Dental public health
Dental Public Health (DPH) is a non-clinical specialty of dentistry that deals with the prevention of oral disease and promotion of oral health.[1][2] Dental public health is involved in the assessment of key dental health needs and coming up with effective solutions to improve the dental health of populations rather than individuals.[3]
Prevention is becoming increasingly important. Dental related diseases are largely preventable and there is a growing burden on health care systems for cure. Dental public health looks beyond the role of a dental practitioner in treating dental disease, and seeks to reduce demand on health care systems by redirection of resources to priority areas.[4] Countries around the world all face similar issues in relation to dental disease. Implementation of policies and principles vary due to available of resources. Similar to public health, an understanding of the many factors that influence health will assist the implementation of effective strategies.[4]
Public health dentistry, is practiced generally through government sponsored programs, which are for the most part directed toward public-school children in the belief that their education in oral hygiene is the best way to reach the general public. The pattern for such programs in the past was a dental practitioners annual visit to a school to lecture and to demonstrate proper tooth-brushing techniques. The 1970s saw the emergence of a more elaborate program that included a week of one-hour sessions of instruction, demonstration, and questions and answers, conducted by a dentist and a dental assistant and aided by a teacher who had previously been given several hours of instruction. Use was also made of televised dental health education programs, which parents were encouraged to observe.[5]
Background
There seems to be a lot more that can be done to help individuals prevent tooth decay and gum disease based on what is already known.
Even with fluoridation and oral hygiene, tooth decay is still the most common diet–related disease affecting many people. Tooth decay has the economic impact of heart disease, obesity and diabetes.[6]
Dental decay is however easily prevented by reducing acid demineralisation caused by the remaining dental plaque left on teeth after brushing. Risk factors for tooth decay include physical, biological, environmental, behavioural, and lifestyle-related factors such as high numbers of cariogenic bacteria, inadequate salivary flow, insufficient fluoride exposure, poor oral hygiene, inappropriate methods of feeding infants, and poverty.[7] Neutralising acids after eating and at least twice a day brushing with fluoridated toothpaste will assist prevention.
Cavities can develop on any surface of a tooth, but are most common inside the pits and fissures in grooves on chewing surfaces. This is where the toothbrush bristles and fluoride toothpaste cannot reach effectively.[8]
Gum diseases gingivitis and periodontitis are caused by certain types of bacteria that accumulate in remaining dental plaque. The extent of gum disease depends a lot on host susceptibility.[9]
Daily brushing must include brushing of both the teeth and gums. Effective brushing itself, will prevent progression of both dental decay and gum diseases. Neutralising acids after eating and at least twice a day brushing with fluoridated toothpaste will assist preventing dental decay. Stimulating saliva flow assists in the remineralisation process of teeth, this can be done by chewing sugar free gum.[7] Using an interdental device once daily will assist prevention of gum diseases.[9]
Fissure sealants applied over the chewing surfaces of teeth, block plaque from being trapped inside pits and fissures. The sealants make brushing more effective and prevent acid demineralisation and tooth decay.[10] A diet low in fermentable carbohydrates will reduce the buildup of plaque on teeth.[7]
Current practice
Competencies
The American Board of Dental Public Health (ABDPH) have devised a list of competencies for dental public health specialists to follow.[11] Dental public health specialists are a select group of certified dentists. The 10 competencies allow for growth and learning of individuals and set expectations for the future. An advantage of the design is that they are implementable on a global level. The list is updated periodically.[11]
| 1998 competencies | New competencies |
|---|---|
| 1. Plan oral health programs for populations | 1. Manage oral health programs for population health |
| 2. Select interventions and strategies for the prevention and control of oral diseases and promotion of oral health | 2. Demonstrate ethical decision-making in the practice of dental public health |
| 3. Develop resources, implement and manage oral health programs for populations | 3. Evaluate systems of care that impact oral health |
| 4. Incorporate ethical standards in oral health programs and activities | 4. Design surveillance systems to measure oral health status and its determinants |
| 5. Evaluate and monitor dental care delivery systems | 5. Communicate on oral and public health issues |
| 6. Design and understand the use of surveillance systems to monitor oral health | 6. Lead collaborations on oral and public health issues |
| 7. Communicate and collaborate with groups and individuals on oral health issues | 7. Advocate for public health policy, legislation, and regulations to protect and promote the public's oral health, and overall health |
| 8. Advocate for public health policy, legislation, and regulations to protect and promote the public's oral health, and overall health | 8. Critically appraise evidence to address oral health issues for individuals and populations |
| 9. Critique and synthesize scientific literature | 9. Conduct research to address oral and public health problems |
| 10. Design and conduct population-based studies to answer oral and public health questions | 10. Integrate the social determinants of health into dental health practice |
Scope
Major areas of dental public health activity include:
- Oral health surveillance
National Oral Health Surveillance system (NOHSS) is designed to monitor the effects of oral disease on the population, as well as monitor how the oral care is delivered. Additionally the status of water fluoridation on both a state and a national level is continually supervised [12]
- Assessing the evidence on oral health and dental interventions, programmes, and services
- Policy and strategy development and implementation
- Oral health improvement
- Health and public protection
- Developing and monitoring quality dental services
- Dental public health intelligence
- Academic dental public health
- Role within health services
Principles
Dental health is concerned with promoting health of an entire population and focuses on an action at a community level, rather than at an individual clinical approach. Dental public health is a broad subject that seeks to expand the range of factors that influences peoples oral health and the most effective means of preventing and treating these oral health problems.[4]
Criteria to determine a public health problem
To allow a health problem to be properly managed, it is important that there is a set of rules or criteria to follow which determines what is defined as a public health problem and what is the best way to manage health problems in communities. The following are questions should be considered when addressing public health problems:
| What is the prevalence of the condition? |
|---|
| What is the prevalence of the health problem? |
| Is the disease widespread? |
| Who has the disease? |
| What percentage of the population is affected? |
| What is the distribution of the disease within the community? |
| Is the prevalence increasing or decreasing? |
| What is the impact of the condition on an individual level? |
|---|
| How severe are the effects of the disease on the patient? |
| Do people die because of it? |
| Do they suffer pain, discomfort or loss of function? |
| Can they perform their normal social roles? |
| Are they prevented from going to school or becoming employed because of their problem? |
| What is the impact on the wider society? |
|---|
| What are the costs to the health service of treating the condition? |
| How much time do people take off work to get treatment and care? |
| What effects does the condition have on economic performance and productivity of the country? |
| What conditions are preventable and effective treatments available? |
|---|
| Is the natural history of the disease fully understood? |
| Can the early stages of the conditions be recognised? |
| If so, are there interventions that can be implemented to stop the disease progressing? |
| If it does progress, are there effective treatments available? |
Once these questions have been answered, the way a public health problem is acted upon to protect a population can be determined.
Approaches to prevention
Fluoridation of drinking water
Water fluoridation is the implementation of artificial fluoride in public water supplies with the intentions to halt the progression of dental diseases.[14] Fluoride has the ability to interfere with the demineralisation and remineralisation process that occurs on the tooth surface and improves the mineral intake when the pH level may reduce below the neutral pH level.[15]
This achievement was implemented through the public health development in the 19th, 20th century and led into the 21st century. Research into the effects of fluoride on teeth began due to the concern about the presence of dental fluorosis.[16]
Many clinical case trials occurred in the beginning of the 20th century. However, the very first clinical trial to have occurred dates back to the 19th century when Denninger conducted a trial prescribing children and pregnant women with calcium fluoride.[15] From this trial it was recognised fluoride’s significance on tooth tissue and from this point, many clinical trials were conducted [14] Following these studies, the recognition of the positive outcome on dental tissues became clear and projects in water fluoridation became of significant importance.
The development of artificial water fluoridation began in 1945 in the Grand rapid Michigan followed by Newburgh, New York and Evanston, Illinois.[17] In 1955 three towns Watford, Kilmarnock and Anglesey trialled the water fluoridation implementation scheme.[14] In 1960 the Republic of Ireland implemented all public water supplies with artificial fluoridated water and four years later extending this into the main cities of Dublin and Cork.[14]
Currently, 40 countries have fluoridated water schemes implemented. Fluoride is still yet to be completely implemented across the full population however, progress is slowly improving and access is becoming more common.[14]

| Country | Population with fluoridated water |
|---|---|
| Argentina | 21% |
| Australia | 61% |
| Brazil | 41% |
| Canada | 43% |
| Chile | 40% |
| Columbia | 80% |
| Hong Kong | 100% |
| Israel | 75% |
| Malaysia | 70% |
| New Zealand | 61% |
| Panama | 18% |
| Republic of Ireland | 73% |
| Singapore | 100% |
| Spain | 10% |
| United Kingdom | 10% |
| United States | 74.4% [18] |
Career opportunities focusing on prevention
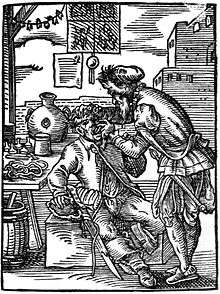
Prevention methods such as oral health promotion began with the education of clinicians and the population in the health promotion strategies. Since the mid 19th century oral health practice has revolved more around prevention and education rather than treatment of disease.[19] This education can be focused towards dental practitioners and to the wider population who may interested.
There has been a change in focus in the education of developing clinicians all over the world. The first dental school was developed in 1828 [20] and was followed by an ever-growing field of practice. The dental practice began with its main focus on the treatment of oral disease and branched into a wide scope of practice with many dental occupations involved.
The most common form of dental clinicians are either general dentists, oral health therapists, dental therapists and dental hygienist. When desired, some of these clinicians may seek further experience in projects that may assist the dental public system in bringing further awareness to prevention of dental diseases.[21]
Oral health prevention is the current form of practice of many clinicians. As education in oral care to the population is now believed to be the superior solution rather than the treatment of disease. Dental university education now develops clinicians to focus on the education of patients, education of the community and a wider population using different approaches.[19]
Approaches to promotion
Oral Health Promotion outlines the strategies for improving and educating the general public about how they can better take improve and maintain their current oral health. Oral health promotion is part of both government and private incentives to create a healthier and better educated generation of individuals.[22]
These are the nine key principles involved for oral health promotion: [23]
| Empowerment | Individuals, groups and communities are given the ability to exercise more control over the personal, socioeconomics, and environmental factors through interventions that affect their oral health. |
| Participatory | Key stakeholders that are invested in the intervention program should be actively participating in the stages of planning, implementing and evaluating interventions. |
| Holistic | Common risks and conditions of oral health, general health and inequalities should be taken into consideration of a broad intervention approach. |
| Inter-sectoral | Collaboration between all relevant agencies and sectors is paramount as it allows oral health improvement to be implemented upon the wider public health agenda. |
| Equity | It is important to place an emphasis on Oral health inequalities when planning interventions for oral health improvement. |
| Evidence base | Future interventions of oral health improvement should be implemented through existing knowledge of effectiveness and good practice of oral health. |
| Sustainable | The measures of whether individuals, groups and communities of achieving long-term oral health improvement can be maintained. |
| Multi-strategy | It is imperative to perform a range of complementary actions such as health public policies, community development and environmental change in order to address the underlying determinants of oral health. |
| Evaluation | Adequate resources in conjunction with suitable methods should be present for effective assessment of oral health interventions. |
There are three important way in achieving oral health promotion, which is done by addressing the determinants of oral health, community participation, and implementing a strategy approach that involves a range of complementary actions.[23]
Determinants of oral health
Oral health promotion focuses on individual behaviour, the Socioeconomic status and environmental factors. Underlying determinants that can also impact oral health, including non-milk extrinsic sugars consumption, alcohol consumption and smoking behaviour.[23]
The ability to remove dental plaque, exposure to fluoride and access to quality dental care can affect the ways the aforementioned underlying factors are and can be modified to the needs of the individual to obtain optimum oral health.[23] Ways in which oral health promotion can minimise the effects of these determinants;
- Promoting healthy eating.
- Teaching effective oral hygiene practices.
- Promoting the use of topical fluoride for preventing and control of dental caries.
- Facilitating early access to preventative dental services.[24]
It is also important to note that these factors are also influenced by socio-political considerations that are outside the control of most individuals.[23]
Community participation is a key factor in oral health promotion. Inter-sectoral collaboration is where relevant agencies and sectors are involved in partnership to identify key oral health issues and to implement new methods to improve oral health.[23]
The World Health Organization has agreed on a health promotion approach as the foundation for oral health improvement strategies and policies for the population. Oral health promotion is based on the principles of the framework, Ottawa Charter. There are five areas of action outlined to achieve oral health promotion; building Health public policy, creating supportive environment, strengthening community action, developing personal skills, re-orienting healthcare services.[22]
Research studies on dental public health issues
Oral health in care homes
A study investigating the efficacy of staff workers' oral care education on improving the oral health of care home residents found that despite the education and training of care workers, certain ongoing barriers prevented them from conducting the necessary daily oral hygiene care for the residents. The most frequently listed obstacles to care included the residents' bad breath, inadequate time to perform oral care and uncooperative residents who do not perceive the need for oral care.[25]
Another study on the effects of oral health educational interventions for nursing home staff or residents, or both, to maintain or improve the oral health for nursing home residents shows insufficient supporting evidence.[26]
School dental screening programs
Researchers have concluded that it is unclear whether or not school screening programs improve attendance at the dentist. School screening initiatives with incentives attached, such as free treatment, may be helpful in improving oral health of children.[27]
One-to-one oral hygiene advice provided in a dental setting for oral health
One-to-one oral hygiene advice (OHA) is often given on a regular basis to motivate individuals and to improve one's oral health. However, it is still unclear if one-to-one OHA in a dental settings is effective in improving one's oral health.[28]
Examples
Australia
Child Dental Benefits Schedule (CDBS)
- A Government funded program which provides assistance for basic dental services for children aged 2–17 years. Services provided include: examinations, dental x-rays, cleaning, fissure sealants, fillings, extractions and root canals
- The CDBS is means tested, those who qualify are eligible to $1,000 of the aforementioned treatments over a two-year period.[29]
To find out if a child is eligible, families can contact the Department of Human Services [29]
National Partnership Agreement on Adult Public Dental Services
- As part of the National Partnership Agreement on Adult Public Dental Services, between 2015- 2016 $155 million was provided to service around 178,000 adult public patients
- On 15 December 2016, a further $320 million was provided by the Australian Government for dental services to public adult patients; the funding is to last for three years.[29]
Autonomous Region of Madeira - Portugal
In 1985 three dentists with the sponsorship of Colonel Joy Wheeler Dow, Jr., implemented an Oral Health Program in the Autonomous Region of Madeira with the aid of five assistants.
The four-year program reached 15,000 children around the main island and Porto Santo and it included Oral Hygiene Instruction classes, informative literature including films, fortnightly fluoride mouth-rinse and daily fluoride tables with the collaboration of the school teachers.
During this period a study was undertaken using the World Health Organization (WHO) Combined Oral Health Assessment (CPTIN) plan resulting in the final report where it was found that there had been a decrease of 44% in the need for fillings, 40% decrease in the need for extractions, whilst the caries free children population grew from the initial 1% to 5%.
United Kingdom
National Health Service (NHS) dentistry
National Health Service (NHS) is the name of the public health services of England, Scotland and Wales and is directly funded from taxation. The dentistry services are available to all, regardless of wealth. In order to find a NHS dentist search NHS Dentist Near You Some clinics may not have the capacity to take on new patients so waiting lists may occur.[30]
- Availability of treatment
All treatment deemed necessary to maintain optimal oral health will be provided by the dentist, however not all treatments will be funded by the Dentistry NHS and will incur private fees.[30]
- Fee's
Dentistry performed under the Dentistry NHS will involve fees, however are heavily subsidized by the government, below is some information which explains how the fee’s system works, only one charge is required per treatment course of care, regardless of the amount of appointments needed [30]
| Course of Care | Fee | Treatment involved |
|---|---|---|
| Emergency | £20.60 | This only covers treatment involving pain on a specific tooth |
| Band 1 | £20.60 | This covers the most basic care including examination, x-rays and if needed scale and polish, fissure sealants and fluoride application |
| Band 2 | £56.30 | This band covers all the above and any further restorative treatment, including restorations, root canals and also extractions |
| Band 3 | £244.30 | If all the above treatment is deemed necessary, along with any other laboratory work, including crowns, bridges and dentures |
Nepal
Nepalese population is at a greater disadvantage than westernized societies in terms of oral health. The benefit of implementing health insurance is to assist a large number of people with similar risks by sharing funding.[31] In Nepal, implementing health insurance is difficult due to limited supply of finances. To assist families with accessing health care “elimination of direct payments is necessary but is not sufficient alone; costs of transportation and loss of income can have more impact than direct payment of services” must be considered.[31]
Education

- The amount of dental professionals produced from tertiary education has increased in Nepal over the years, but remains low in comparison to the rest of the world. There were approximately only 100 dentists in the workforce in the year 2000, which has increased to 240 in the present.[32]
- Nepal is now using dental hygienists, therapists and oral health therapists to increase access to dental treatment.[33]
- Programs such as training rural women about oral health promotion are being utilized to increase awareness of basic dental problems in remote areas.[34]
Dental outreach program
- Attempts to reduce the gap in dental health of Nepalese people through volunteer work provides oral health care education and basic treatment to small villages.
- Services provided include oral hygiene instruction, distribution of free toothbrush and fluoride toothpaste, application of fluoride gel, application of sealant, screening and charting out treatment plan under a supervising dentist, scaling, filling, extraction, prescribing medicine, and free dispensing distributing medicines
For more information, you can access the Around Good People fact sheet
Early history
The earliest known person identified as a dental practitioner dates back to 2600BC, an Egyptian scribe states that he was ‘the greatest of those who deal with teeth ad of physicians’
- 1500BC- Egyptian Ebers papyrus explains oral disease and offers prescription for strengthening teeth and gums
- 9th century AD- The Arabs discussed the care of teeth rather than extractions and replacement. Mouth hygiene was established with a small wooden stick
- Late 1400s- The first tooth brush was invented by the Chinese
- 1723- A French surgeon describes a comprehensive care system for dentistry including restorative techniques and denture reconstruction
- 1791- The first dental treatment available for the poor, established in New York City
- 1840- The world's first national dental organisation was founded
- 1861- Philadelphian charity hospital offers dental services
- 1865- First ever children’s dental clinic, established in Germany
- 1867- Boston opened its first low income dental clinic
- 1884- The term Oral Hygiene come about when ML Rhein asks dentists to teach patients how to brush their teeth
- 1890- A committee in England carried out oral hygiene promotion in schools
- 1989- The powerful slogan ‘A clean tooth never decays’ helps improves standards of mouth hygiene
- 1931- Fluoride is identified
- 1945- First ever water fluoridation
- 1969- World Health Organization (WHO) establishes a data bank which collect information on dental health and needs
- 1996- WHO Oral Health Country/Area Profile Program (CAPP) is established, this online database presents information on individual countries oral health services and oral disease rates
See also
References
- "Dental public health". NHS careers.
- "Residency Program". School of Dental Medicine. CWRU School of Dental Medicine. 2017. Archived from the original on 2016-08-13.
- "Public Health Dental Program". Florida Department of Health. 2017.
- Daly B, Batchelor P, Treasure E, Watt R (2013). Essential Dental Public Health (2nd ed.). Great Britain: Oxford University Press.
- Tyack D. Health and social services in public schools: Historical perspectives. The Future of Children. 2017.
- Listl S, Galloway J, Mossey PA, Marcenes W (October 2015). "Global Economic Impact of Dental Diseases". Journal of Dental Research. 94 (10): 1355–61. doi:10.1177/0022034515602879. PMID 26318590.
- Selwitz RH, Ismail AI, Pitts NB (January 2007). "Dental caries". Lancet. 369 (9555): 51–9. doi:10.1016/S0140-6736(07)60031-2. PMID 17208642.
- Kluss R (2015). "What Causes Tooth Decay?". Absolute Smile.
- Axelsson P, Lindhe J (May 1978). "Effect of controlled oral hygiene procedures on caries and periodontal disease in adults". Journal of Clinical Periodontology. 5 (2): 133–51. doi:10.1111/j.1600-051x.1978.tb01914.x. PMID 275282.
- Beauchamp J, Caufield PW, Crall JJ, Donly K, Feigal R, Gooch B, et al. (March 2008). "Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs". Journal of the American Dental Association. 139 (3): 257–68. doi:10.14219/jada.archive.2008.0155. PMID 18310730.
- Altman D, Mascarenhas AK (September 2016). "New competencies for the 21st century dental public health specialist". Journal of Public Health Dentistry. 76 Suppl 1: S18–S28. doi:10.1111/jphd.12190. PMID 27990679.
- "National Oral Health Surveillance System (NOHSS)". United State Centers for Disease Control and Prevention. 2017.
- Gulliford M, Tan CC, Karim QA, eds. (February 2015). Oxford Textbook of Global Public Health. USA: Oxford University Press.
- Mullen J (October 2005). "History of water fluoridation". British Dental Journal. 199 (7 Suppl): 1–4. doi:10.1038/sj.bdj.4812863. PMID 16215546.
- Fejerskov O, Nyvad B, Kidd E (2015). Dental Caries (1st ed.). Chichester, West Sussex: Wiley Blackwell.
- Capper S (2007). "Book Review: Silent Victories: The History and Practice of Public Health in Twentieth-Century America". Inquiry. 44 (1): 128–129. doi:10.5034/inquiryjrnl_44.1.128.
- Lennon MA (September 2006). "One in a million: the first community trial of water fluoridation". Bulletin of the World Health Organization. 84 (9): 759–60. doi:10.2471/blt.05.028209. PMC 2627472. PMID 17128347.
- "2014 Water Fluoridation Statistics, Community Water Fluoridation". Oral Health. United States Centers for Disease Control and Prevention. 2017.
- Satur J (2005). "The development of the dental therapy profession". The Australian Dental and Oral Health Therapists.
- Owen LK, ed. (1999). Dictionary of Ohio Historic Places. 2. Somerset: St. Clair Shores. pp. 1217–1218.
- "Dental Hygienist". Ada.org. 2017.
- "Milestones in Health Promotion Statements from Global Conferences" (PDF). World Health Organization (WHO). 2009.
- Daly B, Batchelor P, Treasure E, Watt R (2017). Essential Dental Public Health (2nd ed.). Great Britain: Oxford University Press. p. 102. ISBN 978-0-19-967937-9.
- Ministry of Health. Promoting Oral Health A toolkit to assist the development, planning, implementation and evaluation of oral health promotion in New Zealand. New Zealand: Ministry of Health; 2017.
- Le P, Dempster L, Limeback H, Locker D (November 2012). "Improving residents' oral health through staff education in nursing homes". Special Care in Dentistry. 32 (6): 242–50. doi:10.1111/j.1754-4505.2012.00279.x. PMID 23095067.
- Albrecht M, Kupfer R, Reissmann DR, Mühlhauser I, Köpke S, et al. (Cochrane Oral Health Group) (September 2016). "Oral health educational interventions for nursing home staff and residents". The Cochrane Database of Systematic Reviews. 9: CD010535. doi:10.1002/14651858.CD010535.pub2. PMC 6457754. PMID 27689868.
- Arora, Ankita; Khattri, Shivi; Ismail, Noorliza Mastura; Kumbargere Nagraj, Sumanth; Prashanti, Eachempati (21 December 2017). "School dental screening programmes for oral health". The Cochrane Database of Systematic Reviews. 12: CD012595. doi:10.1002/14651858.CD012595.pub2. ISSN 1469-493X. PMC 6485978. PMID 29267989.
- Soldani FA, Lamont T, Jones K, Young L, Walsh T, Lala R, Clarkson JE, et al. (Cochrane Oral Health Group) (October 2018). "One-to-one oral hygiene advice provided in a dental setting for oral health". The Cochrane Database of Systematic Reviews. 10: CD007447. doi:10.1002/14651858.CD007447.pub2. PMC 6516798. PMID 30380139.
- "Department of Health". 2017.
- "Help with health costs". England: National Health Servies. 2017.
- Knevel R, Gussy MG, Farmer J, Karimi L (August 2017). "Perception of Nepalese dental hygiene and dentistry students towards the dental hygienists profession". International Journal of Dental Hygiene. 15 (3): 219–228. doi:10.1111/idh.12192. PMID 26756212.
- Knevel RJ, Gussy MG, Farmer J, Karimi L (December 2015). "Nepalese dental hygiene and dental students' career choice motivation and plans after graduation: a descriptive cross-sectional comparison". BMC Medical Education. 15: 219. doi:10.1186/s12909-015-0500-5. PMC 4676855. PMID 26655045.
- Knevel RJ, Luciak-Donsberger C (February 2009). "Dental hygiene education in Nepal". International Journal of Dental Hygiene. 7 (1): 3–9. doi:10.1111/j.1601-5037.2008.00338.x. PMID 19215305.
- Knevel RJ (November 2010). "Training rural women to improve access to oral health awareness programmes in remote villages in Nepal". International Journal of Dental Hygiene. 8 (4): 286–93. doi:10.1111/j.1601-5037.2010.00481.x. PMID 20961385.
- Hiremath S. Textbook of Preventive and Community Dentistry. 2nd ed. Elsevier India; 2011.