Barbiturate overdose
| Barbiturate overdose | |
|---|---|
| Synonyms | Barbiturate poisoning, barbiturate toxicity |
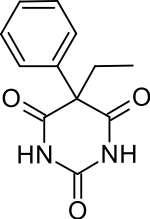 | |
| Molecular diagram of phenobarbital | |
| Specialty | Emergency medicine |
| Symptoms | Decreased breathing, decreased level of consciousness[1] |
| Complications | Noncardiogenic pulmonary edema[2] |
| Duration | 6-12 hours[2] |
| Causes | Accidental, suicide[3] |
| Diagnostic method | Blood or urine tests[4] |
| Treatment | Breathing support, activated charcoal[5][6] |
| Frequency | Uncommon[7] |
Barbiturate overdose is poisoning due to excessive doses of barbiturates.[8] Symptoms typically include difficulty thinking, poor coordination, decreased level of consciousness, and a decreased effort to breathe (respiratory depression).[1] Complications of overdose can include noncardiogenic pulmonary edema.[2] If death occurs this is typically due to a lack of breathing.[3]
Barbiturate overdose may occur by accident or purposefully in an attempt to cause death.[3] The toxic effects are additive to those of alcohol and benzodiazepines.[3] The lethal dose varies with a person's tolerance and how the drug is taken.[3] The effects of barbiturates occur via the GABA neurotransmitter.[2] Exposure may be verified by testing the urine or blood.[4]
Treatment involves supporting a person's breathing and blood pressure.[2][5] While there is no antidote, activated charcoal may be useful.[5][6] Multiple doses of charcoal may be required.[7] Hemodialysis may occasionally be considered.[6] Urine alkalinisation has not been found to be useful.[6] While once a common cause of overdose, barbiturates are now a rare cause.[7]
Mechanism
Barbiturates increase the time that the chloride pore of the GABAA receptor is opened for, thereby increasing the efficacy of GABA. This is as opposed to benzodiazepines which increase the frequency that the chloride pore is opened, thereby increasing GABA's potency.[9]
Treatment
The treatment of barbiturate abuse or overdose is generally supportive. The amount of support required depends on the person's symptoms. If the patient is drowsy but awake and can swallow and breathe without difficulty, the treatment can be as simple as monitoring the person closely. If the person is not breathing, it may involve mechanical ventilation until the drug has worn off.
Supportive treatment often includes the following:
- Activated charcoal may be given via nasogastric tube.
- Intravenous administration of saline, naloxone, thiamine, and/or glucose.
- Intubation and bemegride, or a hand-breather where these are not available until the patient can breathe under their own power.
- Observation in the Emergency Department for a number of hours or admission to the hospital for several days of observation if symptoms are severe.
- Advise the patient about drug misuse or refer for psychiatric consult.
Notable cases
In famous cases, Marilyn Monroe, Dalida,[10][11] Judy Garland, Chester Morris, George Sanders, Pier Angeli, Jimi Hendrix, Scott Newman, Brian Epstein, Alan Wilson, Scotty Beckett, Edie Sedgwick, Dominick Elwes and Carole Landis died from a barbiturate overdose.
See also
References
- 1 2 Weaver, MF (3 September 2015). "Prescription Sedative Misuse and Abuse". The Yale journal of biology and medicine. 88 (3): 247–56. PMC 4553644. PMID 26339207.
- 1 2 3 4 5 Marx, John A. Marx (2014). "165". Rosen's emergency medicine : concepts and clinical practice (8th ed.). Philadelphia, PA: Elsevier/Saunders. pp. Sedative Hypnotics. ISBN 1455706051.
- 1 2 3 4 5 Sadock, Benjamin J.; Sadock, Virginia A. (2008). Kaplan & Sadock's Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins. p. 149. ISBN 9780781787468. Archived from the original on 2016-11-04.
- 1 2 Baren, Jill M. (2008). Pediatric Emergency Medicine. Elsevier Health Sciences. p. 955. ISBN 1416000879. Archived from the original on 2016-11-04.
- 1 2 3 Carroll, Robert G. (2010). Problem-based Physiology. Elsevier Health Sciences. p. 99. ISBN 1416042172. Archived from the original on 2016-11-04.
- 1 2 3 4 Roberts, DM; Buckley, NA (January 2011). "Enhanced elimination in acute barbiturate poisoning - a systematic review". Clinical Toxicology. 49 (1): 2–12. doi:10.3109/15563650.2010.550582. PMID 21288146.
- 1 2 3 Müller, D; Desel, H (October 2013). "Common causes of poisoning: etiology, diagnosis and treatment". Deutsches Arzteblatt international. 110 (41): 690–9, quiz 700. doi:10.3238/arztebl.2013.0690. PMC 3813891. PMID 24194796.
- ↑ Publishing, Bloomsbury (2009). Dictionary of Medical Terms. Bloomsbury Publishing. p. 37. ISBN 9781408102091. Archived from the original on 2016-11-04.
- ↑ Lafferty, KA; Bonhomme, K; Kopinski, P; Lee, DC; Abdel-Kariem, R (14 January 2017). Tarabar, A; VanDeVoort, JT; Burns, MJ, ed. "Barbiturate Toxicity: Pathophysiology". eMedicine. New York, USA: WebMD. Archived from the original on 26 August 2017. Retrieved 26 August 2017.
- ↑ "Dalida ,". New York Times. 5 May 1987. Archived from the original on 26 May 2012. Retrieved 28 February 2008.
- ↑ Simmonds, Jeremy (2008). v. Chicago Review Press. p. 225. ISBN 1-55652-754-3. Archived from the original on 2016-05-18.
External links
| Classification | |
|---|---|
| External resources |