Pulp (tooth)
| Pulp | |
|---|---|
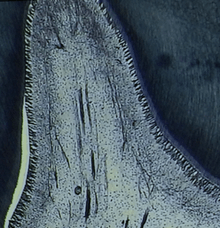
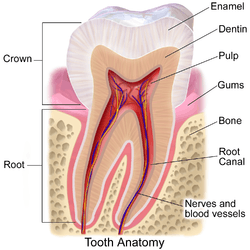 Section of a human molar | |
| Details | |
| Identifiers | |
| Latin | pulpa dentis |
| MeSH | D003782 |
| TA | A05.1.03.051 |
| FMA | 55631 |
| Anatomical terminology | |
The pulp, or endodontium, is the part in the center of a tooth made up of living connective tissue and cells called odontoblasts. The dental pulp is a part of the dentin–pulp complex (endodontium).[1] The vitality of the dentin-pulp complex, both during health and after injury, depends on pulp cell activity and the signaling processes that regulate the cell’s behavior.[2]
Anatomy
The pulp is the neurovascular bundle central to each tooth, permanent or primary. It comprises a central pulp chamber, pulp horns, and radicular canals. The large mass of pulp is contained within the pulp chamber, which is contained in and mimics the overall shape of the crown of the tooth.[2] Because of the continuous deposition of dentin, the pulp chamber becomes smaller with age. This is not uniform throughout the coronal pulp but progresses faster on the floor than on the roof or side walls.
Radicular pulp canals extend down from the cervical region of the crown to the root apex. They are not always straight but vary in shape, size, and number. They are continuous with the periapical tissues through the apical foramen or foramina.
The total volumes of all the permanent teeth organs is 0.38cc and the mean volume of a single adult human pulp is 0.02cc.
Accessory canals are pathways from the radicular pulp, extending laterally through the dentin to the periodontal tissue seen especially in the apical third of the root. Accessory canals are also called lateral canals because they are usually located on the lateral surface of the roots of the teeth.
Development
The pulp has a background similar to that of dentin, because both are derived from the dental papilla of the tooth germ. During odontogenesis, when the dentin forms around the dental papilla, the innermost tissue is considered pulp.[3]
Internal structure
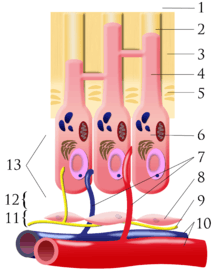
The central region of the coronal and radicular pulp contains large nerve trunks and blood vessels.
This area is lined peripherally by a specialized odontogenic area which has four layers (from innermost to outermost):
- Pulpal core, which is in the center of the pulp chamber with many cells and an extensive vascular supply; except for its location, it is very similar to the cell-rich zone.
- Cell rich zone; which contains fibroblasts and undifferentiated mesenchymal cells.
- Cell free zone (zone of Weil) which is rich in both capillaries and nerve networks.
- Odontoblastic layer; outermost layer which contains odontoblasts and lies next to the predentin and mature dentin.
Cells found in the dental pulp include fibroblasts (the principal cell), odontoblasts, defence cells like histiocytes, macrophage, granulocytes, mast cells and plasma cells.The nerve plexus of Raschkow is located central to the cell-rich zone.[3]
The plexus of Raschkow
The plexus of Raschkow monitors painful sensations. By virtue of their peptide content they also play important functions in inflammatory events and subsequent tissue repair. There are two types of nerve fiber that mediate the sensation of pain: A-fibers conduct rapid and sharp pain sensations and belong to the myelinated group, whereas C-fibers are involved in dull aching pain and are thinner and unmyelinated. The A-fibers, mainly of the A-delta type, are preferentially located in the periphery of the pulp, where they are in close association with the odontoblasts and extend fibers to many but not all dentinal tubules. The C-fibers typically terminate in the pulp tissue proper, either as free nerve endings or as branches around blood vessels. Sensory nerve fibers that originate from inferior and superior alveolar nerves innervate the odontoblastic layer of the pulp cavity. These nerves enter the tooth through the apical foramen as myelinated nerve bundles. They branch to form the subodontoblastic nerve plexus of Raschkow which is separated from the odontoblasts by a cell-free zone of Weil, therefore this plexus lies between the cell free and cell rich zones of the pulp.
Functions
The primary function of the dental pulp is to form dentin (by the odontoblasts).
Other functions include:
- Nutritive: the pulp keeps the organic components of the surrounding mineralized tissue supplied with moisture and nutrients;
- Protective/Sensory: extremes in temperature, pressure, or trauma to the dentin or pulp are perceived as pain;
- Defensive/reparative : the formation of reparative or tertiary dentin (by the odontoblasts);
- Formative: cells of the pulp produce dentin which surrounds and protects the pulpal tissue.
Pulp Testing
[4] Dental pulp testing is an investigation that is used to assess the pulpal vitality. This assessment is crucial in order to plan the most suitable endodontic treatment for the tooth. Traditionally, the pulp’s condition is inspected via a pulp sensibility test, which extrapolates pulpal status based on its sensory response towards stimuli such as heat and cold. Listed are the diagnostic techniques most commonly used to assess the pulpal sensitivity:
1. Thermal Test
a. Heat test – A heated Gutta-Percha stick is the most commonly used method for heat testing.
b. Cold Test – Ethyl Chloride, frozen carbon dioxide (dry ice) and Dichlorodifluoromethane (Freon) are used as cold testing material.
2.[5] Electric pulp testing – Health status of the pulp is tested by electrical excitations of neural elements within the pulp.
3. Anaesthesia testing – A single tooth is anaesthetized at a time until the pain is diminished. If the pain continues, the procedure is repeated to the next tooth mesial to it. It is continued until the pain is gone. If source of pain cannot be determined, the same technique on the opposite arch is repeated.
4. Bite test – In this test patient is asked to bite on a hard object such as cotton swab, tooth pick, or orange wood stick. Pain on biting may indicate a fractured tooth.
5. Test cavity – This technique is only used when the results produced by all other methods above are inconclusive. High speed burs are used to make the test cavity. Patient is asked whether painful sensation is felt during drilling. Pulpal vitality is indicated if there is any sensitivity or pain felt by the patient.
However, these traditional testing methods have some disadvantages compared to the pulp vitality test in which the pulp blood circulation is evaluated instead. Major limitations of the traditional pulp sensitivity test include:
- Likelihood to elicit an uncomfortable and sometimes painful sensation in the patient.
- May yield false positive or false negative results. These tests only indicate the pulpal sensory fibres' vitality but do not always reflect the stage and extent of pulpal disease.
- Subjective nature of the test. The pulp sensibility test depends on the patient’s response to a particular stimulus and the dentist’s interpretation of that response.
Recent studies have suggested that blood circulation is the most reliable factor in testing the pulp’s vitality. The recent diagnostic methods to assess the vascular response of the pulp include:
3. Dual Wavelength Spectrophotometry
Reversible Pulpitis
A mild to moderate inflammation of dental pulp caused by any momentary irritation or stimulant whereby no pain is felt upon removal of stimulants.[6] Nevertheless, there is no significant radiographic changes in the periapical region hence further examination is mandatory to ensure that the dental pulp has returned to its normal healthy state.[7]
Common Causes [6]
- Bacterial infection from caries
- Thermal shock
- Trauma
- Excessive dehydration of a cavity during restoration
- Irritation of exposed dentine
Symptoms [6]
- Temporary post-restoration sensitivity
- Short sharp pain due to a stimulant
Prevention [6]
- Regular check-ups for carcinogenic or non-carcinogenic caries
- When preparing cavities, dehydrate with adequate amount of alcohol or chloroform and apply enough varnish to protect the pulp
Irreversible Pulpitis
Pain occurs spontaneously if the reversible pulpitis hasn’t been treated well leaving the cause of inflammation. Usually occurs as a result of cracked tooth following trauma,[8] extensive restorations,[7] dental caries.[8] Incapable of healing and hence root canal treatment is required. It can present as symptomatic irreversible pulpitis or asymptomatic irreversible pulpitis.[7]
Symptoms
The intensity of pain varies at different temperatures. A person may experience
- A spontaneous, high intensity pain while eating hot and cold products(thermal stimulus).[7][8]
- A lingering pain which often lasts for 30 seconds or longer after the stimulus is removed.[7][8]
- Referred pain[7]
- No tender to percussion[7]
Treatments: Require endodontic (root canal) treatment or tooth extraction. In endodontic therapy, removal of the inflamed pulp relieves the pain. The empty root canal system is then obturated with Gutta-Percha which is a rubber material that acts as a pressure and pain reliever.[8]
Complications
Pulp acts as a security and alarm system for a tooth. Slight decay in tooth structure not extending to the dentin may not alarm the pulp but as the dentin gets exposed, either due to dental caries or trauma, sensitivity starts. The dentinal tubules pass the stimulus to odontoblastic layer of the pulp which in turns triggers the response. This mainly responds to cold. At this stage simple restorations can be performed for treatment. As the decay progresses near the pulp the response also magnifies and sensation to a hot diet as well as cold gets louder. At this stage indirect pulp capping might work for treatment but at times it is impossible to clinically diagnose the extent of decay, pulpitis may elicit at this stage. Carious dentin by dental decay progressing to pulp may get fractured during mastication (chewing food) causing direct trauma to the pulp hence eliciting pulpitis.
The inflammation of the pulp is known as pulpitis. Pulpitis can be extremely painful and in serious cases calls for root canal therapy or endodontic therapy.[9] Traumatized pulp starts an inflammatory response but due to the hard and closed surroundings of the pulp pressure builds inside the pulp chamber compressing the nerve fibres and eliciting extreme pain (acute pulpitis). At this stage the death of the pulp starts which eventually progresses to periapical abscess formation (chronic pulpitis).
The pulp horns recede with age. Also with increased age, the pulp undergoes a decrease in intercellular substance, water, and cells as it fills with an increased amount of collagen fibers.This decrease in cells is especially evident in the reduced number of undifferentiated mesenchymal cells. Thus, the pulp becomes more fibrotic with increased age, leading to a reduction in the regenerative capacity of the pulp due its loss of these cells. Also, the overall pulp cavity may be smaller by the addition of secondary or tertiary dentin, thus causing pulp recession. The lack of sensitivity associated with older teeth is due to receded pulp horns, pulp fibrosis, addition of dentin, or possibly all these age-related changes; many times restorative treatment can be performed without local anesthesia on older dentitions.[2]
See also
References
- ↑ http://endodontistrootcanal.com/endodontium/
- 1 2 3 Illustrated Dental Embryology, Histology, and Anatomy, Bath-Balogh and Fehrenbach, Elsevier, 2011, page 164.
- 1 2 Antonio Nanci, Ten Cate's Oral Histology, Elsevier, 2007, page 91
- ↑ Garg, Nisha Garg Amit (2013). Textbook of endodontics. New Delhi ; London : Jaypee Brothers Medical Publishers. pp. 74–78. ISBN 9789350909522.
- ↑ Cohen's pathways of the pulp. Hargreaves, Kenneth M.,, Berman, Louis H.,, Rotstein, Ilan, (Eleventh ed.). St. Louis, Mo. ISBN 9780323096355. OCLC 931533556.
- 1 2 3 4 Hedge, Jayshree (2008). Prep Manual for Undergraduates: Endodontics. India: Reed Elsevier India Private Limited. p. 29. ISBN 978-81-312-1056-7.
- 1 2 3 4 5 6 7 "Endodontic Diagnosis" (PDF). American Association of Endodontics. Retrieved 14 March 2018.
- 1 2 3 4 5 "Antibiotic use for irreversible pulpitis". doi:10.1002/14651858.CD004969.pub4.
- ↑ http://www.animated-teeth.com/root_canal/t1_root_canal.htm
External links
- An overview of the dental pulp: its functions and responses to injury, C Yu, PV Abbott, Australian Dental Journal Supplement 2007;52:(1 Suppl):S4-S16 at https://web.archive.org/web/20160304023719/http://www.ada.org.au/app_cmslib/media/lib/0704/m70470_v1_633112728503963750.pdf
- Guideline on Pulp Therapy for Primary and Immature Permanent Teeth, REFERENCE MANUAL V 34 / NO 6 12 / 13, 2009, American Academy of Pediatric Dentistry at http://www.aapd.org/media/Policies_Guidelines/G_Pulp.pdf