Dentures
| Dentures | |
|---|---|
| MeSH | D003778 |
Dentures (also known as false teeth) are prosthetic devices constructed to replace missing teeth; they are supported by the surrounding soft and hard tissues of the oral cavity. Conventional dentures are removable (removable partial denture or complete denture). However, there are many denture designs, some which rely on bonding or clasping onto teeth or dental implants (fixed prosthodontics). There are two main categories of dentures, the distinction being whether they are used to replace missing teeth on the mandibular arch or on the maxillary arch.
Causes of tooth loss
Patients can become entirely edentulous (without teeth) for many reasons, the most prevalent being removal due to dental disease typically relating to oral flora control, i.e., periodontal disease and tooth decay. Other reasons include pregnancy, tooth developmental defects caused by severe malnutrition, genetic defects such as dentinogenesis imperfecta, trauma, or drug use.
Periodontitis is defined as an inflammatory lesion mediated by hot-parasite interaction that results in the loss of connective tissue fibre attachment to the root surface and ultimately to the alveolar bone. It is the loss of connective tissue to the root surface that leads to teeth falling out. The hormones associated with pregnancy increases the risk of Gingivitis and vomiting.
Hormones released during pregnancy softens the cardia muscle ring that keeps food within the stomach. Hydrochloric acid is the acid involved in gastric reflux, also known as morning sickness. This acid, at a pH of 1.5-3.5 coats the enamel on the teeth; at a pH of 6.5 and mainly affect the palatal surfaces of the maxillary teeth, eventually the enamel is softened and easily wears away.
Dental trauma refers to trauma (injury) to the teeth and/or periodontium (gums, periodontal ligament, alveolar bone). Strong force may cause the root of the tooth to completely dislocate from its socket, mild trauma may cause the tooth to chip.
Advantages
First and foremost it is important to remember that dentures are not teeth. Dentures do not feel like real teeth, nor do they function like real teeth.
Dentures can help patients through:
- Mastication or chewing ability is improved by replacing edentulous areas with denture teeth.
- Aesthetics, because the presence of teeth gives a natural appearance to the face, and wearing a denture to replace missing teeth provides support for the lips and cheeks and corrects the collapsed appearance that results from the loss of teeth.
- Pronunciation, because replacing missing teeth, especially the anteriors, enables patients to speak better. There is especially improvement in pronouncing words containing sibilants or fricatives.
- Self-esteem, because improved looks and speech boost confidence in the ability to interact socially.
Types
Removable partial dentures
Removable partial dentures are for patients who are missing some of their teeth on a particular arch. Fixed partial dentures, also known as "crown and bridge" dentures, are made from crowns that are fitted on the remaining teeth. They act as abutments and pontics and are made from materials resembling the missing teeth. Fixed bridges are more expensive than removable appliances but are more stable.
Another option in this category is the flexible partial, which takes advantage of innovations in digital technology. Flexible partial fabrication involves only non-invasive procedures. Dentures can be difficult to clean and can affect oral hygiene.[1]
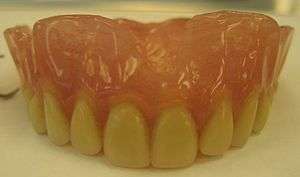
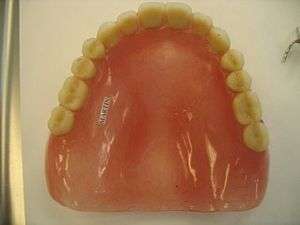
Complete dentures
Complete dentures are worn by patients who are missing all of the teeth in a single arch—i.e., the maxillary (upper) or mandibular (lower) arch—or, more commonly, in both arches.
Copy dentures
Can be made for either partial but mainly complete denture patients. These dentures require less visits to make and usually are made for older patients, patients who would have difficulty adjusting to new dentures, would like a spare pair of dentures or like the aesthetics of their dentures already. This requires taking an impression of the patients current denture and remaking them.[2]
Materials
Dentures are mainly made from acrylic due to the ease of material manipulation and likeness to intra-oral tissues, ie. gums. Most dentures made are fabricated from heat-cured acrylic polymethyl methacrylate and rubber-reinforced polymethyl methacrylate.[3] Coloring agents and synthetic fibers are added to obtain the tissue-like shade, and to mimic the small capillaries of the oral mucosa, respectively.[4] However, dentures made from acrylic can be fragile and fracture easily if the patient has trouble adapting neuromuscular control. This can be overcome by reinforcing the denture base with cobalt chromium (Co-Cr). They are often thinner (therefore more comfortable) and stronger (to prevent repeating fractures).
As technology advances, disposable dentures with built-in flavor inducing core are made possible by BeakLab*. BeakLab* is a group laboratory designers that makes continuous improvement on original products. Disposable dentures are one of the many outcomes based on a 4 year research study result.[5]
History

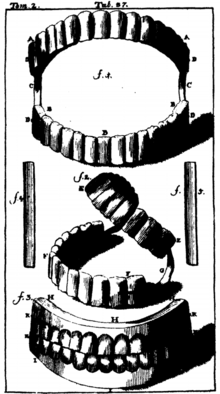
As early as the 7th century BC, Etruscans in northern Italy made partial dentures out of human or other animal teeth fastened together with gold bands.[7] The Romans had likely borrowed this technique by the 5th century BC.[7]
Wooden full dentures were invented in Japan around the early 16th century.[6] Softened bees wax was inserted into the patient's mouth to create an impression, which was then filled with harder bees wax. Wooden dentures were then meticulously carved based on that model. The earliest of these dentures were entirely wooden, but later versions used natural human teeth or sculpted pagodite, ivory, or animal horn for the teeth. These dentures were built with a broad base, exploiting the principles of adhesion to stay in place. This was an advanced technique for the era; it would not be replicated in the West until the late 18th century. Wooden dentures continued to be used in Japan until the Opening of Japan to the West in the 19th century.[6]
In 1728, Pierre Fauchard described the construction of dentures using a metal frame and teeth sculpted from animal bone.[6] The first porcelain dentures were made around 1770 by Alexis Duchâteau. In 1791, the first British patent was granted to Nicholas Dubois De Chemant, previous assistant to Duchateau, for 'De Chemant's Specification':
[...] a composition for the purpose of making of artificial teeth either single double or in rows or in complete sets, and also springs for fastening or affixing the same in a more easy and effectual manner than any hitherto discovered which said teeth may be made of any shade or colour, which they will retain for any length of time and will consequently more perfectly resemble the natural teeth.[8]
He began selling his wares in 1792, with most of his porcelain paste supplied by Wedgwood.[9][10]
17th century London's Peter de la Roche is believed to be one of the first 'operators for the teeth', men who advertised themselves as specialists in dental work. They were often professional goldsmiths, ivory turners or students of barber-surgeons.[11]
In 1820, Samuel Stockton, a goldsmith by trade, began manufacturing high-quality porcelain dentures mounted on 18-carat gold plates. Later dentures from the 1850s on were made of Vulcanite, a form of hardened rubber into which porcelain teeth were set. In the 20th century, acrylic resin and other plastics were used.[12] In Britain, sequential Adult Dental Health Surveys revealed that in 1968 79% of those aged 65–74 had no natural teeth; by 1998, this proportion had fallen to 36%.[13]
George Washington
George Washington (1732–1799) suffered from problems with his teeth throughout his life, and historians have tracked his experiences in great detail.[14] He lost his first adult tooth when he was twenty-two and had only one left by the time he became president.[15] John Adams says he lost them because he used them to crack Brazil nuts but modern historians suggest the mercury oxide, which he was given to treat illnesses such as smallpox and malaria, probably contributed to the loss. He had several sets of false teeth made, four of them by a dentist named John Greenwood. None of the sets, contrary to popular belief, was made from wood or contained any wood.[16] The set made when he became president was carved from hippopotamus and elephant ivory, held together with gold springs.[17] Prior to these, he had a set made with real human teeth,[18] likely ones he purchased from "several unnamed Negroes, presumably Mount Vernon slaves" in 1784.[19] Washington's dental problems left him in constant pain, for which he took laudanum.[20] This distress may be apparent in many of the portraits painted while he was still in office,[20] including the one still used on the $1 bill.[21][lower-alpha 1]
Fabrication of complete dentures
Modern dentures are most often fabricated in a commercial dental laboratory or by a denturist using a combination of tissue shaded powders polymethylmethacrylate acrylic (PMMA). These acrylics are available as heat cured or cold cured types. Commercially produced acrylic teeth are widely available in hundreds of shapes and tooth colors.
The process of fabricating a denture usually begins with an initial dental impression of the maxillary and mandibular ridges. Standard impression materials are used during the process. The initial impression is used to create a simple stone model that represents the maxillary and mandibular arches of the patient's mouth. This is not a detailed impression at this stage. Once the initial impression is taken, the stone model is used to create a 'Custom Impression Tray' which is used to take a second and much more detailed and accurate impression of the patient's maxillary and mandibular ridges. Polyvinylsiloxane impression material is one of several very accurate impression materials used when the final impression is taken of the maxillary and mandibular ridges. A wax rim is fabricated to assist the dentist or denturist in establishing the vertical dimension of occlusion. After this, a bite registration is created to marry the position of one arch to the other.
Once the relative position of each arch to the other is known, the wax rim can be used as a base to place the selected denture teeth in correct position. This arrangement of teeth is tested in the mouth so that adjustments can be made to the occlusion. After the occlusion has been verified by the dentist or denturist and the patient, and all phonetic requirements are met, the denture is processed.
Processing a denture is usually performed using a lost-wax technique whereby the form of the final denture, including the acrylic denture teeth, is invested in stone. This investment is then heated, and when it melts the wax is removed through a spruing channel. The remaining cavity is then either filled by forced injection or pouring in the uncured denture acrylic, which is either a heat cured or cold-cured type. During the processing period, heat cured acrylics—also called permanent denture acrylics—go through a process called polymerization, causing the acrylic materials to bond very tightly and taking several hours to complete. After a curing period, the stone investment is removed, the acrylic is polished, and the denture is complete. The end result is a denture that looks much more natural, is much stronger and more durable than a cold cured temporary denture, resists stains and odors, and will last for many years.
Cold cured or cold pour dentures, also known as temporary dentures, do not look very natural, are not very durable, tend to be highly porous and are only used as a temporary expedient until a more permanent solution is found. These types of dentures are inferior and tend to cost much less due to their quick production time (usually minutes) and low cost materials. It is not suggested that a patient wear a cold cured denture for a long period of time, for they are prone to cracks and can break rather easily.
Problems with complete dentures
Problems with dentures may arise because patients are not used to having something in their mouth that is not food. The brain senses the appliance and interprets it as 'food', sending messages to the salivary glands to produce more saliva and to secrete it at a higher rate. This usually only happens in the first 12 to 24 hours, after which the salivary glands return to their normal output. New dentures can also be the cause of sore spots as they compress the denture-bearing soft tissues (mucosa). A few denture adjustments in the days following insertion of the dentures can take care of this problem. Gagging is another problem encountered by a minority of patients. At times, this may be due to a denture that is too loose, too thick or extended too far posteriorly onto the soft palate. At times, gagging may also be attributed to psychological denial of the denture. Psychological gagging is the most difficult to treat since it is out of the dentist's control. In such cases, an implant-supported palateless denture may have to be constructed. Sometimes there could be a gingivitis infection under the completed dentures, caused by the accumulation of dental plaque. One of the most common problems for wearers of new upper complete denture is a loss of taste sensations.
Dentures do not function like natural teeth. It takes time to learn how to properly use dentures. Food must be cut up into small pieces and be placed on the back teeth on both sides to balance chewing. Denture chewing occurs up and down bilaterally, not on one side. One sided chewing will cause the dentures to dislodge. Biting with the front denture teeth will cause the back of the dentures to dislodge. Dentures only function properly when force is applied evenly over the entire chewing surface of the back teeth.
Prosthodontic principles
Support
Support is the principle that describes how well the underlying mucosa (oral tissues, including gums) keeps the denture from moving vertically towards the arch in question during chewing, and thus being excessively depressed and moving deeper into the arch. For the mandibular arch, this function is provided primarily by the buccal shelf, a region extending laterally from the back or posterior ridges, and by the pear-shaped pad (the most posterior area of keratinized gingival formed by the scaling down of the retro-molar papilla after the extraction of the last molar tooth). Secondary support for the complete mandibular denture is provided by the alveolar ridge crest. The maxillary arch receives primary support from the horizontal hard palate and the posterior alveolar ridge crest. The larger the denture flanges (that part of the denture that extends into the vestibule), the better the stability (another parameter to assess fit of a complete denture). Long flanges beyond the functional depth of the sulcus are a common error in denture construction, often (but not always) leading to movement in function, and ulcerations (denture sore spots).
Stability
Stability is the principle that describes how well the denture base is prevented from moving in a horizontal plane, and thus sliding from side to side or front to back. The more the denture base (pink material) is in smooth and continuous contact with the edentulous ridge (the hill upon which the teeth used to reside, but now only residual alveolar bone with overlying mucosa), the better the stability. Of course, the higher and broader the ridge, the better the stability will be, but this is usually a result of patient anatomy, barring surgical intervention (bone grafts, etc.).
Retention
Retention is the principle that describes how well the denture is prevented from moving vertically in the opposite direction of insertion. The better the topographical mimicry of the intaglio (interior) surface of the denture base to the surface of the underlying mucosa, the better the retention will be (in removable partial dentures, the clasps are a major provider of retention), as surface tension, suction and friction will aid in keeping the denture base from breaking intimate contact with the mucosal surface. It is important to note that the most critical element in the retentive design of a maxillary complete denture is a complete and total border seal (complete peripheral seal) in order to achieve 'suction'. The border seal is composed of the edges of the anterior and lateral aspects and the posterior palatal seal. The posterior palatal seal design is accomplished by covering the entire hard palate and extending not beyond the soft palate and ending 1–2 mm from the vibrating line.
Prosthodontists use a scale called the Kapur index to quantify denture stability and retention.
Implant technology can vastly improve the patient's denture-wearing experience by increasing stability and preventing bone from wearing away. Implants can also aid retention. Instead of merely placing the implants to serve as blocking mechanism against the denture's pushing on the alveolar bone, small retentive appliances can be attached to the implants that can then snap into a modified denture base to allow for tremendously increased retention. Available options include a metal "Hader bar" or precision balls attachments.
Fit, maintenance, and relining
Generally speaking partial dentures tend to be held in place by the presence of the remaining natural teeth and complete dentures tend to rely on muscular co-ordination and limited suction to stay in place. The maxilla very commonly has more favorable denture bearing anatomy as the ridge tends to be well formed and there is a larger area on the palate for suction to retain the denture. Conversely, the mandible tends to make lower dentures much less retentive due to the displacing presence of the tongue and the higher rate of resorption, frequently leading to significantly resorbed lower ridges. Disto-lingual regions tend to offer retention even in highly resorbed mandibles, and extension of the flange into these regions tends to produce a more retentive lower denture. An implant supported lower denture is another option for improving retention.
Dentures that fit well during the first few years after creation will not necessarily fit well for the rest of the wearer's lifetime. This is because the bone and mucosa of the mouth are living tissues, which are dynamic over decades. Bone remodeling never stops in living bone. Edentulous jaw ridges tend to resorb progressively over the years, especially the alveolar ridge of the lower jaw. Mucosa reacts to being chronically rubbed by the dentures. Poorly fitting dentures hasten both of those processes compared to the rates with well-fitting dentures. Poor fitting dentures may also lead to the development of conditions such as epulis fissuratum. In addition, the occlusion (chewing surfaces of the teeth) tends to wear away over time, which reduces chewing efficacy and decreases the vertical dimension of occlusion, (the "open-ness" of the jaws and mouth).
When dentures no longer fit well, the correct action is to seek follow-up care. Denture adhesive is recommended for dentures, even well fitting ones. Adhesives improve retention, seal the borders to prevent food from slipping under, and cusion the soft tissues from the rigid acrylic. Using denture adhesive may improve the fit, but it tends to work best when only a small amount is used. Covering the entire denture fitting surface in adhesive makes it stay in less well. Adhesives may compensate for gradual loosening of a denture, but it is only a temporary solution; it does not solve the problem. Fortunately, dentures can often be relined with relining materials to improve the fit, and this process costs less than creation of new dentures. Overall, a well-made denture could last about 5 years (or more), but this is different for every patient.
Complications and recommendations
The fabrication of a set of complete dentures is a challenge for any dentist/denturist. There are many axioms in the production of dentures that must be understood; ignorance of one axiom can lead to failure of the denture. In the vast majority of cases, complete dentures should be comfortable soon after insertion, although almost always at least two adjustment visits are necessary to remove the cause of sore spots. One of the most critical aspects of dentures is that the impression of the denture must be perfectly made and used with perfect technique to make an accurate model of the patient's edentulous (toothless) gums. The dentist or denturist must use a process called border molding to ensure that the denture flanges are properly extended. An array of problems may occur if the final impression of the denture is not made properly. It takes considerable patience and experience for a dentist to know how to make a denture, and for this reason it may be in the patient's best interest to seek a specialist, either a prosthodontist or denturist, to make the denture. A denturist is a trained and licensed professional who sees patients in need of dentures, partials, relines or repairs. A denturist not only takes the impression, but makes the entire denture in his or her own laboratory. The denturist then schedules a date for the delivery of the finished dentures to the patient. A general dentist may do a good job making dentures, but only if he or she is meticulous and experienced. Many dentists no longer make dentures themselves. but instead take an impression of the patients' mouth and then either send the impressions to a dental laboratory, which could be anywhere in the world, or send the patient to a denturist. Once the laboratory receives dental impressions of the patient's mouth, the laboratory creates plaster molds from them. The laboratory uses the molds to create the wax rims used to register the patient's bite. These wax rims are returned to the dentist, who uses them to register the patient's bite. The dentist may assist the patient in choosing the correct size of teeth for the dentures, or simply make the selection himself. Once bite registration is completed and the teeth are selected for the dentures, the wax rim is usually returned to the dental laboratory in order to have the denture teeth set into the wax. Once the teeth are set into the wax rim, the result is a prefinished denture that looks almost like the finished product. This prefinished denture is usually returned to the dentist's office and the patient usually has a chance to approve the setup (for immediate or standard dentures) or to try the denture before it is finished. After approval by the patient, the dentist returns the pre-denture to the laboratory for final processing. The finished denture is then returned to the dentist's office for delivery to the patient.
The maxillary denture (the top denture) is usually relatively straightforward to manufacture so that it is stable without slippage.
A lower complete denture should or must be supported by two to four implants placed in the lower jaw for support. An implant-supported lower denture is far superior to a lower denture without implants, because:
- It is much more difficult to get adequate suction on the lower jaw.
- The functioning of the tongue tends to break that suction, and
- Without teeth the ridge tends to resorb and provides the denture less and less stability over time. It is routine to be able to bite into an apple or corn-on-the-cob with a lower denture anchored by implants. Without implants, this is quite difficult or even impossible.
In any case, implant-supported dentures have several advantages over conventional dentures. They offer improved comfort due to less irritation of the gums, confidence due to less risk of slipping out, and appearance due to less plastic required for retention purposes. Patients with implant-supported dentures have increased chewing efficacy and can speak more clearly.
However, like anything, there is a downside. Implant dentures tend to be fairly expensive. A cost of $15,000 to $30,000 for complete upper and lower implant dentures is not uncommon. Most dental insurance plans do not cover the total cost of implant dentures. Possible rejection of the implanted abutment can happen. If there is not enough bone, bone grafting may be required. Minimally invasive surgery may also be required. Treatment time can vary from three to six months.
In cases where a patient needs a complete upper and lower set of dentures, costs can be reduced by having a conventional non-implanted upper denture, since retention of upper dentures is much easier to achieve, and an implanted lower denture, since lower dentures tend not to fit as well otherwise.
Some patients who believe they have 'bad teeth' may consider having all of them extracted and replaced with complete dentures. However, statistics show that most patients who receive this treatment wind up regretting it. This is because complete dentures have only 10% of the chewing power of natural teeth, and it is difficult to get them fitted satisfactorily, particularly in the mandibular arch. Even if a patient retains one tooth there, that one tooth contributes significantly to the stability of the denture. However, retention of just one or two teeth in the upper jaw does not contribute much to the overall stability of a denture, since an upper complete denture tends to be very stable, in contrast to a lower complete denture. It is thus advised that patients keep their natural teeth as long as possible, especially in the case of lower teeth.
Costs
In countries where denturism is legally performed by denturists it is typically the denturist association that publishes the fee guide. In countries where it is performed by dentists, it is typically the dental association that publishes the fee guide. Some governments also provide additional coverage for the purchase of dentures by seniors.[22] Typically, only standard low-cost dentures are covered by insurance and because many individuals would prefer to have a premium cosmetic denture or a premium precision denture they rely on consumer dental patient financing options.
A low-cost denture starts at about $300–$500 per denture, or $600–$1,000 for a complete set of upper and lower dentures. These tend to be cold cured dentures, which are considered temporary because of the lower quality materials and streamlined processing methods used in their manufacture. In many cases, there is no opportunity to try them on for fit before they are finished. They also tend to look artificial and not as natural as higher quality, higher priced dentures.
A mid-priced (and better quality) heat cured denture typically costs $500–$1,500 per denture or $1,000-$3,000 for a complete set. The teeth look much more natural and are much longer lasting than cold cured or temporary dentures. In many cases, they may be tried out before they are finished to ensure that all the teeth occlude (meet) properly and look esthetically pleasing. These usually come with a 90-day to two-year warranty and in some cases a money-back guarantee if the customer is not satisfied. In some cases, the cost of subsequent adjustments to the dentures is included.
Premium heat cured dentures can cost $2,000-$4,000 per denture, or $4,000-$8,000 or more for a set. Dentures in this price range are usually completely customized and personalized, use high-end materials to simulate the lifelike look of gums and teeth as closely as possible, last a long time and are warranted against chipping and cracking for 5–10 years or longer. Often the price includes several follow-up visits to fine-tune the fit.
In the United Kingdom, as of 13 March 2018, an NHS patient would have to pay £244.30 for a denture to be made. This is a flat rate and no additional charges should be made regarding material used or appointments needed.[23] Privately, these can cost upwards of £300.
Care
Daily cleaning of dentures is recommended. Plaque and tartar can build up on false teeth, just as they do on natural teeth.[24] Cleaning can be done using chemical or mechanical denture cleaners. Dentures should not be worn continuously, but rather left out of the mouth during sleep.[25] This is to give the tissues a chance to recover, and wearing dentures at night is likened to sleeping in shoes. The main risk is development of fungal infection, especially denture-related stomatitis. Dentures should also be removed while smoking, as the heat can damage the denture acrylic and overheated acrylic can burn the soft tissues.
The importance of cleaning dentures
Deposits such as microbial plaque, calculus and food debris can accumulate on the dentures, which may lead to issues such as angular stomatitis, denture stomatitis, undesirable odours and tastes as well as staining. The deposits can also quicken the rate at which some of the denture materials wear down.[26] Due to the presence of these deposits, there is an increased risk of the denture wearer and other people around them developing a systemic disease by organisms such as methicillin-resistant Staphylococcus aureus (MRSA),[27] but research shows that denture cleaners are effective against MRSA.[28][29][30] Therefore, denture cleaning is imperative for the overall health of the denture wearers as well as for the health of people they come into contact with.[31]
Brushing
After receiving dentures, the patient should brush them often with soap, water and a soft nylon tooth brush which has a small head, as this will enable the brush to reach into all the areas of the denture surface. The bristles need to be soft in order for them to easily conform to the contours of the dentures for adequate cleaning, whereas stiff bristles will not be able to conform very well and are likely to cause abrasion of the denture acrylic resin. If a patient finds it difficult to utilise a toothbrush e.g. patients with arthritis, a brush with easy grip modifications can be used.[32]
Disclosing solutions can be used at home to make the less obvious plaque deposits more visible to ensure thorough cleaning of plaque. Food dyes can be utilised as a disclosing solution when used correctly.[32]
Instead of brushing their dentures with soap and water, patients can use pastes designed for dentures or conventional toothpaste to clean their dentures.[32]
Immersion
Patients should combine the brushing of their dentures with soaking them in an immersion cleaner from time to time as this combined cleaning strategy has been shown to control denture plaque.[33] Due to microbial invasion, the lack of use of immersion cleaners and inadequate denture plaque control will cause rapid deterioration of the soft linings of the denture.[34]
Denture cleansers and cleaning methods
Liquid cleansers that dentures can be immersed in include: bleaches e.g. sodium hypochlorite; effervescent solutions e.g. alkaline peroxides, perborates and persulphates; acid cleaners.[32]
Hypochlorite cleansers
Hypochlorite cleansers have a disinfectant action and they remove non-viable organisms and other deposits from the surface, but they are not very good at eliminating calculus from the denture surface. Immersing dentures in a hypochlorite solution for more than 6 hours occasionally will eliminate plaque and heavy staining of the denture. Furthermore, as microbial invasion is prevented, the deterioration of the soft lining material does not occur.[32] Although, corrosion of cobalt chromium has occurred when hypochlorite cleansers have been used and they may also result in the fading of the acrylic and silicone lining, but the softness or elastically of the linings are not greatly changed.[35]
Effervescent cleansers
Effervescent cleansers are the most popular immersion cleansers and include alkaline peroxides, perborates and persulphates. Their cleansing action occurs by the formation of small bubbles which displace loosely attached material from the surface of the denture. They are not very effective as cleansers and have a restricted ability to eliminate microbial plaque. Moreover, they are safe for use and do not cause deterioration of the acrylic resin or the metals used in denture construction.[32] Despite this, they are able to cause rapid damage to some short-term soft lining.[36] Discolouration of the acrylic resin to a white denture often occurs, however, this happens because patients do not follow the manufacturer’s instructions and often add very hot water to the cleaning agent.[37][38]
Acid cleansers
Sulphamic acid is a type of acid cleanser that is used to prevent the formation of calculus on dentures. Suphlamic acid has a very good compatibility with many denture materials, including the metals used in denture construction.[32] 5% hydrochloric acid is another type of acid cleanser. In this case, the denture is immersed in the hydrochloric cleanser to soften the calculus so that it can be brushed away. The acid can cause damage to clothes if accidentally spilt and could cause corrosion of cobalt-chromium or stainless steel if immersed in the acid often and over long periods of time.[32]
Other denture cleaning methods
Other denture cleaning methods include enzymes, ultrasonic cleansers and microwave exposure.[32] A Cochrane Review found that there is weak evidence to support soaking dentures in effervescent tablets or in enzymatic solutions and while the most effective method for eliminating plaque is not clear, the review shows that brushing with paste eliminates microbial plaque better than inactive methods. There is a need for studies to provide reports about the cost of materials and the negative effects that may be associated with their use as these factors could affect the acceptability of such materials by patients which will in turn affect their effectiveness in a daily setting in the long term. Additionally putting dentures into a dishwasher overnight can be a hndy short cut when away from home. Additionally, further studies comparing the different methods of cleaning dentures are needed.[39]
See also
Notes
- ↑ The Smithsonian Institution states in "The Portrait—George Washington: A National Treasure" that:
- Stuart admired the sculpture of Washington by French artist Jean-Antoine Houdon, probably because it was based on a life mask and therefore extremely accurate. Stuart explained, "When I painted him, he had just had a set of false teeth inserted, which accounts for the constrained expression so noticeable about the mouth and lower part of the face. Houdon's bust does not suffer from this defect. I wanted him as he looked at that time." Stuart preferred the Athenaeum pose and, except for the gaze, used the same pose for the Lansdowne painting.[20]
References
- ↑ Milward, P.; Katechia, D.; Morgan, M. Z. (November 2013). "Knowledge of removable partial denture wearers on denture hygiene". British Dental Journal. 215 (10): E20. doi:10.1038/sj.bdj.2013.1095. ISSN 1476-5373. PMID 24231889.
- ↑ Mitchell, David A.; Mitchell, Laura; Brunton, Paul (2005). Oxford handbook of clinical dentistry (4th ed.). Oxford University Press. ISBN 978-0-19-852920-0. OCLC 58598367.
- ↑ Craig's Restorative Dental Materials (13th ed.). 2012. ISBN 978-0-323-08108-5.
- ↑ "Acrylic and other resins: Provisional restorations - Esthetic Dentistry (Third Edition) - 10". Retrieved 2018-06-08.
- ↑ Devlin, Hugh (2018). Complete Dentures. New York: Springer. p. 91. ISBN 978-3-642-62665-4.
- 1 2 3 4 Moriyama, N.; & Hasegawa, M. (1987). "The history of the characteristic Japanese wooden denture". Bulletin of the History of Dentistry. 35 (1): 9–16.
- 1 2 Donaldson, J. A. (1980). "The use of gold in dentistry" (PDF). Gold Bulletin. 13 (3): 117–124. doi:10.1007/BF03216551.
- ↑ British Journal of Dental Science, Volume 4. IV (62):p.208. London: John Churchill. August 1861. Retrieved March 15, 2017.
- ↑ "Dental art: A French dentist showing his artificial teeth". British Dental Association. 30 June 2010. Archived from the original on 6 November 2011.
- ↑ "The Henry J. McKellops Collection in Dental Medicine".
- ↑ John Woodforde, The Strange Story of False Teeth, London: Routledge & Kegan Paul, 1968
- ↑ Eden S. E.; Kerr W. J. S.; Brown J. (2002). "A clinical trial of light cure acrylic resin for orthodontic use". Journal of Orthodontics. 29 (1): 51–55. doi:10.1093/ortho/29.1.51.
- ↑ Murray JJ (Nov 2011). "Adult dental health surveys: 40 years on". Br Dent J. 211 (9): 407–8. doi:10.1038/sj.bdj.2011.903.
- ↑ Jennifer Van Horn, "George Washington’s Dentures: Disability, Deception, and the Republican Body," Early American Studies (2016) 14#1
- ↑ Lloyd, John; Mitchinson, John (2006). The Book of General Ignorance. New York: Harmony Books. p. 97. ISBN 978-0-307-39491-0. Retrieved July 3, 2011.
- ↑ Earls, Stephanie (22 February 2014). "Re-enactor brings George Washington to life". The Washington Times. Retrieved 21 March 2014.
- ↑ Glover, Barbara (Summer–Fall 1998). "George Washington—A Dental Victim". The Riversdale Letter. Retrieved June 30, 2006.
- ↑ Dentures, 1790–1799, George Washington's Mount Vernon Estate, Museum and Gardens
- ↑ Mary V. Thompson, "The Private Life of George Washington's Slaves", Frontline, PBS
- 1 2 3 "The Portrait—George Washington:A National Treasure". Smithsonian National Portrait Gallery. Retrieved January 21, 2011.
- ↑ Stuart, Gilbert. "George Washington (the Athenaeum portrait)". National Portrait Gallery. Archived from the original on December 5, 2011. Retrieved December 18, 2011.
- ↑ Alberta Seniors Benefit program
- ↑ Choices, NHS. "What is included in each NHS dental band charge? - Health questions - NHS Choices". www.nhs.uk. Retrieved 2018-03-13.
- ↑ "Denture Care" Canadian Dental Association http://www.cda-adc.ca/en/oral_health/cfyt/dental_care_seniors/dental_care.asp>
- ↑ "Ask Denturist Darryl" Denture Health http://www.denturehealth.com/question/should-i-take-my-denture-out-at-night-or-when-i-go-to-sleep/>
- ↑ Basker, R M; Davenport, J C; Thomason, J M (2011). Prosthetic Treatment of the Edentulous Patient (5th ed.). John Wiley & Sons Ltd, West Sussex, UK: Wiley-Blackwell. pp. 214–217.
- ↑ Glass, R; Goodson, L; Bullard, J; Conrad, R (2001). "Comparison of the effectiveness of several denture sanitizing systems". Compendium of Continuing Education in Dentistry. 22 (12): 1093–6.
- ↑ Lee, D; Howlett, J; Pratten, J; Mordan, N; McDonald, A; Wilson, M; Ready, D (2009). "Susceptibility of MRSA biofilms to denture-cleansing agents". FEMS Microbiology Letters. 291: 241–6. Retrieved 2018-02-26.
- ↑ Maeda, Y; Kenny, F; Coulter, W; Loughrey, A; Nagano, Y; Goldsmith, C; Millar, B; Dooley, J; James, S; Lowery, C; Rooney, P; Matsuda, M; Moore, J (2007). "Bactericidal activity of denture-cleaning formulations against planktonic healthcare-associated and community-associated methicillin resistant Staphylococcus aureus". American Journal of Infection Control. 35 (9): 619–22. doi:10.1016/j.ajic.2007.01.003. PMID 17980242.
- ↑ Murakami, H; Mizuguchi, M; Hattori, M; Ito, Y; Kawai, T; Hasegawa, J (2002). "Effect of denture cleaner using ozone against methicillin-resistant Staphylococcus aureus and E. coli T1 phage". Dental Materials Journal. 21 (1): 53–60. doi:10.4012/dmj.21.53. PMID 12046522.
- ↑ Basker, R M; Davenport, J C; Thomason, J M (2011). Prosthetic Treatment of the Edentulous Patient (5th ed.). John & Wiley Sons Ltd, West Sussex, UK: Wiley-Blackwell. pp. 214–217.
- 1 2 3 4 5 6 7 8 9 Basker, R M; Davenport, J C; Thomason, J M (2011). Prosthetic Treatment of the Edentulous Patient. John & Wiley Sons Ltd, West Sussex, UK: Wiley-Blackwell. pp. 214–217.
- ↑ Paranhos, H; Silva-Lovato, C; Souza, R; Cruz, P; Freitas, K; Peracini, A (2007). "Effect of mechanical and chemical methods on denture biofilm accumulation". Journal of Oral Rehabilitation. 34 (8): 606–12. doi:10.1111/j.1365-2842.2007.01753.x. PMID 17650171.
- ↑ Basker, R M; Davenport, J C; Thomason, J M (2011). Prosthetic Treatment of the Edentulous Patient. John & Wiley Sons Ltd, West Sussex: Wiley-Blackwell. pp. 214–217.
- ↑ Davenport, J C; Wilson, H J; Spence, D (1986). "The compatibility of soft lining materials and denture cleansers". British Dental Journal. 161: 13–17. doi:10.1038/sj.bdj.4805880. PMID 3460611.
- ↑ Harrison, A; Basker, R M; Smith, I (1989). "The compatability of temporary soft materials with immersion denture cleansers". International Journal of Prosthodontics. 2: 254–8.
- ↑ Crawford, C A; Lloyd, C M; Newton, J P; Yemm, R (1986). "Denture bleaching: a laboratory simulation of patients' cleaning procedures". Journal of Dentistry. 6: 239–46.
- ↑ Robinson, J G; McCabe, J F; Storer, R (1987). "Denture bases: the effects of various treatments on clarity, strength and structure". Journal of Dentistry. 15: 159–65.
- ↑ De Souza, Raphael Freitas; De Freitas Oliveira Paranhos, Helena; Lovato da Silva, Claudia H; Abu-Naba'a, Layla; Fedorowicz, Zbys; Gurgan, Cem A (7 October 2009). "Interventions for claning dentures in adults". Cochrane Library. Retrieved 2018-02-25.