 3 July 2015.
- Transgender Europe (1 April 2015). Malta Adopts Ground-breaking Trans and Intersex Law – TGEU Press Release. Archived from the original on 3 November 2016.
- Zwischengeschlecht (12 August 2009). "Christiane Völling: Hermaphrodite wins damage claim over removal of reproductive organs". Archived from the original on 5 July 2015. Retrieved 20 July 2015.
- "Condenan al H. de Talca por error al determinar sexo de bebé". diario.latercera.com (in Spanish). Archived from the original on 15 February 2017. Retrieved 15 February 2017.
- García, Gabriela (20 June 2013). "Identidad forzada". www.paula.cl (in Spanish). Archived from the original on 15 February 2017.
- Zwischengeschlecht (17 December 2015). "Nuremberg Hermaphrodite Lawsuit: Michaela "Micha" Raab Wins Damages and Compensation for Intersex Genital Mutilations!". Archived from the original on 11 May 2016. Retrieved 21 December 2015.
- "M.C. V. AARONSON". Retrieved 1 August 2019.
- Dutta, Anatol; Pintens, Walter (12 September 2018), "Private International Law Aspects of Intersex", The Legal Status of Intersex Persons, Intersentia, pp. 415–426, doi:10.1017/9781780687704.026, ISBN 9781780687704
- Holmes, Morgan. "Is Growing up in Silence Better Than Growing up Different?". Intersex Society of North America. Archived from the original on 5 March 2016.
- Intersex Society of North America. "What's wrong with the way intersex has traditionally been treated?". Archived from the original on 26 June 2014.
- Carpenter, Morgan (3 February 2015). Intersex and ageing. Organisation Intersex International Australia. Archived from the original on 13 April 2015.
- World Health Organization (2015). Sexual health, human rights and the law. Geneva: World Health Organization. ISBN 9789241564984.
- "Kenya takes step toward recognizing intersex people in landmark ruling". Reuters. 5 December 2014. Archived from the original on 24 September 2015.
- Money, John; Ehrhardt, Anke A. (1972). Man & Woman Boy & Girl. Differentiation and dimorphism of gender identity from conception to maturity. USA: The Johns Hopkins University Press. ISBN 978-0-8018-1405-1.
- Furtado P. S.; et al. (2012). "Gender dysphoria associated with disorders of sex development". Nat. Rev. Urol. 9 (11): 620–627. doi:10.1038/nrurol.2012.182. PMID 23045263.
- Marañón, Gregorio (1929). Los estados intersexuales en la especie humana. Madrid: Morata.
- "Australian Government Guidelines on the Recognition of Sex and Gender, 30 May 2013". Archived from the original on 1 July 2015. Retrieved 6 October 2014.
- Holme, Ingrid (2008). "Hearing People's Own Stories". Science as Culture. 17 (3): 341–344. doi:10.1080/09505430802280784.
- "New Zealand Passports - Information about Changing Sex / Gender Identity". Archived from the original on 23 September 2014. Retrieved 6 October 2014.
- Third sex option on birth certificates Archived 10 October 2014 at the Wayback Machine, Deutsche Welle, 1 November 2013.
- "Intersex: Third Gender in Germany" (Spiegel, Huff Post, Guardian, ...): Silly Season Fantasies vs. Reality of Genital Mutilations Archived 24 June 2017 at the Wayback Machine, Zwischengeschlecht, 1 November 2013
- Sham package for Intersex: Leaving sex entry open is not an option Archived 29 August 2014 at the Wayback Machine, OII Europe, 15 February 2013
- Jones, Tiffany; Hart, Bonnie; Carpenter, Morgan; Ansara, Gavi; Leonard, William; Lucke, Jayne (2016). Intersex: Stories and Statistics from Australia (PDF). Cambridge, UK: Open Book Publishers. ISBN 978-1-78374-208-0. Archived from the original (PDF) on 14 September 2016. Retrieved 2 February 2016.
- Zderic, Stephen (2002). Pediatric gender assignment : a critical reappraisal; [proceedings from a conference ... in Dallas in the spring of 1999 which was entitled "pediatric gender assignment – a critical reappraisal"]. New York, NY [u.a.]: Kluwer Acad. / Plenum Publ. ISBN 978-0306467592.
- Frader, J.; Alderson, P.; Asch, A.; Aspinall, C.; Davis, D.; Dreger, A.; Edwards, J.; Feder, E. K.; Frank, A.; Hedley, L. A.; Kittay, E.; Marsh, J.; Miller, P. S.; Mouradian, W.; Nelson, H.; Parens, E. (May 2004). "Health care professionals and intersex conditions". Arch. Pediatr. Adolesc. Med. 158 (5): 426–8. CiteSeerX 10.1.1.572.1572. doi:10.1001/archpedi.158.5.426. PMID 15123472.
- Wiesemann, Claudia; Ude-Koeller, Susanne; Sinnecker, Gernot H. G.; Thyen, Ute (20 October 2009). "Ethical principles and recommendations for the medical management of differences of sex development (DSD)/intersex in children and adolescents" (PDF). European Journal of Pediatrics. 169 (6): 671–679. doi:10.1007/s00431-009-1086-x. PMC 2859219. PMID 19841941. Retrieved 6 September 2013.
- Diamond, Milton; H. Keith Sigmundson (1997). "Management of intersexuality: Guidelines for dealing with individuals with ambiguous genitalia". Archives of Pediatrics and Adolescent Medicine. June. Archived from the original on 8 February 2007. Retrieved 8 April 2007.
- Sharon Preves, "Intersex and Identity, the Contested Self". Rutgers, 2003.
- Catherine Harper, "Intersex". Berg, 2007.
- Johnson, Emilie K.; Rosoklija, Ilina; Finlayso, Courtney; Chen, Diane; Yerkes, Elizabeth B.; Madonna, Mary Beth; Holl, Jane L.; Baratz, Arlene B.; Davis, Georgiann; Cheng, Earl Y. (May 2017). "Attitudes towards "disorders of sex development" nomenclature among affected individuals". Journal of Pediatric Urology. 13 (6): 608.e1–608.e8. doi:10.1016/j.jpurol.2017.03.035. ISSN 1477-5131. PMID 28545802.
- Newswise (11 May 2017). "Term "Disorders of Sex Development" May Have Negative Impact". Newswise. Archived from the original on 15 May 2017. Retrieved 11 May 2017.
- Welcome to OII Australia – we promote human rights and bodily autonomy for intersex people, and provide information, education and peer support Archived 31 October 2014 at the Wayback Machine, Organisation Intersex International Australia, 4 April 2004
- Answers to Your Questions About Individuals With Intersex Conditions Archived 31 October 2014 at the Wayback Machine, American Psychological Association, 2006.
- Advocates for Informed Choice Archived 11 August 2011 at the Wayback Machine, Advocates for Informed Choice, undated, retrieved 19 September 2014
- interACT (May 2016). "interACT Statement on Intersex Terminology". Interact Advocates for Intersex Youth. Archived from the original on 8 June 2016. Retrieved 30 May 2016.
- Molina B Dayal, MD, MPH, Assistant Professor, Fertility and IVF Center, Division of Reproductive Endocrinology and Infertility, Medical Faculty Associates, George Washington University distingquishes what 'true hermaphroditism' encompasses in their study of Ovotestis. Found here: "Ovotesticular Disorder of Sexual Development". Archived from the original on 31 December 2007. Retrieved 2 January 2008.
- W. S. Alexander M.D., O. D. Beresford M.D., M.R.C.P. (1953) wrote about extensively about 'female pseudohermaphrodite' origins in utera, in his paper "Masculinization of Ovarian Origin, published An International Journal of Obstetrics and Gynaecology Volume 60 Issue 2 pp. 252–258, April 1953.
- Am J Psychiatry 164:1499–1505, October 2007: Noted Mayo Clinic researchers J.M. Bostwick, MD, and Kari A Martin MD in A Man's Brain in an Ambiguous Body: A Case of Mistaken Gender wrote of the distinctions in male pseudohermaphrodite condition.
- Langman, Jan; Thomas Sadler (2006). Langman's medical embryology. Hagerstown, MD: Lippincott Williams & Wilkins. p. 252. ISBN 978-0-7817-9485-5.
- "Is a person who is intersex a hermaphrodite? | Intersex Society of North America". Isna.org. Archived from the original on 1 July 2013. Retrieved 5 July 2013.
- Intersex Society of North America (24 May 2006). Why is ISNA using "DSD"? Archived 17 June 2006 at the Wayback Machine. Retrieved 4 June 2006.
- Feder, E. (2009) 'Imperatives of Normality: From "Intersex" to "Disorders of Sex Development".' A Journal of Lesbian and Gay Studies (GLQ), 15, 225–247.
- Briffa, Tony (8 May 2014), Tony Briffa writes on "Disorders of Sex Development", Organisation Intersex International Australia, archived from the original on 30 December 2014
- "Why Not "Disorders of Sex Development"?". UK Intersex Association. Retrieved 30 May 2016.
- Children's right to physical integrity Archived 26 December 2013 at the Wayback Machine, Council of Europe Parliamentary Assembly, Report Doc. 13297, 6 September 2013.
- "Trans? Intersex? Explained!". Inter/Act. Archived from the original on 18 October 2014. Retrieved 10 July 2013.
- "Basic differences between intersex and trans". Organisation Intersex International Australia. 3 June 2011. Archived from the original on 4 September 2014. Retrieved 10 July 2013.
- Cabral Grinspan, Mauro (25 October 2015), The marks on our bodies, Intersex Day, archived from the original on 5 April 2016
- Behrmann, Jason; Ravitsky, Vardit (October 2013). "Queer Liberation, Not Elimination: Why Selecting Against Intersex is Not "Straight" Forward". The American Journal of Bioethics. 13 (10): 39–41. doi:10.1080/15265161.2013.828131. ISSN 1526-5161. PMID 24024805.
- Dreger, Alice (4 May 2015). "Reasons to Add and Reasons NOT to Add "I" (Intersex) to LGBT in Healthcare" (PDF). Association of American Medical Colleges. Archived (PDF) from the original on 9 June 2016. Retrieved 18 May 2016. Cite journal requires
|journal=(help) - Koyama, Emi. "Adding the "I": Does Intersex Belong in the LGBT Movement?". Intersex Initiative. Archived from the original on 17 May 2016. Retrieved 18 May 2016.
- "Intersex for allies". 21 November 2012. Archived from the original on 7 June 2016. Retrieved 18 May 2016.
- OII releases new resource on intersex issues Archived 6 June 2014 at the Wayback Machine, Intersex for allies and Making services intersex inclusive by Organisation Intersex International Australia, via Gay News Network, 2 June 2014.
- Kaggwa, Julius (19 September 2016). "I'm an intersex Ugandan – life has never felt more dangerous". The Guardian. ISSN 0261-3077. Archived from the original on 6 October 2016. Retrieved 3 October 2016.
- Cabral, Mauro (26 October 2016). "IAD2016: A Message from Mauro Cabral". GATE – Global Action for Trans Equality. Archived from the original on 3 November 2016. Retrieved 12 November 2016.
- Leffler, Rebecca (26 May 2007). "Critics Week grand prize to 'XXY'". The Hollywood Reporter. Archived from the original on 30 September 2007. Retrieved 12 February 2017.
- "Meet television's groundbreaking intersex character". Buzzfeed. Archived from the original on 29 May 2016.
- ""Faking It" Breaks New Ground With First Intersex Actor To Play Intersex Character On TV". New Now Next. Archived from the original on 5 April 2016. Retrieved 5 April 2016.
- Androgen Insensitivity Syndrome Support Group Australia; Briffa, Anthony (22 January 2003). "Discrimination against People affected by Intersex Conditions: Submission to NSW Government" (PDF). Archived (PDF) from the original on 11 March 2016. Retrieved 16 May 2016.
- "Androgen Insensitivity Syndrome Support Group (AISSG)". Archived from the original on 21 January 2016. Retrieved 16 May 2016.
- "Dear ISNA Friends and Supporters". 2008. Archived from the original on 19 May 2016. Retrieved 16 May 2016.
- Holmes, Morgan (17 October 2015). "When Max Beck and Morgan Holmes went to Boston". Intersex Day. Archived from the original on 20 October 2015. Retrieved 24 October 2015.
- Winter, Gopi Shankar (2014). Maraikkappatta Pakkangal: மறைக்கப்பட்ட பக்கங்கள். Srishti Madurai. ISBN 9781500380939. OCLC 703235508.
- "the space between – Stanford prof: Talmudic rabbis were into analyzing sexuality – j. the Jewish news weekly of Northern California". 19 September 2014. Archived from the original on 10 October 2014. Retrieved 6 October 2014.
- Klaudia Snochowska-Gonzales. "Walasiewicz była kobietą (Walasiewicz Was a Woman)". Gazeta Wyborcza (in Polish). 190 (14 August 2004): 8. Retrieved 31 May 2006.
- Cooky, Cheryl; Shari L. Dworkin (February 2013). "Policing the Boundaries of Sex: A Critical Examination of Gender Verification and the Caster Semenya Controversy". Journal of Sex Research. 50 (2): 103–111. doi:10.1080/00224499.2012.725488. PMID 23320629.
- Karkazis, Katrina; Jordan-Young, Rebecca; Davis, Georgiann; Camporesi, Silvia (July 2012). "Out of Bounds? A Critique of the New Policies on Hyperandrogenism in Elite Female Athletes". The American Journal of Bioethics. 12 (7): 3–16. doi:10.1080/15265161.2012.680533. ISSN 1526-5161. PMC 5152729. PMID 22694023.
- "UN Human Rights Council: resolution, statement and side event, "The time has come"". Organisation Intersex International Australia. 11 September 2014. Archived from the original on 30 September 2014. Retrieved 28 September 2014.
- Pūras, Dainius; Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health (4 April 2016), Sport and healthy lifestyles and the right to health. Report A/HRC/32/33, United Nations, archived from the original on 15 December 2016
- "How common is intersex? | Intersex Society of North America". Isna.org. Archived from the original on 22 August 2009. Retrieved 21 August 2009.
- Blackless, Melanie; Charuvastra, Anthony; Derryck, Amanda; Fausto-Sterling, Anne; Lauzanne, Karl; Lee, Ellen (March 2000). "How sexually dimorphic are we? Review and synthesis". American Journal of Human Biology. 12 (2): 151–166. doi:10.1002/(SICI)1520-6300(200003/04)12:2<151::AID-AJHB1>3.0.CO;2-F. ISSN 1520-6300. PMID 11534012.
- Fausto-Sterling, Anne (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. Basic Books. pp. 53. ISBN 978-0-465-07714-4.
- "On the number of intersex people". Organisation Intersex International Australia. 28 September 2013. Archived from the original on 4 July 2015. Retrieved 4 July 2015.
- Chaleyer, Rani (10 March 2015). "Intersex: the 'I' in 'LGBTI'". Special Broadcasting Service. Archived from the original on 5 July 2015. Retrieved 4 July 2015.
- "The Five Sexes: why male and female is not enough" (PDF). Archived from the original (PDF) on 13 March 2016.
- Vilain E; Achermann JC; Eugster EA; Harley VR; Morel Y; Wilson JD; Hiort O (2007). "We used to call them hermaphrodites". Genetics in Medicine. 9 (2): 65–66. doi:10.1097/gim.0b013e31802cffcf. PMID 17304046.
- "Intersex population figures". 28 September 2013.
- European Union Agency for Fundamental Rights (April 2015), The fundamental rights situation of intersex people (PDF), archived (PDF) from the original on 5 March 2016
- Comisión Interamericana de Derechos Humanos (12 November 2015), Violencia contra Personas Lesbianas, Gays, Bisexuales, Trans e Intersex en América (PDF) (in Spanish), Comisión Interamericana de Derechos Humanos, archived (PDF) from the original on 7 January 2016
- Witchel, Selma Feldman; Azziz, Ricardo (2010). "Nonclassic Congenital Adrenal Hyperplasia". International Journal of Pediatric Endocrinology. 2010: 625105. doi:10.1155/2010/625105. PMC 2910408. PMID 20671993.
- Speiser, Phyllis W.; Azziz, Ricardo; Baskin, Laurence S.; Ghizzoni, Lucia; Hensle, Terry W.; Merke, Deborah P.; Meyer-Bahlburg, Heino F. L.; Miller, Walter L.; Montori, Victor M.; Oberfield, Sharon E.; Ritzen, Martin; White, Perrin C. (2010). "Congenital Adrenal Hyperplasia Due to Steroid 21-Hydroxylase Deficiency: An Endocrine Society Clinical Practice Guideline". Journal of Clinical Endocrinology & Metabolism. 95 (9): 4133–4160. doi:10.1210/jc.2009-2631. PMC 2936060. PMID 20823466.
Nonclassic forms of CAH are more prevalent, occurring in approximately 0.1–0.2% in the general Caucasian population but in up to 1–2% among inbred populations, such as Eastern European (Ashkenazi) Jews
- Springer, A.; van den Heijkant, M.; Baumann, S. (June 2016). "Worldwide prevalence of hypospadias". Journal of Pediatric Urology. 12 (3): 152.e1–152.e7. doi:10.1016/j.jpurol.2015.12.002. PMID 26810252.
- "Klinefelter syndrome Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 19 December 2019.
- Wigby, Kristen; D'Epagnier, Cheryl; Howell, Susan; Reicks, Amy; Wilson, Rebecca; Cordeiro, Lisa; Tartaglia, Nicole (November 2016). "Expanding the phenotype of Triple X syndrome: A comparison of prenatal versus postnatal diagnosis". American Journal of Medical Genetics Part A. 170 (11): 2870–2881. doi:10.1002/ajmg.a.37688. PMC 6501572. PMID 27644018.
- Reference, Genetics Home. "Turner syndrome". Genetics Home Reference. Retrieved 19 December 2019.
- Morcel, Karine; Camborieux, Laure; Guerrier, Daniel (2007). "Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome". Orphanet Journal of Rare Diseases. 2 (1): 13. doi:10.1186/1750-1172-2-13. PMC 1832178. PMID 17359527.
- "Urology Care Foundation – What is Vaginal Agenesis?". www.urologyhealth.org. Retrieved 21 January 2018.
- Stochholm, Kirstine; Juul, Svend; Gravholt, Claus H (2010). "Diagnosis and mortality in 47,XYY persons: a registry study". Orphanet Journal of Rare Diseases. 5 (1): 15. doi:10.1186/1750-1172-5-15. PMC 2889887. PMID 20509956.
- Speiser, Phyllis W.; Azziz, Ricardo; Baskin, Laurence S.; Ghizzoni, Lucia; Hensle, Terry W.; Merke, Deborah P.; Meyer-Bahlburg, Heino F. L.; Miller, Walter L.; Montori, Victor M.; Oberfield, Sharon E.; Ritzen, Martin; White, Perrin C. (September 2010). "Congenital Adrenal Hyperplasia Due to Steroid 21-Hydroxylase Deficiency: An Endocrine Society Clinical Practice Guideline". The Journal of Clinical Endocrinology & Metabolism. 95 (9): 4133–4160. doi:10.1210/jc.2009-2631. PMC 2936060. PMID 20823466.
- Tartaglia, Nicole; Ayari, Natalie; Howell, Susan; D’Epagnier, Cheryl; Zeitler, Philip (June 2011). "48,XXYY, 48,XXXY and 49,XXXXY syndromes: not just variants of Klinefelter syndrome". Acta Paediatrica. 100 (6): 851–860. doi:10.1111/j.1651-2227.2011.02235.x. PMC 3314712. PMID 21342258.
- Reference, Genetics Home. "46,XX testicular disorder of sex development". Genetics Home Reference.
- "Ovotesticular Disorder of Sex Development". NORD (National Organization for Rare Disorders).
- Yen and Jaffe's reproductive endocrinology : physiology, pathophysiology, and clinical management (7th ed.). Elsevier/Saunders. 13 September 2013. ISBN 9781455727582.
phenotypically, pure XY GD individuals are unambiguously phenotypic females (previously known as Swyer syndrome) but usually internally possess hypoplastic müllerian structures.
- Reference, Genetics Home. "Swyer syndrome". Genetics Home Reference. Retrieved 21 December 2019.
- Sinnecker, G. H. G.; Hiort, O.; Nitsche, E. M.; Holterhus, P.-M.; Kruse, K.; Group, German Collaborative Intersex Study (29 June 1996). "Functional assessment and clinical classification of androgen sensitivity in patients with mutations of the androgen receptor gene". European Journal of Pediatrics. 156 (1): 7–14. doi:10.1007/s004310050542. PMID 9007482.
- Boehmer, Annemie L. M.; Brüggenwirth, Hennie; van Assendelft, Cissy; Otten, Barto J.; Verleun-Mooijman, Marja C. T.; Niermeijer, Martinus F.; Brunner, Han G.; Rouwé, Catrienus W.; Waelkens, J. J.; Oostdijk, Wilma; Kleijer, Wim J.; van der Kwast, Theo H.; de Vroede, Monique A.; Drop, Stenvert L. S. (September 2001). "Genotype Phenotype in Families with Androgen Insensitivity Syndrome". The Journal of Clinical Endocrinology & Metabolism. 86 (9): 4151–4160. doi:10.1210/jcem.86.9.7825. PMID 11549642.
- Mosley, Michael (20 September 2015). "The extraordinary case of the Guevedoces". BBC News. BBC News. Archived from the original on 23 September 2015. Retrieved 23 September 2015.
- Imperato-McGinley, Julianne; Guerrero, Luis; Gautier, Teofilo; Peterson, Ralph Edward (December 1974). "Steroid 5alpha-reductase deficiency in man: an inherited form of male pseudohermaphroditism". Science. 186 (4170): 1213–1215. Bibcode:1974Sci...186.1213I. doi:10.1126/science.186.4170.1213. PMID 4432067.
- Kolodny, Robert C.; Masters, William H.; Johnson, Virginia E. (1979). Textbook of Sexual Medicine (1st ed.). Boston: Little, Brown and Company. ISBN 978-0-316-50154-5.
- "Intersex: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 25 March 2019.
- Diamond, Milton; Linda, Watson (2004). "Androgen insensitivity syndrome and Klinefelter's syndrome: sex and gender considerations". Child Adolesc Psychiatric Clin N Am (13). pp. 623–640. Archived from the original on 1 July 2013.
- Forrester, John (2009). "The psychology of the sexual–reproductive–gender system" (PDF). Wellcome History (42): 13–15.
- Marchal, Joseph (3 July 2010). "Bodies Bound for Circumcision and Baptism: An Intersex Critique and the Interpretation of Galatians". Theology & Sexuality. 16 (2): 163–182. doi:10.1558/tse.v16i2.163. ISSN 1355-8358.
- García López, Daniel J (March 2015). "La intersexualidad en el discurso médico-jurídico". Eunomía. 0 (8): 54–70. ISSN 2253-6655.
- Baylis, Françoise; Borgerson, Kirstin; Hoffmaster, Barry; Sherwin, Susan (6 October 2011). Health Care Ethics in Canada. Cengage Learning. ISBN 9780176504649.
- Kamijo, H.; Narita, O. (November 1997). "[Female pseudohermaphroditism]". Nihon Rinsho. Japanese Journal of Clinical Medicine. 55 (11): 2925–2929. ISSN 0047-1852. PMID 9396289.
- Migeon, C. J. (July 1980). "Male pseudohermaphroditism". Annales d'Endocrinologie. 41 (4): 311–343. ISSN 0003-4266. PMID 7011168.
- Fernández-Cancio, Mónica; Camats, Núria; Flück, Christa E.; Zalewski, Adam; Dick, Bernhard; Frey, Brigitte M.; Monné, Raquel; Torán, Núria; Audí, Laura (29 April 2018). "Mechanism of the Dual Activities of Human CYP17A1 and Binding to Anti-Prostate Cancer Drug Abiraterone Revealed by a Novel V366M Mutation Causing 17,20 Lyase Deficiency". Pharmaceuticals. 11 (2): 37. doi:10.3390/ph11020037. PMC 6027421. PMID 29710837.
- Iqbal, Muhammad Zafar; Jam, Mazhar Rafee; Saleem, Muhammad; Ahmad, Mushtaq (30 July 2011). "True Hermaphrodite: A Case Report". APSP Journal of Case Reports. 2 (2): 16. ISSN 2218-8185. PMC 3418019. PMID 22953283.
- Dreger, Alice; Ellen K. Feder; Anne Tamar-Mattis (30 July 2012). "Prenatal Dexamethasone for Congenital Adrenal Hyperplasia". Journal of Bioethical Inquiry. 9 (3): 277–294. doi:10.1007/s11673-012-9384-9. PMC 3416978. PMID 22904609.
- Fernández-Balsells, M.M.; K. Muthusamy; G. Smushkin; et al. (2010). "Prenatal dexamethasone use for the prevention of virilization in pregnancies at risk for classical congenital adrenal hyperplasia because of 21-hydroxylase (CYP21A2) deficiency: A systematic review and meta-analyses". Clinical Endocrinology. 73 (4): 436–444. doi:10.1111/j.1365-2265.2010.03826.x. PMID 20550539.
- "eMedicine article on 5-ARD". Emedicine.com. 23 June 2009. Archived from the original on 17 October 2008. Retrieved 21 August 2009.
- De Marchi M, Carbonara AO, Carozzi F, et al. (1976). "True hermaphroditism with XX/XY sex chromosome mosaicism: report of a case". Clin. Genet. 10 (5): 265–72. doi:10.1111/j.1399-0004.1976.tb00047.x. PMID 991437.
- "ovo-testes (formerly called "true hermaphroditism")". Intersex Society of North America. Archived from the original on 4 January 2008. Retrieved 9 December 2007.
- Weil, Elizabeth (September 2006). What if It's (Sort of) a Boy and (Sort of) a Girl? Archived 16 February 2017 at the Wayback Machine The New York Times Magazine.
- Lee, Peter A.; Nordenström, Anna; Houk, Christopher P.; Ahmed, S. Faisal; Auchus, Richard; Baratz, Arlene; Baratz Dalke, Katharine; Liao, Lih-Mei; Lin-Su, Karen; Looijenga, Leendert H.J.; Mazur, Tom; Meyer-Bahlburg, Heino F.L.; Mouriquand, Pierre; Quigley, Charmian A.; Sandberg, David E.; Vilain, Eric; Witchel, Selma; and the Global DSD Update Consortium (28 January 2016). "Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care". Hormone Research in Paediatrics. 85 (3): 158–180. doi:10.1159/000442975. ISSN 1663-2818. PMID 26820577.
- Mouriquand, Pierre D. E.; Gorduza, Daniela Brindusa; Gay, Claire-Lise; Meyer-Bahlburg, Heino F. L.; Baker, Linda; Baskin, Laurence S.; Bouvattier, Claire; Braga, Luis H.; Caldamone, Anthony C.; Duranteau, Lise; El Ghoneimi, Alaa; Hensle, Terry W.; Hoebeke, Piet; Kaefer, Martin; Kalfa, Nicolas; Kolon, Thomas F.; Manzoni, Gianantonio; Mure, Pierre-Yves; Nordenskjöld, Agneta; Pippi Salle, J. L.; Poppas, Dix Phillip; Ransley, Philip G.; Rink, Richard C.; Rodrigo, Romao; Sann, Léon; Schober, Justine; Sibai, Hisham; Wisniewski, Amy; Wolffenbuttel, Katja P.; Lee, Peter (2016). "Surgery in disorders of sex development (DSD) with a gender issue: If (why), when, and how?". Journal of Pediatric Urology. 12 (3): 139–149. doi:10.1016/j.jpurol.2016.04.001. ISSN 1477-5131. PMID 27132944.
- Creighton, Sarah M.; Michala, Lina; Mushtaq, Imran; Yaron, Michal (2 January 2014). "Childhood surgery for ambiguous genitalia: glimpses of practice changes or more of the same?" (PDF). Psychology and Sexuality. 5 (1): 34–43. doi:10.1080/19419899.2013.831214. ISSN 1941-9899.
- Comisión Interamericana de Derechos Humanos (12 November 2015), Violencia contra Personas Lesbianas, Gays, Bisexuales, Trans e Intersex en América (PDF), Comisión Interamericana de Derechos Humanos, archived (PDF) from the original on 7 January 2016
- German Ethics Council (February 2012). Intersexuality, Opinion. ISBN 978-3-941957-50-3. Archived from the original on 21 April 2017. Retrieved 25 January 2020.
- Cools, Martine; Koen van Aerde; Anne-Marie Kersemaekers; Marjan Boter; Stenvert L. S Drop; Katja P. Wolffenbuttel; Ewout W. Steyerberg; J. Wolter Oosterhuis; Leendert H. J. Looijenga (September 2005). "Morphological and Immunohistochemical Differences between Gonadal Maturation Delay and Early Germ Cell Neoplasia in Patients with Undervirilization Syndromes". J. Clin. Endocrinol. Metab. 90 (9): 5295–5303. doi:10.1210/jc.2005-0139. PMID 15998778.
- Intersex Society of North America (24 May 2006). What evidence is there that you can grow up psychologically healthy with intersex genitals (without "normalizing" surgeries)? Archived 8 December 2006 at the Wayback Machine. Retrieved 25 November 2006.
- Bioethics Forum blog – Preventing Homosexuality (and Uppity Women) in the Womb? Archived 2 April 2016 at the Wayback Machine, Alice Dreger, Ellen K. Feder, Anne Tamar-Mattis (2010), at Hastings Center Bioethics Blog, retrieved 18 May 2012.
- What Causes Low Rates of Child-Bearing in Congenital Adrenal Hyperplasia?, H. F. L. Meyer-Bahlburg (1999), in The Journal of Clinical Endocrinology & Metabolism, Volume 84 Issue 6 | 1 June 1999, retrieved 18 May 2012.
- Meyer-Bahlburg, HFL (1990). "Will prenatal hormone treatment prevent homosexuality?". Journal of Child and Adolescent Psychopharmacology. 1 (4): 279–283. doi:10.1089/cap.1990.1.279.
- "American Journal of Bioethics, 13:10, 51–53. Retrieved 11 September 2013". Archived from the original on 11 October 2014. Retrieved 6 October 2014.
- Preves, Sharon (2003). Intersex and Identity, the Contested Self. Rutgers. ISBN 0-8135-3229-9. p. 72.
- Creighton, Sarah; Alderson, J; Brown, S; Minto, Cathy (2002). "Medical photography: ethics, consent and the intersex patient". BJU International. 89: 67–71. doi:10.1046/j.1464-410X.2002.02558.x. p. 70.
- Dreger, Alice Domurat (2000). "Jarring Bodies: Thoughts on the Display of Unusual Anatomies". Perspectives in Biology and Medicine. 43 (2): 161–172. doi:10.1353/pbm.2000.0002. ISSN 1529-8795. PMID 10804583.
- Kraus, Cynthia (May 2015). "Classifying Intersex in DSM-5: Critical Reflections on Gender Dysphoria". Archives of Sexual Behavior. 44 (5): 1147–1163. doi:10.1007/s10508-015-0550-0. ISSN 0004-0002. PMID 25944182.
Bibliography
- Asia Pacific Forum of National Human Rights Institutions (June 2016). Promoting and Protecting Human Rights in relation to Sexual Orientation, Gender Identity and Sex Characteristics. ISBN 978-0-9942513-7-4.
- Blackless, Melanie; Charuvastra, Anthony; Derryck, Amanda; Fausto-Sterling, Anne; Lauzanne, Karl; Lee, Ellen (2000). "How sexually dimorphic are we? Review and synthesis". Am J Hum Biol. 12 (2): 151–166. doi:10.1002/(SICI)1520-6300(200003/04)12:2<151::AID-AJHB1>3.0.CO;2-F. PMID 11534012.
- Council of Europe; Commissioner for Human Rights (April 2015), Human rights and intersex people, Issue Paper
- Davis, Georgiann (2015). Contesting Intersex, The Dubious Diagnosis. NYU Press. New York. ISBN 978-1-4798-3786-1.
- Elders, M Joycelyn; Satcher, David; Carmona, Richard (June 2017). "Re-Thinking Genital Surgeries on Intersex Infants" (PDF). Palm Center.
- Fausto-Sterling, Anne (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. Basic Books. ISBN 978-0-465-07714-4.
- Ghattas, Dan Christian; Heinrich-Böll-Stiftung (2013). Human Rights between the Sexes: A preliminary study on the life situations of inter*individuals. Berlin: Heinrich-Böll-Stiftung. ISBN 978-3-86928-107-0.
- Holmes, Morgan, ed. (2009). Critical intersex. Ashgate Publishing. Queer interventions. Burlington, VT. ISBN 978-0-7546-7311-8.
- Hughes, I A; Houk, C; Ahmed, S F; Lee, P A; LWPES1/ESPE2 Consensus Group (June 2005). "Consensus statement on management of intersex disorders". Archives of Disease in Childhood. 91 (7): 554–563. doi:10.1136/adc.2006.098319. ISSN 0003-9888. PMC 2082839. PMID 16624884.
- Human Rights Commission of the City and County of San Francisco; de María Arana, Marcus (2005). A Human Rights Investigation Into The Medical "Normalization" Of Intersex People. San Francisco.
- Human Rights Watch; interACT (July 2017). I Want to Be Like Nature Made Me. ISBN 978-1-62313-502-7.
- Jones, Tiffany; Hart, Bonnie; Carpenter, Morgan; Ansara, Gavi; Leonard, William; Lucke, Jayne (2016). Intersex: Stories and Statistics from Australia (PDF). Cambridge, UK: Open Book Publishers. ISBN 978-1-78374-208-0. Archived from the original (PDF) on 27 May 2018. Retrieved 2 February 2016.
- Jones, Tiffany (2018). "Intersex Studies: A Systematic Review of International Health Literature". Sage Open. 2018 (1): 1–22. doi:10.1177/2158244017745577.
- Karkazis, Katrina (2008). Fixing Sex: Intersex, Medical Authority, and Lived Experience. Duke University Press. ISBN 978-0-8223-4318-9.
- Lee, Peter A.; Nordenström, Anna; Houk, Christopher P.; Ahmed, S. Faisal; Auchus, Richard; Baratz, Arlene; Baratz Dalke, Katharine; Liao, Lih-Mei; Lin-Su, Karen; Looijenga, Leendert H.J.; Mazur, Tom; Meyer-Bahlburg, Heino F.L.; Mouriquand, Pierre; Quigley, Charmian A.; Sandberg, David E.; Vilain, Eric; Witchel, Selma; and the Global DSD Update Consortium (28 January 2016). "Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care". Hormone Research in Paediatrics. 85 (3): 158–180. doi:10.1159/000442975. ISSN 1663-2818. PMID 26820577.
- National Advisory Commission on Biomedical Ethics, Switzerland (November 2012). On the management of differences of sex development. Ethical issues relating to "intersexuality".Opinion No. 20/2012 (PDF). 2012. Berne. Archived from the original (PDF) on 23 April 2015. Retrieved 20 October 2018.
- Organisation Intersex International Australia; Carpenter, Morgan (April 2014). "Submission on the Review of Part B of the Ethical Guidelines for the Use of Assisted Reproductive Technology in Clinical Practice and Research, 2007". Sydney.
- Regmi, Esan (2016). Stories of Intersex People from Nepal. Kathmandu.
- Senate of Australia; Community Affairs References Committee (2013). Involuntary or coerced sterilisation of intersex people in Australia. Canberra. ISBN 978-1-74229-917-4.
- Tamar-Mattis, Anne (2014). "Medical Treatment of People with Intersex Conditions as Torture and Cruel, Inhuman, or Degrading Treatment or Punishment". In Center for Human Rights & Humanitarian Law; Washington College of Law (eds.). Torture in Healthcare Settings: Reflections on the Special Rapporteur on Torture's 2013 Thematic Report. Washington, DC. pp. 91–104.
- United Nations Office of the High Commissioner for Human Rights (2015). "Free & Equal Campaign Fact Sheet: Intersex" (PDF).
- UN Committee against Torture; UN Committee on the Rights of the Child; UN Committee on the Rights of People with Disabilities; UN Subcommittee on Prevention of Torture and other Cruel, Inhuman or Degrading Treatment or Punishment; Juan Méndez; Dainius Pῡras; Dubravka Šimonoviæ; Marta Santos Pais; African Commission on Human and Peoples' Rights; Council of Europe Commissioner for Human Rights; Inter-American Commission on Human Rights (24 October 2016), "Intersex Awareness Day – Wednesday 26 October. End violence and harmful medical practices on intersex children and adults, UN and regional experts urge", Office of the High Commissioner for Human Rights
- World Health Organization; OHCHR; UN Women; UNAIDS; UNDP; UNFPA; UNICEF (2014). Eliminating forced, coercive and otherwise involuntary sterilization, An interagency statement (PDF). ISBN 978-92-4-150732-5.
- Zwischengeschlecht (March 2014). "IGM – Historical Overview. Hermaphrodites in the 'Developed World': From Legal Self-Determination to IGM, Supplement 1" (PDF). NGO Report to the 2nd, 3rd and 4th Periodic Report of Switzerland on the Convention on the Rights of the Child (CRC) (2 ed.). pp. 49–62.
External links
![]()